Empirical Examination of Current Depression Categories in a Population-Based Study: Symptoms, Course, and Risk Factors
Abstract
OBJECTIVE: Research studies on the validity of current diagnostic and subthreshold categories of depression that use a population-based follow-up design are rare. The authors examined the validity and utility of four current depression categories by examining subject transition between categories and the symptoms, course, and risk factors of each. METHOD: A general population sample of 1,920 adults from the Baltimore Epidemiologic Catchment Area 13-year follow-up study were examined. Data on diagnoses, symptoms, course, and risk factors were collected by using the National Institute of Mental Health Diagnostic Interview Schedule, the Life Chart Interview, and an office visit. Polychotomous regression was used to examine the heterogeneity of four diagnostic categories: major depressive disorder, depressive syndrome, dysthymia, and a comorbid depression condition (major depressive disorder and dysthymia). RESULTS: Transitions between the four depression categories occurred over the 13 years. Symptom profiles for the four categories were parallel but differed in severity. Course characteristics among the four categories slightly differed. Risk factor profiles showed significant differences. Family history was associated with both depressive syndrome and major depressive disorder. Stressful life events were most strongly associated with depressive syndrome. Female gender was most strongly associated with the comorbid depression category. CONCLUSIONS: The evidence suggests that except for dysthymia, the depression categories are genetically homogeneous and environmentally heterogeneous. Stress is associated with mild depression, and gender is associated with severe depression. The apparent familial transmission of the subthreshold entity, depressive syndrome, needs further investigation.
Lack of consensus as to the heterogeneity of depression is reflected in the evolving diagnostic categories of depressive disorders. Criteria for existing diagnostic categories differ depending on the particular version, and new categories such as minor depressive disorder have been included. For example, the minimal number of symptom groups required for a diagnosis of major depressive disorder changed from DSM-III to DSM-III-R, and distress or impairment caused by symptoms is a new requirement in DSM-IV. There is also a growing interest in subthreshold depression, a classification that requires fewer symptoms than major depressive disorder for diagnosis. The differentiation of dysthymic disorder from major depressive disorder is still an area of intense research (1). The concept of “double depression,” which captures individuals with both major depressive and dysthymic episodes in specific temporal fashion, poses the question as to whether this classification is a comorbid condition or a separate entity (2).
Studies on the validity of different depressive disorders have shown inconclusive results. Attempts to distinguish different diagnostic categories have been made by examining symptoms, course, or risk factors. A study by Wells et al. (3) showed that initial depression severity and level of functional status accounted for more of the variance in outcomes than did type of depressive disorder. A comparison of symptoms among cases of major depressive disorder and dysthymic disorder revealed that symptom presentation did not distinguish clearly between the diagnostic groups (4). The findings by Romanoski et al. (5), which were based on the 1981 psychiatric assessments of the Baltimore Epidemiologic Catchment Area (ECA) sample, suggested that risk factors differed between the subjects with major depressive disorder and those with nonmajor depression. However, the diagnosis of nonmajor depression comprised several potentially heterogeneous disorders.
Studies have been conducted to examine the diagnostic validity of the distinction between dysthymia and major depressive disorder (1, 2, 6), two disorders with a very high rate of comorbidity (7). The condition of an index episode of major depressive disorder continuous with a preexisting dysthymia and without an intervening period of euthymia of at least 8 weeks has been coded “double depression” (2). The poor prognoses for double depressive disorders and dysthymic disorders have been recognized (2), but there is little conclusive evidence that dysthymia is a separate disease entity from major depressive disorder (6). In addition, evidence from the Medical Outcomes Study (3) suggests that the outcome for minor depression may be even worse than that for major depressive disorder.
The heterogeneity of minor depression and its separate role from major depressive disorder also have drawn increasing research attention. Family studies suggest that there is a higher risk of minor depression among relatives of probands with major depressive disorder (8). Epidemiologic evidence suggests that major depressive disorder is more often an exacerbation of a chronic mood disturbance with roots in longstanding vulnerability factors, while in later life minor depression is more often a reaction to commonly experienced stresses (9). Some researchers have suggested that minor depression is a heterogeneous disorder because some cases of minor depression progress into major depressive disorder while others do not (10, 11).
This study uses a prospective and population-based sample to assess the discriminant validity and utility of four subcategories of depression: major depressive disorder, depressive syndrome, dysthymia, and comorbid depression (operationally defined here as meeting criteria for both major depressive disorder and dysthymia). The heterogeneity of these depression categories can be probed from three perspectives: symptoms, natural course, and risk factors.
METHOD
Sample
The ECA study was a series of epidemiologic surveys of the general household population conducted from 1980 to 1983 by collaborators at five sites in the United States (12, 13). During 1993–1996, the Baltimore ECA follow-up study interviewed 1,920 adults from the original Baltimore sample of 3,481. Nonresponse was due to mortality, sample loss, or subject refusal. The nonsurvivors were more likely to be older, male, white, less educated, widowed, and unemployed. Subjects lost to follow-up were more likely to be younger, nonwhite, divorced or separated, less educated, and unemployed. Subjects who refused participation were more likely to be white and less educated, but refusal was not associated with baseline psychopathology. Since 24.0% (N=835) of the cohort died, the 1,920 subjects represented 72.6% of survivors (14). The demographic composition of the follow-up cohort was comparable to that of the original sample in gender and race, but the follow-up group was older and more educated. The follow-up sample was primarily female (63.0%, N=1,209) and Caucasian (67.0%, N=1,286) and ranged in age from 27 to 96 years (median age=48 years) (15). Depression predicts mortality (16), but in this sample the effect was not statistically significant. Sample attrition was not associated with depression (14). After subjects with missing diagnostic information were excluded, 1,856 subjects from the 1993–1996 follow-up were included in the analyses. Subjects signed statements of informed consent in accordance with procedures of the Johns Hopkins School of Public Health Human Subjects Committee.
Symptoms and Diagnoses
The National Institute of Mental Health Diagnostic Interview Schedule (DIS) (17) was used to assess the diagnostic elements, including symptoms, their severity and frequency over time, and whether or not the symptoms were caused by physical illness or injury, use of drugs or alcohol, or the presence of another psychiatric disorder. Several questions targeted at different symptoms were asked for each of the nine depressive symptom groups in the diagnostic criteria. The presence of each symptom in the lifetime and during the worst episode as well as temporal clustering with other symptoms were clarified.
The diagnoses of major depressive disorder and dysthymia were generated from the algorithm based on DSM-III-R criteria. Depressive syndrome was defined by the statement “have had a period of 2 weeks or longer when several (three or more) depressive symptoms occur together including dysphoria or anhedonia” and excluded individuals who met criteria for major depressive disorder (18). Finally, the comorbid depression group was defined as “meeting criteria for lifetime diagnoses of both major depressive disorder and dysthymia.”
Course Characteristics
Course descriptors were defined operationally following the temporal sequence in disease development and progression. Age at onset was defined as the age in years when the first depressive episode occurred. Depressive episode was defined as a clustering of at least three depressive symptoms, including dysphoria or loss of interest, during a period of 2 weeks or longer. We used the onset age of the first depressive episode as a standard comparison across disorder categories, including the comorbid depression category, which had potentially two different onsets. Prodrome length for depressive syndrome was the duration in years between the onset of the first depressive symptom to the onset of the depressive episode. Number of depressive episodes was the number of lifetime depressive episodes, which indicated the fluctuation of depressive psychopathology over the lifetime.
Impairment was coded present when subjects reported any depression-related interference with working or everyday activities or reported taking medication more than once or being hospitalized for the problem. Depression is known for psychiatric comorbidities, and there is still ongoing debate on the distinction between anxiety and depression (19). Therefore, we also studied how often each of the four depression categories presented comorbidly with other psychiatric disorders as part of our effort to compare the disease course. Lifetime anxiety disorder comorbidity was defined as meeting DSM-III-R criteria for at least one of the anxiety disorders (phobia, generalized anxiety disorder, panic disorder, obsessive-compulsive disorder) in addition to depression. Lifetime alcohol- or substance-related disorder comorbidity was defined as meeting DSM-III-R criteria for abuse of or dependence on alcohol, cocaine, hallucinogens, marijuana, sedatives, stimulants, or tranquilizers in addition to depression. All these course characteristics were cumulative lifetime measures from all available interviews.
Risk Factors
Family history was assessed in the clinical reappraisal of 810 Baltimore ECA subjects in 1981 (20) and at the wave 2 interview in 1982 as well as during an office visit interview of 349 subjects in 1993–1996 (21). A positive family history of depression was defined as any first- or second-degree relatives with depression.
Information on stressful life events was collected from administering the DIS at wave 1, wave 2, and wave 3 assessments. The assessed events included separation, divorce, widowhood, life-threatening illnesses, traumatic events, death of loved one(s), children moving out, retirement, losing job, and breakup of love relationships or important friendships. An addition to the interview for the wave 3 follow-up addressed the problem of deterioration of recall with time through a new standardized instrument called the Life Chart Interview (22). The Life Chart Interview generates age- and calendar-linked personal memory cues for the respondent at the beginning of the interview by means of an interactive visually oriented life calendar that focuses the respondent’s attention on a designated time period. A dichotomous variable to indicate the presence or absence of one or more stressful life events before the onset of the first DIS depressive episode was created. Those who reported any of the above events and also required at least some time for adjustment during the 1 year before onset of the first depressive episode were coded positive for prior stressful life events during the 1 year before onset.
Statistical Analysis
Any overall differences in depressive symptoms, course, and risk factors among the four groups were examined by means of analyses of variance (ANOVAs) for continuous variables and chi-square tests for categorical variables. Nonparametric Kruskal-Wallis tests were used for nonnormally distributed continuous measures. Differences between any two groups were compared by means of two-sample t tests for continuous variables and z tests for categorical variables. Nonparametric Mann-Whitney tests were used for nonnormally distributed continuous measures. We used the Bonferroni method to adjust for type I errors due to multiple comparisons. Both the actual p values and the Bonferroni p values are reported.
We first examined the univariate associations between a set of hypothesized risk factors (female gender, family history of depression, and stressful life events before the onset of the first episode) and each of the four depression categories. The reference group was composed of subjects without major depressive disorder, depressive syndrome, or dysthymia in their lifetime. Next, we used logistic regression models to examine the multivariate associations between hypothesized risk factors and each of the four disorder categories. The interactions between the covariates were also examined. In order to compare the risk factor association profiles across different categories, polychotomous logistic regression models were used to test the homogeneity among these parallel odds ratios. For example, we were able to compare the associations with female gender between the major depressive disorder and the dysthymia categories in the polychotomous regression model. The polychotomous logistic regression model is the natural extension of the binary logistic regression model and can be used to carry out simultaneous analyses of multiple response types (23). A homogeneity z test was used to test whether two parallel odds ratios for two different response types differed.
RESULTS
Sample Characteristics
Individuals who met criteria for each of the three depression categories (major depressive disorder, dysthymia, and depressive syndrome) were identified first, which resulted in the following lifetime prevalence rates: major depressive disorder: 9.8% (95% confidence interval [CI]=8.2%–11.4%); depressive syndrome: 16.0% (95% CI=14.2%–17.8%); dysthymia: 7.3% (95% CI=6.1%–8.5%). For the purpose of examination among different categories, individuals were assigned to one of four mutually exclusive lifetime categories: major depressive disorder (5.4%, N=100), depressive syndrome (12.0%, N=223), dysthymia (3.7%, N=68), and comorbid depression (major depressive disorder and dysthymia; 2.8%, N=53).
Subject Transition Between Depression Diagnostic Categories
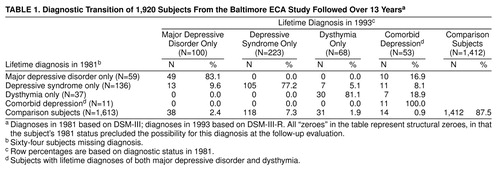
We examined the change of lifetime diagnostic status by cross-tabulating lifetime diagnoses assessed in the wave 1 (1981) interview and lifetime diagnoses summarized from assessments in three waves (1981, 1982, 1993–1996). As seen in table 1, about 17% of the 59 subjects with major depressive disorder in 1981 developed comorbid dysthymia during the follow-up. About 10% of the 136 subjects with depressive syndrome in 1981 developed major depressive disorder; 5% developed dysthymia; and 8% developed comorbid major depressive disorder and dysthymia. About 19% of the 37 dysthymia subjects in 1981 developed comorbid major depressive disorder.
Symptom Heterogeneity
The proportions of individuals in each of the four categories reporting depressive symptoms during their worst episodes are compared visually in figure 1 and statistically by using polychotomous regression models with homogeneity z tests. Proportions of subjects with depressive syndrome were lower than those of subjects with major depressive disorder for all nine symptom groups. The odds ratio of reporting each symptom group in the major depressive disorder category was significantly higher than it was for the depressive syndrome category (e.g., from the polychotomous regression model for depressed mood, homogeneity z=2.4, N=1,856, p=0.02). For all symptom groups except “feeling worthless,” subjects with dysthymia were significantly less likely than subjects with major depressive disorder to report experiencing the symptoms. Subjects with comorbid depression had significantly higher proportions reporting symptoms of feeling tired, feeling worthless, and suicidal thought/behavior than those with major depressive disorder. To summarize, the associations between each category and the symptom profiles were parallel but significantly differed in the strength of associations (comorbid depression greater than major depressive disorder greater than dysthymia and depressive syndrome), with a few exceptions in the comparison of the major depressive disorder and the comorbid depression categories.
Course Heterogeneity
We compared the means of three continuous course variables (age at onset of first depressive episode, length of prodrome, number of depressive episodes) among the four depression diagnostic categories (figure 2 shows the distributions of age at first depressive episode). The age-at-onset distributions were similar for the major depressive disorder and depressive syndrome categories. There was more variation in the onset distribution for the dysthymia category, and the age at onset was earlier for the comorbid depression category. Statistical tests for an overall difference across the four depressive categories suggested significant differences in age at onset (Kruskal-Wallis χ2=8.84, df=3, p=0.03) and number of episodes (Kruskal-Wallis χ2=13.2, df=3, p=0.004), but not in length of prodrome. Next, examination of six paired comparisons by means of Mann-Whitney tests revealed that the comorbid depression category had an earlier onset than the other three categories (versus depressive syndrome: U=3,584, N=236, p=0.004; versus major depressive disorder: U=1,971.5, N=150, p=0.02; versus dysthymia: U=899, N=98, p=0.04). If we used the Bonferroni method to adjust for multiple comparisons by multiplying the above p values by six, only the difference between the comorbid depression and the depressive syndrome categories remained significant.
Next, examination of six paired comparisons again by means of Mann-Whitney tests showed that subjects in the comorbid depression category experienced more episodes than those with major depressive disorder and those with depressive syndrome (versus major depressive disorder: U=1,916, N=148, p=0.03; versus depressive syndrome: U=2,711.5, N=213, p<0.001). If we used the Bonferroni method to adjust for multiple comparisons by multiplying the above p values by six, only the difference between the comorbid depression and the depressive syndrome categories remained significant.
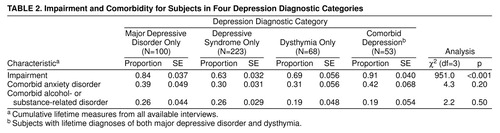
The proportion of subjects reporting dichotomous course variables (impairment, comorbid anxiety disorder, or comorbid alcohol- or substance-related disorder) are compared in table 2. The chi-square test that compared all four categories suggested an overall difference in the proportion reporting impairment but not in subjects with co-occurring conditions. Subjects in the comorbid depression category reported the highest rate of depression-related impairment (91%), whereas those in the depressive syndrome category reported the lowest rate (63%). Examination of six paired comparisons by means of z tests showed that the impairment rate was higher in the major depressive disorder and comorbid depression categories but lower in the depressive syndrome and dysthymia categories (major depressive disorder versus depressive syndrome: z=4.30, N=323, p<0.00006; major depressive disorder versus dysthymia: z=2.22, N=168, p=0.03; comorbid depression versus depressive syndrome: z=5.36, N=276, p<0.00006; comorbid depression versus dysthymia: z=3.12, N=121, p=0.002). If we used the Bonferroni method to adjust for multiple comparisons by multiplying the above p values by six, all differences except that between the major depressive disorder and the dysthymia categories remained significant.
Risk Factor Heterogeneity Among Four Categories
Results of logistic regressions that compared each of the four depression categories and the reference group are summarized in table 3. In the univariate regression model, subjects with depressive syndrome, dysthymia, and comorbid depression—but not major depressive disorder—had a significantly higher likelihood of being female; the odds ratio for female gender was much higher in the comorbid depression category than it was in the other three categories. The homogeneity z test of odds ratios between the major depressive disorder and comorbid depression categories indicated that the association between female gender and comorbid depression was significantly stronger than that of female gender and major depressive disorder (z=–2.8, N=1,856, p=0.005). Family history was associated with all four diagnostic categories, but the odds ratio for the dysthymia subjects was lower than those of the other three groups. The homogeneity z test of odds ratios between the major depressive disorder and dysthymia categories indicated that the association between family history and major depressive disorder was significantly stronger than that of family history and dysthymia (z=2.6, N=1,594, p=0.009). Stressful life events had a significantly higher likelihood of occurring with major depressive disorder and depressive syndrome but not with dysthymia or comorbid depression.
In the multivariate regression model, the odds ratio for female gender was significant only for the comorbid depression category. The odds ratio for family history of depressive disorder was significantly associated with all categories except dysthymia. Stressful life events were a significant predictor for major depressive disorder and depressive syndrome but not for dysthymia or comorbid depression. A homogeneity z test comparison of odds ratios between the major depressive disorder and the comorbid depression categories indicated a significantly stronger association between female gender and comorbid depression than between female gender and major depressive disorder (z=–2.02, N=1,160, p=0.04).
Both major depressive disorder and depressive syndrome were associated with family history of depression and stressful life events before onset. Yet, for the subjects with major depressive disorder, family history was a stronger risk factor than a stressful life event; for depressive syndrome, a stressful life event was a stronger risk factor than family history. For subjects with comorbid depression, family history was a prominent risk factor in addition to female gender. Dysthymia was the only category not significantly associated with any of the examined risk factors. There were no significant interactions between the examined risk factors in any of the four categories.
DISCUSSION
There was a substantial degree of transition among these depression diagnostic categories over time. Symptoms of a substantial proportion of subjects with dysthymia have only intensified with time. The course of some individuals with depressive syndrome or major depressive disorder has become more chronic. The transition from depressive syndrome to major depression is consistent with what has been reported earlier by Broadhead and colleagues (24). There have been some discrepancies in subject reports of psychopathology in multiple waves of assessments (15), so we took information from three waves to establish the lifetime diagnoses in wave 3.
The profiles of depressive symptoms were parallel among the four depression diagnostic categories. Proportionally more subjects with comorbid depression or major depressive disorder reported all depression symptom groups than did those with dysthymia or depressive syndrome. The depressive episode was more severe in subjects with comorbid depression than for those with major depressive disorder, especially when reporting symptoms that may be considered more severe in nature, such as suicidality and worthlessness. Individuals with dysthymia presented symptom profiles similar to those with depressive syndrome.
The four depression diagnostic categories were similar in course characteristics except that the earlier onset for comorbid depression might explain its more severe and recurrent nature and the higher proportion of subjects reporting impairment. Our finding of earlier onset for subjects with comorbid depression is consistent with the study by Sorenson et al. (25). The high rates of impairment associated with all four categories including depressive syndrome are consistent with existing evidence. Wells et al. (3) reported that depressive symptoms in the absence of disorder are associated with limitations in six dimensions of patient well-being and functioning (physical functioning, role functioning, social functioning, number of bed days, current health, and being free of pain) when compared with patients with no chronic conditions in a general medical outpatient sample. Judd et al. (26) found significantly more subjects with depressive symptoms reported high levels of household strain, social irritability, and financial strain as well as limitations in physical or job functioning, restricted activity days, bed days, and poor health status than did subjects without disorder. The lifetime prevalence of major depressive disorder is 5.4%, and in our study 84% of the subjects with major depressive disorder reported impairment. However, the lifetime prevalence of depressive syndrome is 12%, and in our study 63% of the depressive symptom subjects reported impairment. Therefore, we found that more people are impaired by minor depression than by major depressive disorder. This has also been found in prior studies (3, 26). The combination of a higher prevalence and associated impairment of subthreshold or subsyndromal depressive symptoms emphasizes its clinical and public health importance. It has also been demonstrated that individuals with minor depression were associated with 51% more disability days in the community than persons with major depression (24).
We used the course characteristic onset age for first depressive episode for a standardized comparison of the four depression categories. In this study, the median onset age for subjects with dysthymia was 25 years, while the median onset age for depressive episode was 33 years. Contrary to conclusions based on clinical samples (25), only a little more than half of the subjects reporting the presence of depressive episode had more than one episode in their lifetime.
Risk factor profiles differed from category to category, and there were linkages between specific risk factors and certain symptom or course characteristics. The association with family history of depressive disorder in episodic forms of depression (major depressive disorder, depressive syndrome, comorbid depression) was strong regardless of symptom severity. The association with stressful life events was stronger for the mild episodic form of depression (depressive syndrome) than it was for major depressive disorder. There was a prominent association between female gender and a more chronic course or more severe symptoms (the comorbid depression category). We used the “stressful life events before the onset of the first depressive episode” as a standardized comparison across disorder categories, in spite of the fact that for the comorbid depression category there are potentially two different onsets. The possibility that different roles might be played by the same risk factor such as stress before the first episodes of different types (depressive versus dysthymic) remain to be investigated.
Not very much is known about the risk factors for depressive syndrome. The existing evidence shows that family history of major depressive disorders and certain type of stressful life events were associated with minor depression (9), and the association with female gender is still unclear (10). Our evidence suggests that family history and prior stressful life events, but not female gender, are significant risk factors for depressive syndrome.
The finding that female gender is not a significant risk factor for major depressive disorder has not been reported in earlier studies. We also examined the risk factor profiles for three inclusive categories (all subjects with major depressive disorder, all subjects with depressive syndrome, all subjects with dysthymia), since the four examined categories were mutually exclusive, and the “major depressive disorder” only group did not include those who met criteria for both major depressive disorder and dysthymia. The odds ratio, after adjusting for family history and stressful life events, for female gender among all subjects with major depressive disorder relative to comparison subjects was 3.4 (95% CI=1.5–7.8). In other words, when all major depressive individuals are considered as a group, female gender is more prominent than it is in the group with major depressive disorder only. It is possible that the diagnostic switch between the first and final interviews is captured in the longitudinal study and that the course has been different for female subjects, since more of them have become comorbid, thus changing their diagnostic category and removing them from the major depressive disorder category, while strengthening the association of gender as a risk factor within the comorbid group.
The DIS instrument does not generate the diagnoses of minor depression or double depression. The “depressive syndrome” we used in this study is similar to the category of minor depression (18). According to current diagnostic concepts, the comorbid depression group of this study consisted of individuals with 1) double depression as defined by Keller and Lavori (2), or 2) chronic major depressive disorder, or 3) nonconcurrent comorbidity of major depressive disorder and dysthymic disorder. Future research is needed to examine the differences among them. Yet the comorbid depression group represented individuals who were experiencing both an intense and prolonged depressive episode. A limitation of studying a large population sample is the validity of measurements. This study would have been stronger if there were more detailed measures on depression-related impairment. The associations between depressive disorders and the potential risk factors, including family history and stress, could be clarified in future studies with prospectively refined measures. In addition, although three examined risk factors in this study represented potential hormonal, social, genetic, familial, or environmental etiologies for depression, there are still many among the whole spectrum of hypothesized risk factors for depression that were not included.
Since the subthreshold entity, depressive syndrome, is associated with similar etiologic profiles to major depressive disorder and a substantial rate of impairment, we highlight the importance of depressive syndrome in genetic and clinical research. In contrast, the dysthymia category was similar to depressive syndrome regarding symptoms but not risk factor profiles. It did not show a strong relationship to any of the examined risk factors. Its value as a distinct nosologic entity appears to be questionable. The comorbid depression category (lifetime major depressive disorder and dysthymia) has a worse course and is associated with female gender and family history but not with stress. Thus, the evidence suggests a genetic homogeneity and an environmental heterogeneity among three different forms of depression: major depressive disorder, depressive syndrome, and a more severe form of major depressive disorder with chronic and unremitting course.
Received Oct. 1, 1998; revisions received July 27 and Aug. 23, 1999; accepted Sept. 28, 1999. From the Departments of Mental Hygiene and Epidemiology, School of Hygiene and Public Health, Johns Hopkins University; and the Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine, Baltimore. Address reprint requests to Dr. Chen, Department of Mental Hygiene, School of Hygiene and Public Health, Johns Hopkins University, 624 North Broadway, Baltimore, MD 21205. Supported by NIMH grant MH-47447.
 |
 |
 |
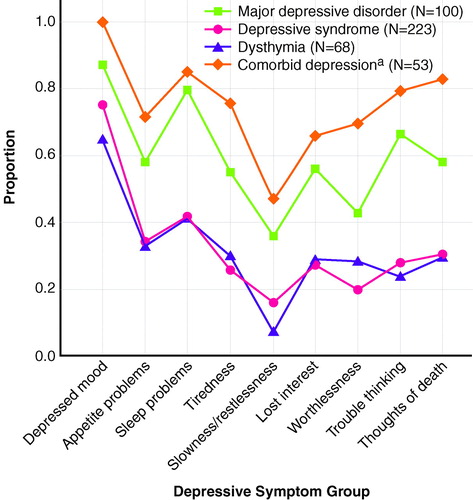
FIGURE 1. Specific Depressive Symptoms During Worst Episodes of Subjects in Four Depression Diagnostic Categories
aSubjects with lifetime diagnoses of both major depressive disorder and dysthymia.
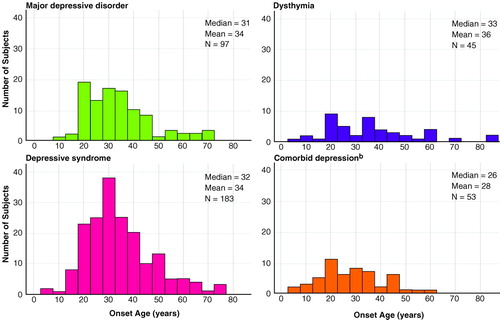
FIGURE 2. Age at First Depressive Episode for Subjects in Four Depression Diagnostic Categoriesa
aTotal numbers for each group are smaller because of missing age-at-onset information.
bSubjects with lifetime diagnoses of both major depressive disorder and dysthymia.
1. Keller MB, Klein DN, Hirschfeld RM, Kocsis JH, McCullough JP, Miller I, First MB, Holzer CP III, Keitner GI, Marin DB, Shea T: Results of the DSM-IV mood disorders field trial. Am J Psychiatry 1995; 152:843–849Link, Google Scholar
2. Keller MB, Lavori PW: Double depression, major depression, and dysthymia: distinct entities or different phases of a single disorder? Psychopharmacol Bull 1984; 20:399–402Google Scholar
3. Wells KB, Burnam MA, Rogers W, Hays R, Camp P: The course of depression in adult outpatients: results from the Medical Outcomes Study. Arch Gen Psychiatry 1992; 49:788–794Crossref, Medline, Google Scholar
4. Spalletta G, Troisi A, Saracco M, Ciani N, Pasini A: Symptom profile, axis II comorbidity and suicidal behaviour in young males with DSM-III-R depressive illnesses. J Affect Disord 1996; 39:141–148Crossref, Medline, Google Scholar
5. Romanoski AJ, Folstein MF, Nestadt G, Chahal R, Merchant A, Brown CH, Gruenberg EM, McHugh PR: The epidemiology of psychiatrist-ascertained depression and DSM-III depressive disorders: results from the Eastern Baltimore Mental Health Survey clinical reappraisal. Psychol Med 1992; 22:629–655Crossref, Medline, Google Scholar
6. Keller MB, Russell CW: Dysthymia, in DSM-IV Sourcebook, vol 2. Edited by Widiger TA, Francis AJ, Pincus HA, Ross R, First MB, Davis WW. Washington, DC, American Psychiatric Association, 1996, pp 21–35Google Scholar
7. Akiskal HS, King D, Rosenthal TL, Robinson D, Scott-Strauss A: Chronic depressions, part 1: clinical and familial characteristics in 137 probands. J Affect Disord 1981; 3:297–315Crossref, Medline, Google Scholar
8. Maier W, Lichtermann D, Minges J, Heun R, Hallmayer J: The risk of minor depression in families of probands with major depression: sex differences and familiarity. Eur Arch Psychiatry Clin Neurosci 1992; 242:89–92Crossref, Medline, Google Scholar
9. Beekman AT, Deeg DJ, van Tilburg T, Smit JH, Hooijer C, van Tilburg W: Major and minor depression in later life: a study of prevalence and risk factors. J Affect Disord 1995; 36:65–75Crossref, Medline, Google Scholar
10. Beck DA, Koenig HG: Minor depression: a review of the literature. Int J Psychiatry Med 1996; 26:177–209Crossref, Medline, Google Scholar
11. Blazer D: Clinical features in depression in old age: a case for minor depression in later life. Current Opinion in Psychiatry 1991; 4:596–599Crossref, Google Scholar
12. Regier DA, Myers JK, Kramer M, Robins LN, Blazer DG, Hough RL, Eaton WW, Locke BZ: The NIMH Epidemiologic Catchment Area program: historical context, major objectives, and study population characteristics. Arch Gen Psychiatry 1984; 41:934–941Crossref, Medline, Google Scholar
13. Robins LN, Regier DA (eds): Psychiatric Disorders in America: The Epidemiological Catchment Area Study. New York, Free Press, 1991, pp 449Google Scholar
14. Badawi MA, Eaton WW, Myllyluoma J, Weimer LG, Gallo J: Psychopathology and attrition in the Baltimore ECA 15-year follow-up 1981–1996. Soc Psychiatry Psychiatr Epidemiol 1999; 34:91–98Crossref, Medline, Google Scholar
15. Eaton WW, Anthony JC, Gallo J, Cai G, Tien A, Romanoski A, Lyketsos C, Chen LS: Natural history of Diagnostic Interview Schedule/DSM-IV major depression: the Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry 1997; 54:993–999Crossref, Medline, Google Scholar
16. Bruce ML, Seeman TE, Merrill SS, Blazer DG: The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health 1994; 84:1796–1799Google Scholar
17. Robins LN, Helzer JE, Croughan J, Ratcliff KS: National Institute of Mental Health Diagnostic Interview Schedule (DIS), in Psychiatric Epidemiology: Assessment, Concepts and Methods. Edited by Mezzich JE, Jorge MR, Salloum IM. Baltimore, Johns Hopkins University Press, 1994Google Scholar
18. Anthony JC, Petronis KR: Suspected risk factors for depression among adults 18–44 years old. Epidemiology 1991; 2:123–132Crossref, Medline, Google Scholar
19. Kendler KS, Heath AC, Martin NG, Eaves LJ: Symptoms of anxiety and symptoms of depression: same genes, different environments? Arch Gen Psychiatry 1987; 44:451–457Google Scholar
20. Anthony JC, Folstein M, Romanoski AJ, Von Korff MR, Nestadt GR, Chahal R, Merchant A, Brown CH, Shapiro S, Kramer M, Gruenberg EM: Comparison of the lay Diagnostic Interview Schedule and a standardized psychiatric diagnosis: experience in eastern Baltimore. Arch Gen Psychiatry 1985; 42:667–675Crossref, Medline, Google Scholar
21. Eaton WW, Anthony JC, Romanoski A, Tien A, Gallo J, Cai G, Neufeld K, Schlaepfer T, Laugharne J, Chen LS: Onset and recovery from panic disorder in the Baltimore Epidemiologic Catchment Area follow-up. Br J Psychiatry 1998; 173:501–507Crossref, Medline, Google Scholar
22. Lyketsos CG, Nestadt G, Cwi J, Heithoff K, Eaton WW: The Life Chart Interview: a standardized method to describe the course of psychopathology. Int J Methods Psychiatr Res 1994; 4:143–155Google Scholar
23. Liang KY, Stewart WF: Polychotomous logistic regression methods for matched case-control studies with multiple case or control groups. Am J Epidemiol 1987; 125:720–730Crossref, Medline, Google Scholar
24. Broadhead WE, Blazer DG, George LK, Tse CK: Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA 1990; 264:2524–2528Google Scholar
25. Sorenson SB, Rutter CM, Aneshensel CS: Depression in the community: an investigation into age of onset. J Consult Clin Psychol 1991; 59:541–546Crossref, Medline, Google Scholar
26. Judd LL, Paulus MP, Wells KB, Rapaport MH: Socioeconomic burden of subsyndromal depressive symptoms and major depression in a sample of the general population. Am J Psychiatry 1996; 153:1411–1417Google Scholar



