Efficacy of Continuation ECT and Antidepressant Drugs Compared to Long-Term Antidepressants Alone in Depressed Patients
Abstract
OBJECTIVE: The purpose of this study was to evaluate the efficacy of continuation ECT in depression. METHOD: The authors used retrospective chart review to identify 29 patients who received continuation ECT plus long-term antidepressant treatment after a positive response to acute treatment with ECT for a depressive episode (continuation ECT group). A retrospective case-controlled approach was used to ascertain a matching group of 29 patients who received long-term antidepressant treatment alone after responding positively to acute ECT (antidepressant-alone group). All 58 patients (46 with unipolar depression, 12 with bipolar disorder) had been chronically depressed before receiving acute ECT. Data from medical records were analyzed by using survival analysis and proportional hazards regression to determine outcome and risk factors. RESULTS: The mean duration of the follow-up period for all patients was 3.9 years (5.4 years for the continuation ECT patients and 2.4 years for the antidepressant-alone patients). Outcome was significantly better in the continuation ECT group. The cumulative probability of surviving without relapse or recurrence at 2 years was 93% for continuation ECT patients and 52% for antidepressant-alone patients. At 5 years, survival declined to 73% for continuation ECT patients, but fell to 18% for antidepressant-alone patients. Mean survival times were 6.9 years for the continuation ECT patients and 2.7 years for the antidepressant-alone patients. CONCLUSIONS: The findings provide strong support for the efficacy of continuation ECT plus long-term antidepressant treatment in preventing relapse and recurrence in chronically depressed patients who have responded to acute treatment with ECT.
The efficacy of ECT is well established for the acute treatment of depression, particularly in patients with very severe symptoms, mood-congruent delusions, prominent suicidality, and inanition and dehydration (1–5). Unfortunately, this population of severely ill patients remains at high risk for relapse and recurrence, even when adequate extended pharmacotherapy is provided (6). The identification of effective continuation and maintenance strategies for these patients is a critical issue in the long-term management of depression.
Continuation therapy is often narrowly defined as treatment that occurs during the several months immediately after resolution of an acute episode of illness, with the primary purpose of relapse prevention (7). Maintenance therapy is sometimes differentiated as a more prolonged course of intervention, extending beyond continuation therapy and used to prevent recurrence of the illness (i.e., a new episode). In practice, the distinction between continuation therapy and maintenance therapy is arbitrary (5); what is important is that continuation therapy of some sort is necessary to prevent the return of depressive symptoms, irrespective of whether ECT or antidepressant medications are used to treat an acute episode of depression (8).
Although the practice of extended and long-term drug therapy for depression has become standard, the use of broadly defined continuation ECT has failed to gain general acceptance (9). Proponents of continuation ECT argue that this approach represents an effective alternative or adjunct to drug treatment in selected patients who are at high risk of relapse. This group includes patients who have demonstrated response of their acute episode to a standard course of ECT and 1) have experienced an acute episode that was refractory to drugs, 2) have relapsed during long-term pharmacological treatment, or 3) have had contraindications to long-term antidepressant or thymoleptic drug treatment (7, 10, 11). The published literature on continuation ECT consists mainly of case reports (12–15), naturalistic studies (8, 16), and retrospective case series (11, 17–20) of patients who clearly obtained benefit from continuation ECT. We are aware of no prospective or randomized studies, and only three reports have included some form of controlled comparison, even if retrospective (11, 16, 18).
The present retrospective case-controlled study was undertaken to evaluate the efficacy of continuation ECT plus long-term antidepressant treatment versus long-term antidepressant treatment alone in a large sample of patients with severe chronic depression treated under naturalistic conditions. Before beginning long-term treatment of any sort, all patients had responded positively to a standard course of ECT given for an acute episode of illness. Both within- and between-subjects comparisons were used, and outcome measures corresponded to those used in previous reports (12). Clinical and demographic factors were evaluated with respect to their ability to predict outcome. On the basis of the published literature, we hypothesized that continuation ECT combined with long-term antidepressant treatment would be superior to standard treatment with long-term antidepressants alone in these severely ill patients.
Method
Patients
To determine patients’ eligibility for the study, we reviewed the charts of all patients who received continuation ECT from April 1985 to July 1999 in the ECT Program at Butler Hospital, a university-affiliated psychiatric facility in Providence, R.I. Continuation ECT patients with a primary DSM-III, DSM-III-R, or DSM-IV axis I diagnosis of either major depression (unipolar) or bipolar I or bipolar II disorder (most recent episode depressed) were enrolled (continuation ECT group). Excluded were continuation ECT patients who 1) had severe concurrent medical illness, 2) had a preexisting nonaffective psychiatric illness, or 3) met criteria for schizoaffective disorder. This protocol was reviewed by the Butler Hospital institutional review board and judged to be exempt from the requirement for written informed consent.
A comparison group consisting of patients given long-term antidepressant treatment alone (antidepressant-alone group) was matched to the continuation ECT group for age, gender, primary axis I diagnosis, age at onset of depression, presence of comorbid psychosis, and year during which the index course of acute ECT was administered. Like the continuation ECT group, all patients in the antidepressant-alone group had had a positive response to acute treatment with ECT. Patients included in the antidepressant-alone group were subjected to the same inclusion/exclusion criteria as the continuation ECT patients. The patients in the antidepressant-alone group had received four to 15 treatments of acute ECT for their depressive episode. After acute ECT, these patients were continued or maintained with antidepressant medications alone, without additional ECT, for prevention of relapse and recurrence.
Additional data on demographic and clinical characteristics were abstracted from all patients’ charts. Additional demographic characteristics included ethnicity, marital status, and employment history. Ancillary clinical characteristics included secondary axis I diagnoses, any axis II diagnoses, bipolar versus unipolar subtype, family history of affective disorder in first-degree relatives, age at onset of depressive symptoms, age at first ECT, age at index ECT, medications administered during the index depressive episode (including number, duration of trials, and doses of antidepressants, neuroleptics, thymoleptics, and anxiolytics), number and duration of hospitalizations, and the use of psychotherapy. Clinical information suggestive of greater severity (psychosis, severe suicidality, and melancholia) (7, 16, 21) was noted. The method of electrode placement (unilateral versus bilateral) and mean seizure duration were determined.
A total of 58 patients were included in the study, 29 in the continuation ECT group and 29 in the antidepressant-alone comparison group. The mean age of the continuation ECT patients at the time of the study was 64.5 years (SD=19.0, range=29–91) and that of the antidepressant-alone patients was 66.1 years (SD=18.7, range=34–96). Both groups were predominantly (>80%) female and appeared similar in terms of socioeconomic background and ethnicity (Table 1).
After the course of acute ECT, 28 (96.6%) of 29 continuation ECT patients and all of the antidepressant-alone patients were managed with antidepressant medications. One continuation ECT patient received no psychotropic medication during the course of continuation ECT. A comparably broad range of agents was used in both groups, including tricyclics (amitriptyline, clomipramine, desipramine, doxepin, imipramine, nortriptyline), heterocyclics (amoxapine, bupropion, venlafaxine), monoamine oxidase inhibitors (phenelzine, tranylcypromine), selective serotonin reuptake inhibitors (sertraline, fluoxetine, paroxetine), and serotonin receptor antagonists (nefazodone, trazodone). Patients with bipolar disorder in both groups received mood stabilizers (carbamazepine, lithium, divalproex), and a similar proportion of psychotic patients in both groups received neuroleptics. No patients with bipolar disorder were maintained with antidepressants without a mood stabilizer. Drug doses were generally in accepted therapeutic ranges and were similar between treatment groups.
ECT Treatment
ECT was administered by using a Mecta SR-1 (Mecta, Portland, Ore.) brief-pulse, constant-current device. ECT duration was considered optimal if the seizure duration (determined by observable tonic-clonic seizure) lasted 30–60 seconds. All ECT was given by a single psychiatrist (M.J.F.), who adjusted the treatment frequency on the basis of the patient’s clinical response. Patients generally received ECT for acute episodes at a rate of two to three treatments/week until a positive clinical response occurred, on the basis of the consensus evaluation of M.J.F. and the referring psychiatrist that the core depressive symptoms necessitating hospital admission were much or very much improved. The decision to institute continuation ECT was similarly based on the clinical consensus of M.J.F. and the referring psychiatrist that medication maintenance alone was unlikely to be effective given the patient’s history of treatment response and most recent clinical presentation. If the patient continued with ECT, treatments generally were delivered weekly for the first month, every 2 weeks for the following month, and then monthly.
Study Design and Methods
This retrospective study evaluated the efficacy of continuation ECT by comparing the outcomes of patients who received this treatment combined with long-term antidepressant treatment (continuation ECT group) with those of matched comparison patients who received long-term antidepressant treatment alone (antidepressant-alone group). Both groups had manifested a positive response to acute treatment with ECT just before entering the period of long-term treatment under study. In addition, patients in the continuation ECT group were included in a mirror-image comparison of their own clinical course during the time period immediately preceding the index episode of illness versus their course afterward.
Acute ECT was defined as a standard course of ECT administered for the acute treatment of an index episode of depression. The index ECT was the first treatment in the course of acute ECT, and it served as the reference point for calculating the major outcome variables and for the beginning of the survival analysis. Continuation ECT was defined as ongoing ECT that was administered after completion of the course of thrice weekly acute ECT, beginning with the administration of ECT on a weekly or less frequent basis.
The four outcome measures of primary interest were the probability of surviving without relapse or recurrence, the time to relapse/recurrence, the frequency of hospitalization quotient, and the hospital day quotient. Probability of survival and time to relapse/recurrence were evaluated by using survival analysis, with relapse/recurrence stringently defined as the reemergence of depressive symptoms of sufficient severity to result in either rehospitalization or a new course of acute ECT. Time was counted in years from the date of the index ECT. Data from patients who did not experience relapse or recurrence during the observation period were censored. The mean duration of the observation period for all patients was 3.9 years (SD=3.1) (for continuation ECT patients, mean=5.4 years, SD=3.1; for antidepressant-alone patients, mean=2.4 years, SD=2.4).
As described elsewhere (12), the frequency of hospitalization quotient and hospital day quotient were used to quantify the clinical history and functional status of each patient. Each variable was computed for the observation period after index ECT and for an equivalent time period preceding the index ECT. The frequency of hospitalization quotient, reflecting the average number of hospital admissions per year, was calculated by dividing the total number of admissions by the number of days in the observation period and multiplying the quotient by 365. The hospital day quotient, reflecting the average number of psychiatric inpatient hospital days, was determined in a similar manner. Both measures were calculated only for patients with an observation period ≥6 months (periods of <6 months would have resulted in artificially inflated quotients).
Statistical Analysis
Comparisons of clinical and demographic characteristics between groups were performed with t tests for continuous variables or contingency tables (chi-square or Fisher’s exact test) for categorical variables. The Kaplan-Meier product-limit method was used to estimate survival curves. Differences between the continuation ECT and antidepressant-alone groups were evaluated by using the Mantel-Cox test. The Cox proportional hazards regression model was used to determine the significance of potential risk factors for relapse/recurrence. All statistical tests were two-tailed, with significance set at p<0.05. Analyses were performed with SPSS, version 6.1 (22).
Results
Patient and Treatment Characteristics
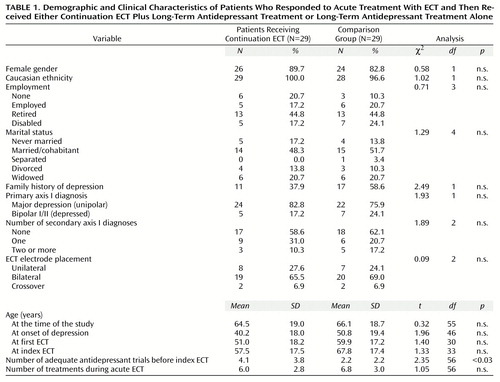
Table 1 presents selected clinical and demographic characteristics of the 58 patients involved in the study. In general, patients in the continuation ECT and antidepressant-alone groups appeared very similar in clinical and demographic features. The single significant difference between groups was the mean number of adequate medication trials before the index ECT. (“Adequacy” was defined as at least 4 weeks of treatment at a dose equal to the manufacturer’s recommended minimum effective dose). Patients in the continuation ECT group had received a mean of 4.1 trials (SD=3.7), whereas the antidepressant-alone patients had received 2.2 trials (SD=2.2) (t=2.36, df=56, p<0.03).
The treatment parameters of the acute ECT given to the continuation ECT and the antidepressant-alone patients were also similar (Table 1). About two-thirds of the patients in each group received bilateral treatment. The mean number of treatments during acute ECT did not differ significantly between groups. The mean seizure duration during the course of acute ECT was nearly identical for both groups, with a pooled mean of 39.7 seconds (SD=10.4). Mean seizure duration for the remainder of treatments after the acute course in the continuation ECT patients was 44.7 seconds (SD=10.5).
Survival Analysis and Risk Factors
Figure 1, depicting the Kaplan-Meier survival curves for continuation ECT and antidepressant-alone patients, shows that outcome was superior for the continuation ECT group. The cumulative probability of surviving without relapse or recurrence at 2 years after index ECT was 93% for continuation ECT patients and 52% for antidepressant-alone patients. At 5 years, survival declined to 73% for continuation ECT patients, but fell to 18% for antidepressant-alone patients. Between 5.5 and 7 years, survival appeared to drop substantially for the continuation ECT patients, although it remained higher than that for antidepressant-alone patients. Mean survival time for continuation ECT patients was 6.9 years (SD=4.4) (95% confidence interval [CI]=5.3–8.5 years), with a median of 6.6 years (SD=3.9) (95% CI=5.1–8.0 years). In contrast, mean survival time for antidepressant-alone patients was 2.7 years (SD=2.5) (95% CI=1.7–3.6 years), with a median of 2.2 years (SD=3.7) (95% CI=0.9–3.6 years).
Potential risk factors for relapse/recurrence, including secondary axis I diagnoses, axis II diagnoses, bipolar versus unipolar subtype, concomitant psychosis or melancholia, prominent suicidality, number of adequate medication trials before index ECT, and adjunctive psychotherapy after acute ECT, were not statistically significant in analyses using proportional hazards regression.
Frequency of Hospitalization Quotient and Hospital Day Quotient
In the continuation ECT group, the frequency of hospitalization quotient was 3.4 (SD=6.6) before the index ECT and 0.8 (SD=1.3) after the index ECT. The hospital day quotient for this group was 57 (SD=112) before the index ECT and 9 (SD=17) after the index ECT. In the antidepressant-alone group, the preindex frequency of hospitalization quotient was 1.2 (SD=1.2) and the postindex frequency of hospitalization quotient was 1.2 (SD=1.0). The preindex hospital day quotient for this group was 17 (SD=15), and the postindex hospital day quotient was 13 (SD=11). There were no statistically significant differences between the continuation ECT group and antidepressant-alone group in the frequency of hospitalization quotient or the hospital day quotient before or after the index ECT or in the difference between the pre- and postindex quotients. Similarly, there were no significant pre- versus postindex differences in the frequency of hospitalization quotient or the hospital day quotient within either group, although both measures showed declines in the continuation ECT group.
Discussion
In this sample of chronically depressed patients responding to a standard course of acute ECT, continuation ECT in conjunction with long-term antidepressant treatment resulted in a marked improvement in clinical outcome. In comparison with rates of survival for patients who received long-term antidepressant treatment alone, rates of survival without relapse or recurrence for patients who received continuation ECT and long-term antidepressant treatment were nearly doubled (93% versus 52%) at 2 years and showed a fourfold increase (73% versus 18%) by 5 years. The mean time to relapse or recurrence more than doubled in the continuation ECT group (6.9 years versus 2.7 years for the antidepressant-alone group).
Comparison patients were closely matched with continuation ECT patients on standard demographic variables (i.e., gender and age), as well as on clinical variables (i.e., primary axis I diagnosis, age at onset of depression, the presence of comorbid psychosis), a treatment variable (i.e., positive response to an index course of ECT), and a temporal variable (i.e., year during which the index course of acute ECT was administered). As a result, patients in both groups appeared similar, as demonstrated by the lack of significant differences between groups across a broad array of clinical and treatment variables. The only significant difference detected was the greater number of previous adequate antidepressant trials in the continuation ECT group, suggesting that the depressive symptoms of these patients were more refractory to pharmacotherapy. However, neither this nor any other identified factor was related to risk of relapse/recurrence.
The follow-up period in the present study lasted more than 5 years for the continuation ECT patients, comparing favorably with the results of previous studies of continuation ECT that have employed a comparison group, none of which extended beyond a 1-year follow-up (11, 16, 18). In this regard, it is notable that survival rates for the continuation ECT patients appeared to deteriorate appreciably between 5.5 and 7 years. It is unclear whether this decline represents a true clinical phenomenon or merely the diminished reliability of the right-hand tail of the survival curve with smaller numbers of at-risk patients (23). For example, although the survival curve in Figure 1 suggests that all patients in both treatment groups eventually relapsed, a marked preponderance of relapses (27 [93.1%] of 29 patients) occurred in the antidepressant-alone group; 11 (37.9%) of the 29 continuation ECT patients were censored before relapse.
In a previous study that also utilized survival analysis, Schwarz et al. (18) detected no significant differences between continuation ECT patients and comparison patients. The lack of difference may have been due partly to the relatively short (6-month) follow-up period employed by those investigators. Surprisingly, hospitalization rates and number of hospital days, as reflected by the frequency of hospitalization quotient and hospital day quotient, respectively, proved insensitive to the effects of continuation ECT in between-groups comparisons in the present study. This finding is in contrast to the significant findings of other investigators who used these or analogous measures (3, 16, 21, 24). Although our findings for the mean frequency of hospitalization quotient and mean hospital day quotient were similar to those previously reported, greater variance in our data precluded findings of statistically significant differences. Significant within-group decreases before and after continuation ECT were also not demonstrable, even though mean changes were in the predicted direction. Again, these results appeared to be due to marked variability and artifacts related to the manner in which the frequency of hospitalization quotient and the hospital day quotient were computed for the time period before the index ECT, even though efforts were made to minimize such artifacts. In any case, these observations underscore the importance of utilizing the more robust survival analytic techniques in subsequent research on continuation ECT.
The present findings must be considered in light of the many caveats that apply to naturalistic, retrospective studies. The sample size, although among the largest yet reported on this topic, was still modest, resulting in limited power to detect possibly meaningful differences in the clinical and demographic characteristics of the two groups. Assignment of patients to treatment groups was not random, and assessments of outcome were not blind or prospectively systematic. Diagnostic and clinical data were not derived from structured instruments and, even though the medical records were relatively complete, detailed information on patients’ clinical and functional status over time was not available. The use of hospitalization or initiation of a new course of acute ECT as measures of relapse/recurrence may have been overly stringent, resulting in an underestimation of the true relapse/recurrence rates. The relatively older age, female preponderance, and Caucasian ethnicity of the study group limit generalizability, as does the fact that all of the patients in this study demonstrated a positive response to a standard course of acute ECT before entering long-term treatment. Finally, even though treatment groups were matched on several clinical and demographic variables of obvious relevance, it is possible that other key clinical or treatment variables that were not subjected to matching or assessment may have differed between groups and may have affected outcome.
It is possible that the more favorable outcome of patients in the continuation ECT group was a result of nonbiological and nonpharmacological aspects of the different follow-up treatments. Patients who received continuation ECT were required to have direct contact with clinicians at least once a month to maintain treatment. If a continuation ECT patient missed an appointment, the ECT staff attempted to contact and reengage the patient. Such active efforts to ensure compliance were probably less vigorous for patients in the antidepressant-alone group. As a result, continuation ECT patients may have benefited both from the psychosocial support of additional contacts with treaters and from an increased likelihood that the biological treatment was actually being taken.
In summary, this study demonstrates that, in chronically depressed patients who have responded to an acute course of ECT, continuation ECT in combination with antidepressants is more effective than antidepressants alone in preventing relapse and recurrence. Prospective research currently underway should provide more definitive data about the magnitude and duration of this effect, as well as about relevant prognostic factors (25). In the meantime, this study supports the continued judicious use of this therapeutic approach in patients who have failed to tolerate or benefit from long-term antidepressant pharmacotherapy.
 |
Received Dec. 22, 2000; revision received June 13, 2000; accepted July 12, 2000. From the Mood Disorders Program, Butler Hospital; and the Department of Psychiatry and Human Behavior, Brown University School of Medicine. Address reprint requests to Dr. Price, Butler Hospital, Department of Psychiatry and Human Behavior, Brown University School of Medicine, 345 Blackstone Blvd., Providence RI 02906; [email protected] (e-mail). Supported in part by a grant from the Department of Psychiatry and Human Behavior, Brown University School of Medicine. The authors thank Jason Siniscalchi, M.S., and Christine A. Richard.
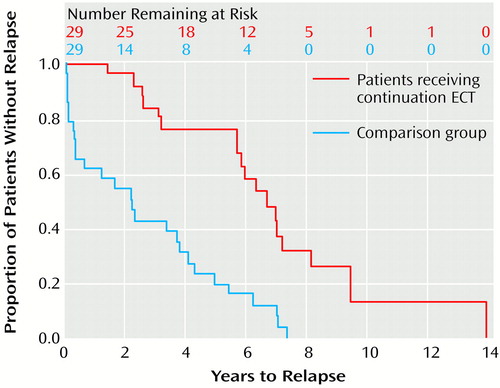
Figure 1. Time to Relapse or Recurrence of Depression in Patients Who Responded to Acute Treatment With ECT and Then Received Either Continuation ECT Plus Long-Term Antidepressant Treatment or Long-Term Antidepressant Treatment Alonea
aMantel-Cox χ2=19.87, df=1, p<0.00005.
1. Martin BA: Electroconvulsive therapy for depression in general psychiatric practice. Psychiatr J Univ Ottawa 1989; 14:413–417Medline, Google Scholar
2. Schatzberg AF: Recent developments in the acute somatic treatment of major depression. J Clin Psychiatry 1992; 53(Mar suppl):20–25Google Scholar
3. Persad E: Electroconvulsive therapy in depression. Can J Psychiatry 1990; 35:175–182Crossref, Medline, Google Scholar
4. Philibert RA, Richards L, Lynch CF, Winokur G: Effect of ECT on mortality and clinical outcome in geriatric unipolar depression. J Clin Psychiatry 1995; 56:390–394Medline, Google Scholar
5. Fink M, Abrams R, Bailine S, Jaffe R: Ambulatory electroconvulsive therapy: report of a task force of the Association for Convulsive Therapy. Convuls Ther 1996; 12:42–55Medline, Google Scholar
6. Grunhaus L, Pande AC, Haskett RF: Full and abbreviated courses of maintenance electroconvulsive therapy. Convuls Ther 1990; 6:130–138Medline, Google Scholar
7. Rabheru K, Persad E: A review of continuation and maintenance electroconvulsive therapy. Can J Psychiatry 1997; 42:476–484Crossref, Medline, Google Scholar
8. Clarke TB, Coffey CE, Hoffman GW Jr, Weiner RD: Continuation therapy for depression using outpatient electroconvulsive therapy. Convuls Ther 1989; 5:330–337Medline, Google Scholar
9. Sackeim HA: Continuation therapy following ECT: directions for future research. Psychopharmacol Bull 1994; 30:501–521Medline, Google Scholar
10. Monroe RR Jr: Maintenance electroconvulsive therapy. Psychiatr Clin North Am 1991; 14:947–960Crossref, Medline, Google Scholar
11. Petrides G, Dhossche D, Fink M, Francis A: Continuation ECT: relapse prevention in affective disorders. Convuls Ther 1994; 10:189–194Medline, Google Scholar
12. Thienhaus OJ, Margletta S, Bennett JA: A study of the clinical efficacy of maintenance ECT. J Clin Psychiatry 1990; 51:141–144Medline, Google Scholar
13. Decina P, Guthrie EB, Sackeim HA, Kahn D, Malitz S: Continuation ECT in the management of relapses of major affective episodes. Acta Psychiatr Scand 1987; 75:559–562Crossref, Medline, Google Scholar
14. Loo H, Galinowski A, de Carvalho W, Bourdel MC, Poirier MF: Use of maintenance ECT for elderly depressed patients (letter). Am J Psychiatry 1991; 148:810Medline, Google Scholar
15. Kramer BA: Maintenance electroconvulsive therapy in clinical practice. Convuls Ther 1990; 6:279–286Medline, Google Scholar
16. Aronson TA, Shukla S, Hoff A: Continuation therapy after ECT for delusional depression: a naturalistic study of prophylactic treatments and relapse. Convulsive Ther 1987; 3:251–259Medline, Google Scholar
17. Stiebel VG: Maintenance electroconvulsive therapy for chronically mentally ill patients: a case series. Psychiatr Serv 1995; 46:265–268Link, Google Scholar
18. Schwarz T, Loewenstein J, Isenberg KE: Maintenance ECT: indications and outcome. Convuls Ther 1995; 11:14–23Medline, Google Scholar
19. Jaffe R, Dubin W, Shoyer B, Roemer R, Sharon D, Lipschutz L: Outpatient electroconvulsive therapy: efficacy and safety. Convuls Ther 1990; 6:231–238Medline, Google Scholar
20. Thornton JE, Mulsant BH, Dealy R, Reynolds CF III: A retrospective study of maintenance electroconvulsive therapy in a university-based psychiatric practice. Convuls Ther 1990; 6:121–129Medline, Google Scholar
21. Olfson M, Marcus S, Sackiem HA, Thompson J, Pincus HA: Use of ECT for the inpatient treatment of recurrent major depression. Am J Psychiatry 1998; 155:22–29Link, Google Scholar
22. SPSS Advanced Statistics User’s Guide 6.1. Chicago, SPSS, 1994Google Scholar
23. Parmar MKB, Machin D: Survival Analysis: A Practical Approach. Chichester, UK, John Wiley & Sons, 1995Google Scholar
24. Vanelle JM, Loo H, Galinowski A, de Carvalho W, Bourdel MC, Brochier P, Bouvet O, Brochier T, Olie JP: Maintenance ECT in intractable manic-depressive disorders. Convuls Ther 1994; 10:195–205Medline, Google Scholar
25. Rudorfer MV, Lebowitz BD: Progress in ECT research (letter). Am J Psychiatry 1999; 156:975Link, Google Scholar



