Cognitive Therapy Versus Medication in Augmentation and Switch Strategies as Second-Step Treatments: A STAR*D Report
Abstract
Objective: The authors compared the effectiveness of cognitive therapy and pharmacotherapy as second-step strategies for outpatients with major depressive disorder who had received inadequate benefit from an initial trial of citalopram. Cognitive therapy was compared with medication augmentation and switch strategies. Method: An equipoise-stratified randomization strategy was used to assign participants to either augmentation of citalopram with cognitive therapy (N=65) or medication (N=117; either sustained-release bupropion [N=56] or buspirone [N=61]) or switch to cognitive therapy (N=36) or another antidepressant (N=86; sertraline [N=27], sustained-release bupropion [N=28], or extended-release venlafaxine [N=31]). Treatment outcomes and the frequency of adverse events were compared. Results: Less than one-third of participants consented to randomization strata that permitted comparison of cognitive therapy and pharmacotherapy. Among participants who were assigned to second-step treatment, those who received cognitive therapy (either alone or in combination with citalopram) had similar response and remission rates to those assigned to medication strategies. For those who continued on citalopram, medication augmentation resulted in significantly more rapid remission than augmentation with cognitive therapy. Among those who discontinued citalopram, there were no significant differences in outcome, although those who switched to a different antidepressant reported significantly more side effects than those who received cognitive therapy alone. Conclusions: After an unsatisfactory response to citalopram, patients who consented to random assignment to either cognitive therapy or alternative pharmacologic strategies had generally comparable outcomes. Pharmacologic augmentation was more rapidly effective than cognitive therapy augmentation of citalopram, whereas switching to cognitive therapy was better tolerated than switching to a different antidepressant.
In controlled studies of acute therapy, less than 50% of patients with major depressive disorder remit during the initial course of antidepressant medication (1 – 3) . For those who do not obtain adequate benefit from an initial course of pharmacotherapy, a wide variety of next-step strategies are available, including switching within and between classes of antidepressants, various augmentation and antidepressant combination strategies, and adding or switching to psychotherapy. Although the efficacy of most of these strategies has been established in randomized controlled trials, few comparative studies are available to help determine which of these options should be considered the preferred next step for patients who do not benefit adequately from an initial course of pharmacotherapy (4 – 6) .
The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) trial is a multicenter, multistage research project funded by the National Institute of Mental Health with the specific purpose of evaluating second-, third-, and fourth-step treatment options for patients with treatment-resistant depression (7 , 8) . In the first treatment step (up to 14 weeks with citalopram alone), approximately one-third of 2,876 participants remitted (9) . In a previous report on second-step treatments (10) , we compared switching from citalopram to alternative second-step antidepressants. There were no significant differences in outcome, with intent-to-treat remission rates ranging from 18% with sertraline (a selective serotonin reuptake inhibitor) to 21% with sustained-release bupropion (a norepinephrine-dopamine reuptake inhibitor) to 25% with extended-release venlafaxine (a serotonin-norepinephrine reuptake inhibitor). A second report compared sustained-release bupropion and buspirone as augmentation agents and found few differences in effectiveness, with both treatments resulting in intent-to-treat remission rates of 30% (11) .
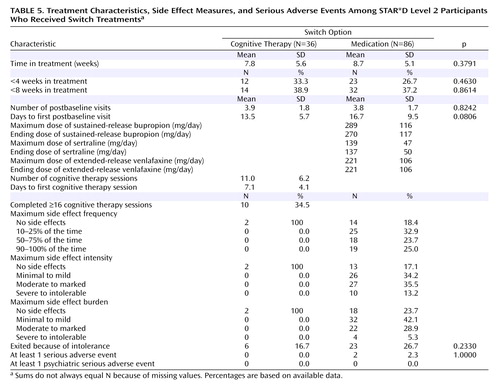
We now report on the utility of cognitive therapy following nonremission with, or intolerance to, citalopram as compared with pharmacologic augmentation and switch strategies. Cognitive therapy is the best-studied form of psychotherapy for acute therapy of major depressive disorder (1 , 12) and has been proposed to be a useful alternative for patients who have not responded to antidepressant medications (13 – 15) . A number of case series and small randomized trials suggest that cognitive therapy may indeed have a role in the management of treatment-resistant depression (16) . The largest study to date (17) found that a form of cognitive behavior therapy was at least as effective when used as a second-step treatment after nonresponse to nefazodone as nefazodone was after nonresponse to the psychotherapy. However, no large-scale randomized studies have evaluated the utility of second-step psychotherapy as compared with medication interventions.
Method
The rationale and design of STAR*D and the specific elements of the cognitive therapy protocol have been detailed elsewhere (7 – 11 , 18) . A summary of the study design is presented below.
Participants
From July 2001 through April 2004, STAR*D enrolled 4,041 outpatients 18 to 75 years of age with a diagnosis of nonpsychotic major depressive disorder from 18 primary care and 23 psychiatric care practice settings across the United States. The diagnosis was clinically established and verified by a checklist based on DSM-IV criteria (19) . Advertising for participants was proscribed to ensure that recruitment would produce a sample representative of patients seen in typical clinical practice. Written informed consent was obtained at study entry and again at enrollment in the second-step treatments.
Inclusion and Exclusion Criteria
STAR*D used broad inclusion and minimal exclusion criteria (7 , 8) to ensure enrollment of a representative study sample of depressed patients seeking treatment in primary care, public mental health, and psychiatric clinics. For example, most forms of comorbidity commonly associated with depression were permitted. The minimum score on the 17-item Hamilton Rating Scale for Depression (HAM-D) (20 , 21) for enrollment was 14, indicating at least a moderate level of depression.
Treatment Protocol and Therapist Training
To ensure rigorous dosing, reflect actual practice, and enhance safety, treatments were not masked to participants or providers. The primary outcome measure was whether participants achieved symptom remission, defined as a score ≤7 on the HAM-D, which was administered by research outcome assessors who were blind to treatment assignments. The protocol recommended that medication treatment visits for all treatment levels be conducted at weeks 0, 2, 4, 6, 9, and 12; however, the visit schedule was flexible, and extra visits could be held if clinically indicated. Depressive symptom severity was assessed at each treatment visit using the clinician-administered version of the 16-item Quick Inventory of Depressive Symptomatology (QIDS-C) (22 – 24) . If participants had a response (defined as a reduction of ≥50% in baseline QIDS-C score) without remission at week 12, they could continue treatment for an additional 2 weeks (14 weeks total) to determine whether remission would occur with additional time. Remission at the clinic visits was defined as a QIDS-C score ≤5. The frequency, intensity, and burden of side effects were monitored with a scale developed for the STAR*D study (25) .
To increase the likelihood that each patient received an adequate course of pharmacotherapy, each STAR*D site had a clinical research coordinator who monitored the progress of each participant, treating physicians received in-service training based on a clinician manual, and a web-based medication monitoring system (26) provided ongoing feedback on patients’ symptom ratings, side effect burden, and treatment regimen (9) . The protocol for the initial course of pharmacotherapy in Level 1 of the STAR*D sequence called for starting citalopram at a dose of 20 mg/day, to be raised to 40 mg/day by week 4. In the case of nonresponse, the dose could be raised to 60 mg/day by week 6. All medication dose recommendations were flexible and could be applied on the basis of clinical judgment informed by scores on the side effect rating scale and the QIDS-C, which were obtained at treatment visits by researchers blind to the patients’ HAM-D score. In the case of intolerable side effects, patients could be withdrawn from Level 1 and advanced to the next treatment level. Patients who did not achieve remission with citalopram were encouraged to move to Level 2 after 12 weeks of citalopram therapy. Those who achieved remission could enter a 12-month naturalistic follow-up phase, and those who had a response without remission were strongly encouraged to proceed to Level 2, although they could also elect to enter the follow-up phase. The flow of patient progress and outcomes from Level 1 to Level 2 is summarized in Figure 1 .
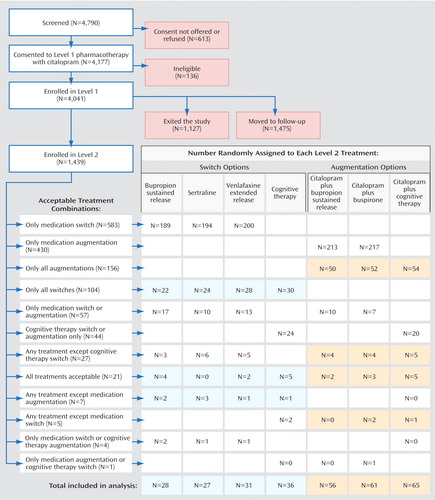
a Shading indicates augmentation or switch strata in which comparison of cognitive therapy and pharmacotherapy was possible; participants who were willing to be randomly assigned to these strata were included in the analysis.
Level 2 Treatments
For patients who did not remit with or tolerate the initial course of citalopram therapy, there were seven possible second-step treatment options. The aims of the study included comparing three augmentation options (adding sustained-release bupropion, buspirone, or cognitive therapy to ongoing citalopram therapy) and four switch strategies (discontinuing citalopram and starting therapy with sertraline, sustained-release bupropion, extended-release venlafaxine, or cognitive therapy).
A novel element of the STAR*D research design, equipoise-stratified randomization (27) , enabled participants—in consultation with their treating physician—to eliminate the possibility of being randomly assigned to treatment strategies they found unacceptable and still remain in the study (thereby mirroring practice). For example, participants could elect to be randomly assigned only to the switch treatments or only the augmentation treatments. They could also accept or decline cognitive therapy within either of these strategies. Or they could exclude all treatments except cognitive therapy alone (as a switch) and cognitive therapy as an augmentation to citalopram. They were subsequently randomly assigned to receive one of the remaining treatment options. In each unique cluster of acceptable treatment options, participants were treated as a stratum in data analyses. The numbers of participants in each stratum provided an approximate ranking of the overall acceptability of both the broader strategies (i.e., augmentation versus switch) and selected treatments.
Of the 4,041 outpatients enrolled in STAR*D Level 1, 1,439 (36%) did not achieve a satisfactory response with citalopram and moved to Level 2. In theory, if all participants had accepted all seven treatment options, on average two out of seven who entered Level 2, or 411 patients (1,439×2/7; 29%) would have been assigned to cognitive therapy. In fact, only 369 participants (26%) accepted one or both cognitive therapy options, and only 147 were assigned to cognitive therapy in Level 2 (including 44 who elected to accept only cognitive therapy options, either alone or as an augmentation to citalopram). Of the 752 patients who were willing to accept an augmentation strategy, 209 (28%) were willing to accept both cognitive therapy and pharmacotherapy among the options; 182 of them were randomly assigned to augmentation of citalopram with either cognitive therapy (N=65) or another medication (N=117). Among the 853 patients who were willing to accept a switch strategy, 132 (16%) were willing to accept both cognitive therapy and pharmacotherapy among the options; 122 of them were randomly assigned to either cognitive therapy alone (N=36) or a second course of pharmacotherapy (N=86). Across the switch and augmentation strata, there was essentially no difference in the acceptability of receiving cognitive therapy among patients treated at primary care sites and in psychiatric settings (25.4% and 25.8%, respectively).
Cognitive Therapy
To ensure that results were generalizable to clinical settings, selection and training of therapists mimicked good clinical practice. Each site’s primary investigator proposed candidate practicing psychotherapists for the study. Candidate therapists submitted summaries of their relevant training and experience and video- or audiotapes of their work with depressed patients. Only one candidate was not accepted for further training, although a number of other candidates did not complete training. Candidate therapists received relevant readings and attended a 2-day workshop conducted by study investigators (E.S.F. and M.E.T.). Training followed the approach described by Shaw (28) , which had been used by the cognitive therapy research group at the University of Pittsburgh for more than 15 years. Before they could participate in the study, therapists had to demonstrate competence (documented by fidelity ratings on the Cognitive Therapy Scale [18] ) in the treatment of one patient who would have been eligible to participate in STAR*D. A total of 44 therapists (30 doctoral-level psychologists, one physician, 11 master’s-level clinical social workers, and two nurses with advanced degrees) completed the certification process; each site had at least two certified therapists. Each therapist treated an average of 2.1 study patients (range=1–6 patients per therapist).
During the study, the psychotherapists’ patients were monitored for adequate therapeutic response using a web-based system that was updated weekly. During monthly group supervision sessions, case conceptualizations, problems implementing cognitive therapy, and treatment strategies were reviewed in detail. If therapists experienced significant problems during the course of the study, additional sessions of individual supervision were provided. No therapists were withdrawn from study participation because of nonadherence to the cognitive therapy model (18) .
The protocol required that cognitive therapy be scheduled twice weekly for weeks 1–4, then once weekly for the remaining 8 weeks (16 sessions total). When twice-weekly sessions were not practicable, the second session could be conducted by telephone. Patients who improved rapidly, as defined by at least three consecutive weeks of remission, could enter follow-up without completing all 16 visits. Patients who had a response but not remission by visit 16 could continue to Level 3 treatment or elect to continue cognitive therapy for an additional four weekly sessions, then twice a month for an additional four sessions and monthly for the final six sessions (research has shown that such patients benefit from continuation-phase cognitive therapy [29] ).
Pharmacotherapy
Pharmacotherapy visits during Level 2 typically lasted 15–20 minutes. Although pharmacotherapists were not prevented from using psychotherapeutic strategies, it is unlikely that much in the way of psychotherapy was provided in these sessions beyond supportive encouragement and psychoeducation. For patients assigned to the augmentation options, the dose of citalopram was typically kept steady, although it could be reduced as needed to alleviate side effects. The target dosing for sustained-release bupropion was 200 mg/day for weeks 1–2, to be raised to 300 mg/day by week 4 and to 400 mg/day as a final dose. Buspirone dosing was to start at 15 mg/day for 1 week, to be raised to 30 mg/day for 1–2 weeks and then to 45 mg/day by week 4, with a maximum dose of 60 mg/day after week 6. For the switch options, citalopram was discontinued at the initial visit, and the new treatment was begun without a tapering or washout period. Sustained-release bupropion dosing was to start at 150 mg/day for 1 week, to be raised to 300 mg/day thereafter, with 400 mg/day as a final dose. Sertraline dosing was to start at 50 mg/day for 1 week, to be raised to 100 mg/day for weeks 3–4, to 150 mg/day for weeks 5–9, and to 200 mg/day for weeks 10–12. The starting dose for extended-release venlafaxine was 37.5 mg/day for 3 days, to be raised to 75 mg/day for week 2, to 150 mg/day for weeks 3–4, to 225 mg/day for weeks 5–6, to 300 mg/day for weeks 7–9, and to 375 mg/day for weeks 10–12.
Measures
At study intake, clinical research coordinators collected standard sociodemographic information and self-reported psychiatric history (including an assessment of suicidality) and completed the HAM-D and QIDS-C, as well as the Cumulative Illness Rating Scale (30 , 31) to measure medical comorbidity. The self-report Psychiatric Diagnostic Screening Questionnaire (32) was administered to assess for the presence of 11 concurrent psychiatric disorders (33) .
For the primary outcome measure, the HAM-D was administered in telephone interviews conducted by the research outcome assessors at entry and exit from each treatment level. Secondary outcomes measures obtained by the research outcome assessors included the 30-item Inventory of Depressive Symptomatology—Clinician Rating (34 – 36) , as well as the 5-item Income and Public Assistance Questionnaire to measure monthly income by source. Anxious depression was defined on the basis of pretreatment scores on the anxiety/somatization factor of the HAM-D (37) . Items from the Inventory of Depressive Symptomatology were used to establish the presence or absence of atypical features (38) and melancholic features (39) . Research outcome assessors blind to treatment assignments repeated the HAM-D, Inventory of Depressive Symptomatology, and Income and Public Assistance Questionnaire at the end of each treatment level.
A telephone-based interactive voice response system (40 , 41) was used to collect function and quality-of-life measures from participants within 72 hours of study entry and exit of each level, including the 16-item Quality of Life Enjoyment and Satisfaction Questionnaire (42) to assess quality of life, the 12-item Short Form Health Survey (43) to evaluate perceptions of mental and physical function, and the Work and Social Adjustment Scale (44) to measure occupational and interpersonal impairment. The interactive voice response system was also used to administer the self-report version of the QIDS (QIDS-SR) (22 – 24) for assessment of depression symptom severity at study entry, at week 6, and at exit from each level. Secondary symptom outcome measures included response and remission rates defined a priori by the QIDS-SR score. Remission was defined as a QIDS-SR score ≤5; response was defined as a reduction of ≥50% from baseline QIDS-SR score.
Statistical Analyses
Summary statistics are presented in the form of means and standard deviations for continuous variables and counts and percentages for discrete variables. Parametric and nonparametric analysis of variance methods and chi-square tests were used to compare baseline clinical and demographic features, treatment options, side effect measures, and serious adverse event rates across treatment group and for the entire sample.
All analyses were conducted using all patients in each randomization group (45) . Separate analyses were performed for the augmentation and switch strategies. The primary outcome measure was the intent-to-treat HAM-D remission rate at study exit. Participants for whom outcome HAM-D scores were missing were assumed not to have achieved remission (8) . Secondary outcome measures included response and remission rates at study exit according to the QIDS-SR. Adjustments for potential confounding effects were limited because of sample size and the inability of the models to converge. Exact logistic regression models were used to compare remission and response rates after adjusting for significant between-group differences (the effect of days to first postbaseline visit for the comparison of augmentation strategies and income in the comparison of switch strategies). To determine whether cognitive therapy had a differential effect by practice setting, exact logistic regression models were fit, including main effects for treatment and setting, as well as the two-way interaction. Because assessment with the QIDS-SR was more frequent across the treatment protocol, this measure was used to estimate the rapidity of response. Times to first remission (QIDS-SR score ≤5) and first response (≥50% reduction from baseline QIDS-SR score) were defined as the first observed point using clinic visit data. Survival hazard functions were estimated using the Kaplan-Meier method, and log-rank tests were used to compare the cumulative proportions of remission and response among the treatment groups.
All Level 2 comparisons in STAR*D were planned to have at least 80% power to detect between-group differences in remission rates of ≥15% (assuming approximately 200 patients per arm, use of two-tailed tests, and an alpha level of 0.05). Because the numbers of consenting participants in the cognitive therapy arms were substantially smaller than planned, the study had 80% power to detect only larger between-group differences, on the order of 22.5% for the augmentation arm and 29% for the switch arm.
Results
Augmentation With Cognitive Therapy or Medication
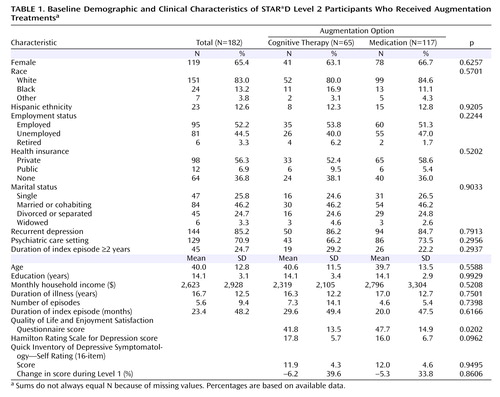
The baseline sociodemographic and clinical characteristics of participants assigned to augmentation treatments are summarized in Table 1 (a larger version of this table is available in a data supplement that accompanies the online version of this article). The mean Work and Social Adjustment Scale scores were significantly different between groups (cognitive therapy augmentation: 25.1 [SD=8.4]; medication augmentation: 21.3 [SD=9.0]; t=2.45, df=142, p=0.016), and the mean Quality of Life Enjoyment and Satisfaction Questionnaire scores were significantly different between these groups (cognitive therapy augmentation: 41.8 [SD=13.5]; medication augmentation: 47.7 [SD=14.9]; t=–2.35, df=142, p=0.020). The cognitive therapy augmentation group thus initially had greater functional impairment and a lower quality of life. No other significant differences between groups were observed in baseline characteristics.
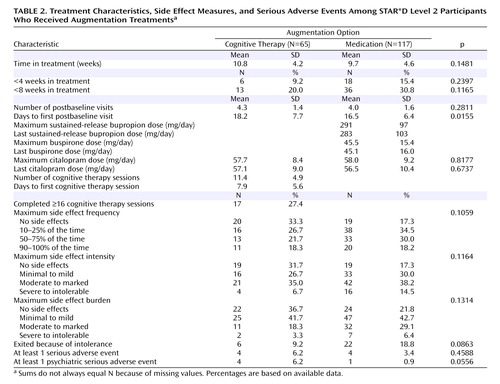
Patients in the cognitive therapy augmentation group attended an average of 11.4 sessions (SD=4.9), and 26% (17 of 65) of participants completed the full 16-session course of therapy. There were no significant differences between groups in mean number of weeks of Level 2 treatment or in the percentages of participants who discontinued treatment in less than 4 weeks or in less than 8 weeks. The only significant difference noted in Level 2 treatment characteristics was in mean days to first “on therapy” physician visit, which was slightly longer for the cognitive therapy augmentation group (18.2 days [SD=7.7] versus 16.5 days [SD=6.4]; χ 2 =5.86, df=1, p=0.016).
Augmentation with cognitive therapy and with medication were equally well tolerated. Four of the cognitive therapy augmentation patients experienced a psychiatric serious adverse event, as compared with only one of the medication augmentation patients (the difference was not statistically different). Data on Level 2 treatments, side effects, and serious adverse events for participants assigned to an augmentation treatment are listed in Table 2 .
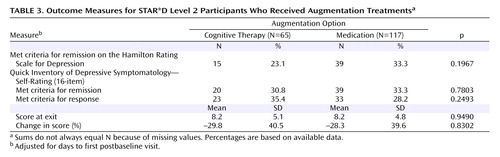
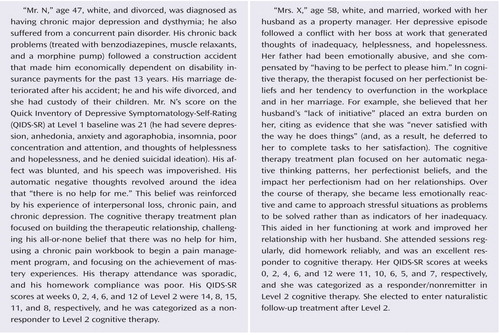
No significant differences were observed between groups in the percentages of participants who achieved remission according to HAM-D score ( Table 3 ), nor in the percentages of those who achieved remission or response as assessed by the QIDS-SR. The two groups had almost identical final (intent-to-treat) scores on the QIDS-SR. Patients assigned to medication augmentation tended to reach remission and response criteria faster than those in the cognitive therapy augmentation condition ( Figures 2 and 3 ), although only the difference in time to remission was statistically significant (p=0.022). Of those who achieved remission, the mean time to first remission was 55.3 days (SD=31.2) in the cognitive therapy group and 40.1 days (SD=25.8) in the medication group. There was no differential effect of cognitive therapy as a function of practice setting type (i.e., primary care versus psychiatric care settings).
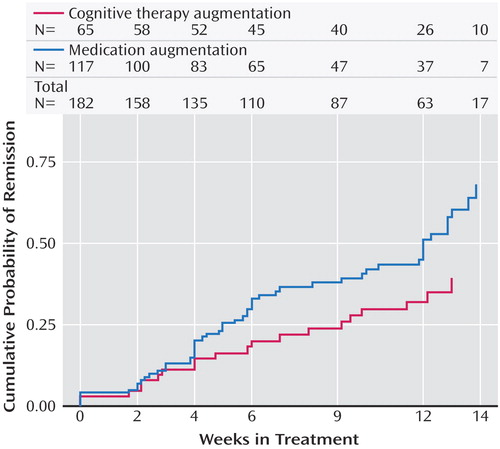
a Log-rank=5.2124, p=0.0224.
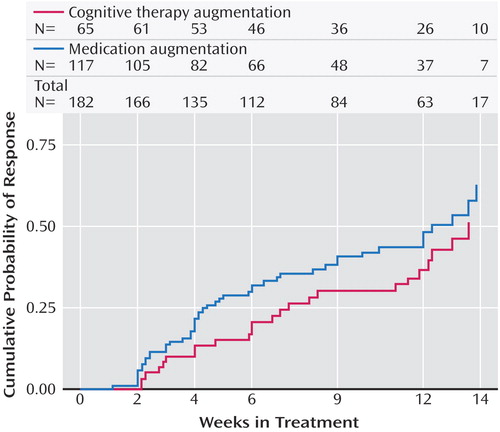
a Log-rank=1.8554, p=0.1732.
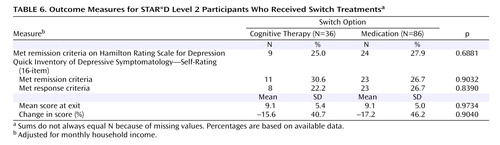
Cognitive Therapy Switch Versus Medication Switch
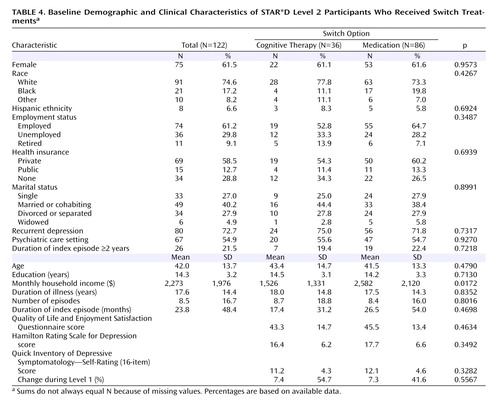
The sociodemographic and clinical characteristics of participants assigned to switch therapies are summarized in Table 4 (a larger version of this table is available in a data supplement that accompanies the online version of this article). A significant difference between groups was noted in monthly household income (cognitive therapy switch: $1,526 [SD=1,331]; medication switch: $2,582 [SD=2,120]; χ 2 =5.68, df=1, p=0.017). On measures of symptoms, illness features, and side effects, four significant differences were observed, including mean Level 2 baseline Work and Social Adjustment Scale score (cognitive therapy switch: 24.6 [SD=8.8]; medication switch: 20.9 [SD=7.7]; χ 2 =4.66, df=1, p=0.031) and maximum Level 1 side effect intensity (χ 2 =8.23, df=3, p=0.047). The group assigned to switch to cognitive therapy experienced somewhat fewer side effects during Level 1 citalopram therapy than those assigned to a medication switch, as would be expected if participants’ treatment strategy preferences were related to side effect burden.
We found no significant difference between groups in the mean number of weeks in Level 2 treatment, the percentage of participants who discontinued treatment in less than 4 weeks or in less than 8 weeks, or in mean days to first postrandomization visit.
As Table 5 shows, there were large differences between the switch treatment groups in measures of the frequency, intensity, and burden of medication side effects in Level 2. For example, 48% of the patients assigned to a second course of antidepressant therapy reported at least a moderate degree of side effect intensity, and 34% reported at least a moderate level of side effect burden, as compared with none of the patients in the cognitive therapy switch arm. Nevertheless, the between-group differences in exiting Level 2 treatment because of intolerance were not statistically significant. There were no psychiatric serious adverse events in either arm.
No significant difference was observed between groups in the percentage of patients who met HAM-D criteria for remission. Cognitive therapy switch and medication switch strategies resulted in similar degrees of change on the QIDS-SR and similar remission or response rates on this measure ( Table 6 ). Rapidity of therapeutic benefit, as measured by time to QIDS-SR response and remission, was essentially identical in these two switch strategies ( Figures 4 and 5 ). There was, again, no differential effect of cognitive therapy as a function of type of practice setting.
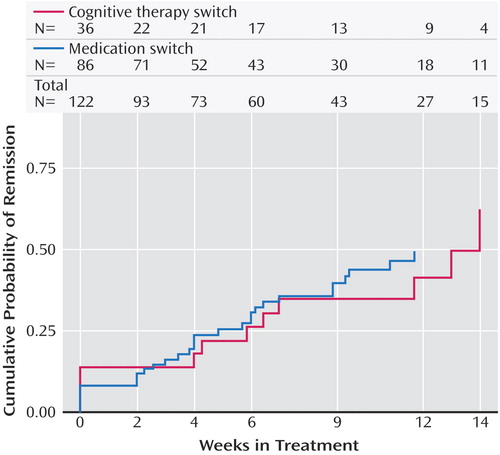
a Log-rank=0.0067, p=0.9350.
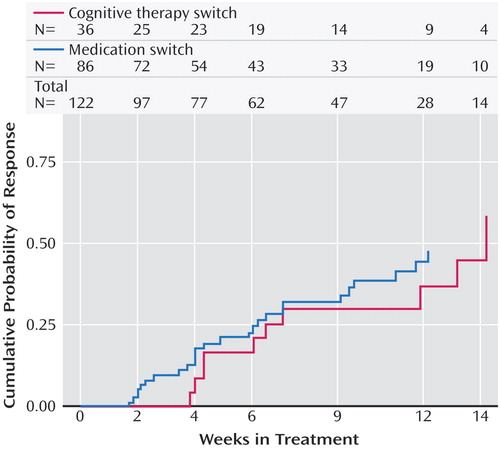
a Log-rank=0.1103, p=0.7398.
Discussion
Perhaps the most important finding of this study was that cognitive therapy, both alone and in combination with citalopram, was generally as effective as the various second-step pharmacologic strategies studied in STAR*D. Among participants who opted for an augmentation strategy, the addition of cognitive therapy ultimately resulted in about the same probability of remission and a similar degree of symptomatic improvement as adding sustained-release bupropion or buspirone. The benefit of cognitive therapy was slower to emerge, however, with a significant 20-day difference in median time to remission favoring pharmacologic augmentation. When speed of response is imperative, this 3-week advantage could be of considerable importance. An unanticipated finding was that pharmacologic augmentation was nearly as well tolerated as cognitive therapy augmentation. In fact, none of the between-group differences in side effect frequency, intensity, or burden were statistically significant.
Patients who switched treatments were likewise about as likely to benefit from cognitive therapy as those who were switched to sertraline, sustained-release bupropion, or extended-release venlafaxine. In contrast to the augmentation groups, the difference in speed of remission was not statistically significant. The major difference between switching to cognitive therapy and switching to another medication was that participants who received cognitive therapy alone were spared the side effect burden of a second course of pharmacotherapy. However, given that the percentage of patients who exited the study because of side effects did not differ between the cognitive therapy and medication switch arms, this advantage may be of limited clinical significance. As an aside, we thought it noteworthy that although the U.S. Food and Drug Administration warns of the emergence of suicidal ideation as a hazard following initiation of antidepressant medication, several cases of suicidal ideation occurred as serious adverse events following the initiation of cognitive therapy in our study.
The remission rates we report here for cognitive therapy (either switch or augmentation) are different from those reported previously by Rush et al. (46) because we used different STAR*D samples. For the cognitive therapy switch remission rates, Rush et al. reported on all participants who received a switch to cognitive therapy, whereas in this article we focused only on those who were both willing to be randomly assigned to cognitive therapy switch or medication switch and were randomly assigned to one of these treatments (see Figure 1 ; we excluded 24 participants who were willing only to receive cognitive therapy as a switch or augmentation and two who were willing to accept any treatment except medication switch). Likewise, for the cognitive therapy augmentation remission rates, Rush et al. report on all participants who received cognitive therapy augmentation, whereas we focused only on those who were both willing to be randomly assigned to cognitive therapy augmentation or medication augmentation and were randomly assigned to one of these treatments (see Figure 1 ; we excluded 20 participants who were willing only to receive cognitive therapy as a switch or augmentation).
The outcomes for participants treated with cognitive therapy in this study are generally comparable to those reported by Scott (13) and Schatzberg et al. (17) , although much less promising than those of Fava et al. (15) . The latter reported that 12 of 19 patients who had not benefited from antidepressant medication responded to a form of cognitive behavior therapy that emphasized life style management and engagement in healthy, adaptive activities. Although it is plausible that differences in the emphasis of therapy could explain the better outcomes, differences in design (Fava et al. conducted a nonrandomized, single-site case series with a single expert therapist) and patient illness characteristics (Fava et al. excluded patients with medical and psychiatric comorbidities) seem more likely to account for the differences.
The greatest shortcoming of this study is the lack of statistical power to detect moderately sized between-group differences. This low power was a result of lower-than-expected numbers of patients agreeing to randomization strata that included both cognitive therapy and pharmacotherapy. The STAR*D investigators had expected that more patients would be at equipoise on the acceptability of second-step treatments. In fact, one of the most surprising findings of STAR*D overall was that only 1.5% of patients were willing to accept all seven of the second-step options ( Figure 1 ). It was particularly surprising that only 26% of the patients were willing to accept assignment to cognitive therapy as either a switch or an augmentation strategy. These low numbers also limited the ability to control for imbalances in baseline characteristics.
The STAR*D investigators were experienced in designing studies of depression-focused psychotherapies, and the unexpectedly low acceptability of cognitive therapy was frankly at considerable variance with our earlier research experiences (see, for example, references 47–51). For example, even among more severely depressed inpatients, the Pittsburgh group (52) found that more than three-quarters of eligible patients accepted treatment with an intensive form of cognitive therapy alone instead of pharmacotherapy. Of particular relevance to the current study is the report of Schatzberg et al. (17) , in which chronically depressed patients who did not respond to 12 weeks of therapy with either a form of cognitive therapy or nefazodone were permitted to switch to the other treatment. In that study, 88% of participants who did not respond to nefazodone accepted the switch to psychotherapy, and 95% of those who did not respond to psychotherapy accepted the switch to nefazodone.
Psychosocial interventions likewise are not commonly viewed as “unacceptable” alternatives to pharmacotherapy outside of research studies. In fact, surveys of patients’ treatment preferences have consistently found that counseling and psychotherapy receive higher marks than pharmacotherapy (53 – 56) . Thus, it may be that some aspects of the design of STAR*D inadvertently biased patients against accepting cognitive therapy as compared with a second course of pharmacotherapy. For example, since the initial treatment in STAR*D was pharmacotherapy, patients who wanted to begin treatment with psychotherapy would very likely have opted not to enroll in the study. A second possible factor is the cost of study treatments. Whereas STAR*D provided the medications and most of the study-related sessions not covered by insurance, it was not possible for the study to reimburse participants for copayment charges for insurance-covered psychotherapy sessions. A third potential bias may have resulted from the need for patients to go to a different site to see a psychotherapist. If so, this is a real-world factor that may limit the utility of psychotherapy as a second-step option, given that referral to a provider at a different site is routine practice.
These were not the only factors that may have dampened patients’ enthusiasm for receiving psychotherapy, however, because cognitive therapy was significantly more acceptable to participants who opted for augmentation than it was to those who opted for a treatment switch. Perhaps the potential fear of breaking the treatment alliance with the study physician biased some patients against accepting a switch to cognitive therapy. Not only did participants in the augmentation groups get to continue citalopram, they also maintained an ongoing therapeutic relationship with their study physician. Finally, because patients who were already participating in psychotherapy could be enrolled in STAR*D, a small number of otherwise eligible participants who wished to continue their current therapy may have declined the option of cognitive therapy with a study therapist. Unfortunately, since we did not systematically record the number and nature of these extraprotocol courses of therapy, it is not possible to determine whether or not this was a common occurrence.
Another limitation of the study is that the fidelity of the therapy was not independently evaluated, and, because not all of the therapists were highly experienced with cognitive therapy, it is possible that some participants did not receive an optimal course of therapy. Both of these limitations reflect the STAR*D investigators’ decision to study the effectiveness of cognitive therapy under real-world conditions. That said, all study therapists were screened to ensure basic competence in cognitive therapy, and they received ongoing supervision—quality controls that probably surpass those generally found in clinical settings. Although it is not certain that expert therapists would have achieved better results with this difficult-to-treat patient population, there is evidence that therapist adherence is associated with better outcomes in cognitive therapy (57 , 58) . In two multicenter controlled studies (59 , 60) , site differences in cognitive therapy response suggest that therapists’ experience level may significantly affect outcomes, perhaps particularly for inpatients with more difficult-to-treat depression.
Our study examined only one form of psychotherapy. Other approaches, including interpersonal psychotherapy and the cognitive behavior analysis system of psychotherapy, may have yielded different results. Secondary analyses of the Treatment of Depression Collaborative Research Program suggest that interpersonal psychotherapy performed better than cognitive therapy among the subset of patients with more severe depressive symptoms (61 , 62) .
Finally, less than one-third of the patients remitted with any of the Level 2 treatments in STAR*D, which indicates that there is room for improvement in the treatment of depression. Future analyses will examine the impact of the STAR*D treatments on functioning and quality of life. Given that only about one-fourth of the patients treated with cognitive therapy completed the full 16-session protocol, it would be worthwhile to explore novel methods of facilitating mastery of therapy materials without increasing the number of therapy sessions. It would be useful in future research to determine whether concurrently starting psychotherapy and making changes in pharmacotherapy can result in higher remission rates. It would likewise be worthwhile in future research to study alternative methods of delivering therapy, such as greater use of telephone sessions and supplemental materials (e.g., self-help materials via print, Internet, video, or DVD modules), to determine whether the acceptability of psychotherapy can be improved.
1. Depression Guideline Panel: Depression in Primary Care, vol 2: Treatment of Major Depression. Clinical Practice Guideline No 5. AHCPR Publication No 93-0551. Rockville, Md, US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, 1993Google Scholar
2. Williams JW, Rost K, Dietrich AJ, Ciotti MC, Zyzanski SJ, Cornell J: Primary care physicians’ approach to depressive disorders: effects of physician specialty and practice. Arch Fam Med 1999; 8:58–67Google Scholar
3. Thase ME: Bipolar depression: issues in diagnosis and treatment. Harv Rev Psychiatry 2005; 13:257–271Google Scholar
4. Stimpson N, Agrawal N, Lewis G: Randomised controlled trials investigating pharmacological and psychological interventions for treatment-refractory depression: systematic review. Br J Psychiatry 2002; 181:284–294Google Scholar
5. Hollon SD, Jarrett RB, Nierenberg AA, Thase ME, Trivedi M, Rush AJ: Psychotherapy and medication in the treatment of adult and geriatric depression: which monotherapy or combined treatment? J Clin Psychiatry 2005; 66:455–468Google Scholar
6. Fava M, Rush AJ: Current status of augmentation and combination treatments for major depressive disorder: a literature review and a proposal for a novel approach to improve practice. Psychother Psychosom 2006; 75:139–153Google Scholar
7. Fava M, Rush AJ, Trivedi MH, Nierenberg AA, Thase ME, Sackeim HA, Quitkin FM, Wisniewski S, Lavori PW, Rosenbaum JF, Kupfer DJ: Background and rationale for the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study. Psychiatr Clin North Am 2003; 26:457–494Google Scholar
8. Rush AJ, Fava M, Wisniewski SR, Lavori PW, Trivedi MH, Sackeim HA, Thase ME, Nierenberg AA, Quitkin FM, Kashner TM, Kupfer DJ, Rosenbaum JF, Alpert J, Stewart JW, McGrath PJ, Biggs MM, Shores-Wilson K, Lebowitz BD, Ritz L, Niederehe G: Sequenced Treatment Alternatives to relieve Depression (STAR*D): rationale and design. Control Clin Trials 2004; 25:119–142Google Scholar
9. Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, Norquist G, Howland RH, Lebowitz B, McGrath PJ, Shores-Wilson K, Biggs MM, Balasubramani GK, Fava M, STAR*D Study Team: Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry 2006; 163:28–40Google Scholar
10. Rush AJ, Trivedi MH, Wisniewski SR, Stewart JW, Nierenberg AA, Thase ME, Ritz L, Biggs MM, Warden D, Luther JF, Shores-Wilson K, Niederehe G, Fava M: Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. N Engl J Med 2006; 354:1231–1242Google Scholar
11. Trivedi MH, Fava M, Wisniewski SR, Thase ME, Quitkin F, Warden D, Ritz L, Nierenberg AA, Lebowitz BD, Biggs MM, Luther JF, Shores-Wilson K, Rush AJ: Medication augmentation after the failure of SSRIs for depression. N Engl J Med 2006; 354:1243–1252Google Scholar
12. Friedman ES, Thase ME: Cognitive-behavioral therapy for depression and dysthymia, in Textbook of Mood Disorders. Edited by Stein DJ, Kupfer DJ, Schatzberg AF. Washington, DC, American Psychiatric Publishing, 2006, pp 353–371Google Scholar
13. Scott J: Chronic depression: can cognitive therapy succeed when other treatments fail? Behavioural Psychotherapy 1992; 20:25–36Google Scholar
14. Thase ME, Friedman ES, Howland RH: Management of treatment-resistant depression: psychotherapeutic perspectives. J Clin Psychiatry 2001; 62(suppl 18):18–24Google Scholar
15. Fava GA, Savron G, Grandi S, Rafanelli C: Cognitive-behavioral management of drug-resistant major depressive disorder. J Clin Psychiatry 1997; 58:278–282Google Scholar
16. McPherson S, Cairns P, Carlyle J, Shapiro DA, Richardson P, Taylor D: The effectiveness of psychological treatments for treatment-resistant depression: a systematic review. Acta Psychiatr Scand 2005; 111:331–340Google Scholar
17. Schatzberg AF, Rush AJ, Arnow BA, Banks PL, Blalock JA, Borian FE, Howland R, Klein DN, Kocsis JH, Kornstein SG, Manber R, Markowitz JC, Miller I, Ninan PT, Rothbaum BO, Thase ME, Trivedi MH, Keller MB: Chronic depression: medication (nefazodone) or psychotherapy (CBASP) is effective when the other is not. Arch Gen Psychiatry 2005; 62:513–520Google Scholar
18. Friedman EF, Thase ME, Biggs MM, Carmin C, Hollon SD, Kornblith SJ, Petersen T, Veenstra G, Wisniewski SR, Rush AJ: The implementation of cognitive therapy in STAR*D. Cognit Ther Res 2004; 28:819–833Google Scholar
19. American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
20. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Google Scholar
21. Hamilton M: Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 1967; 6:278–296Google Scholar
22. Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, Markowitz JC, Ninan PT, Kornstein S, Manber R, Thase ME, Kocsis JH, Keller MB: The 16-item Quick Inventory Of Depressive Symptomatology (QIDS), Clinician Rating (QIDS-C), and Self-Report (QIDS-SR): a psychometric evaluation inpatients with chronic major depression. Biol Psychiatry 2003; 54:573–583Google Scholar
23. Rush AJ, Bernstein IH, Trivedi MH, Carmody TJ, Wisniewski S, Mundt JC, Shores-Wilson K, Biggs MM, Woo A, Nierenberg AA, Fava M: An evaluation of the Quick Inventory of Depressive Symptomatology and the Hamilton Rating Scale for Depression: a Sequenced Treatment Alternatives to Relieve Depression trial report. Biol Psychiatry 2006; 59:493–501Google Scholar
24. Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, Crismon ML, Shores-Wilson K, Toprac MG, Dennehy EB, Witte B, Kashner TM: The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med 2004; 34:73–82Google Scholar
25. Wisniewski SR, Rush AJ, Balasubramani GK, Trivedi MH, Nierenberg AA: Self-rated global measure of the frequency, intensity, and burden of side effects. J Psychiatr Pract 2006; 12:71–79Google Scholar
26. Wisniewski SR, Eng H, Meloro L, Gatt R, Ritz L, Stegman D, Trivedi M, Biggs MM, Friedman E, Shores-Wilson K, Warden D, Bartolowits D, Martin JP, Rush AJ: Web-based communications and management of a multi-center clinical trial: the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) project. Clin Trials 2004; 1:387–398Google Scholar
27. Lavori PW, Rush AJ, Wisniewski SR, Alpert J, Fava M, Kupfer DJ, Nierenberg A, Quitkin FM, Sackeim HA, Thase ME, Trivedi M: Strengthening clinical effectiveness trials: equipoise-stratified randomization. Biol Psychiatry 2001; 50:792–801Google Scholar
28. Shaw BF: Specification of the training and evaluation of cognitive therapists for outcome studies, in Psychotherapy Research: Where We Are and Where We Should Go. Edited by Williams JBW, Spitzer RL. New York, Guilford, 1984, pp 173–189Google Scholar
29. Jarrett RB, Kraft D, Doyle J, Foster BM, Eaves GG, Silver PC: Preventing recurrent depression using cognitive therapy with and without a continuation phase: a randomized clinical trial. Arch Gen Psychiatry 2001; 58:381–388Google Scholar
30. Linn BS, Linn MW, Gurel L: Cumulative Illness Rating Scale. J Am Geriatr Soc 1968; 16:622–626Google Scholar
31. Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, Mulsant B, Reynolds CFI: Rating chronic medical illness burden in geropsychiatric practice and research: application of the cumulative illness rating scale. Psychiatry Res 1992; 41:237–248Google Scholar
32. Zimmerman M, Mattia JI: The reliability and validity of a screening questionnaire for 13 DSM-IV axis I disorders (the Psychiatric Diagnostic Screening Questionnaire) in psychiatric outpatients. J Clin Psychiatry 1999; 60:677–683Google Scholar
33. Rush AJ, Zimmerman M, Wisniewski SR, Fava M, Hollon SD, Warden D, Biggs MM, Shores-Wilson K, Shelton RC, Luther JF, Thomas B, Trivedi MH: Comorbid psychiatric disorders in depressed outpatients: demographic and clinical features. J Affect Disord 2005; 87:43–55Google Scholar
34. Rush AJ, Giles DE, Schlesser MA, Fulton CL, Weissenburger JE, Burns CT: The Inventory for Depressive Symptomatology (IDS): preliminary findings. Psychiatry Res 1986; 18:65–87Google Scholar
35. Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH: The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychol Med 1996; 26:477–486Google Scholar
36. Rush AJ, Carmody TJ, Reimitz PE: The Inventory of Depressive Symptomatology (IDS): Clinician (IDS-C) and Self-Report (IDS-SR) ratings of depressive symptoms. Int J Methods Psychiatr Res 2000; 9:45–59Google Scholar
37. Fava M, Alpert JE, Carmin CN, Wisniewski SR, Trivedi MH, Biggs MM, Shores-Wilson K, Morgan D, Schwartz T, Balasubramani GK, Rush AJ: Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D. Psychol Med 2004; 34:1299–1308Google Scholar
38. Novick JS, Stewart JW, Wisniewski SR, Cook IA, Manev R, Nierenberg AA, Rosenbaum JF, Shores-Wilson K, Balasubramani GK, Biggs MM, Zisook S, Rush AJ: Clinical and demographic features of atypical depression in outpatients with major depressive disorder: preliminary findings from STAR*D. J Clin Psychiatry 2005; 66:1002–1011Google Scholar
39. Khan AY, Carrithers J, Preskorn SH, Lear R, Wisniewski SR, Rush AJ, Stegman D, Kelley C, Kreiner K, Nierenberg AA, Fava M: Clinical and demographic factors associated with DSM-IV melancholic depression. Ann Clin Psychiatry 2006; 18:91–98Google Scholar
40. Mundt JC: Interactive voice response systems in clinical research and treatment. Psychiatr Serv 1997; 48:611–612Google Scholar
41. Kobak KA, Greist JH, Jefferson JW, Mundt JC, Katzelnick DJ: Computerized assessment of depression and anxiety over the telephone using interactive voice response. MD Comput 1999; 16:64–68Google Scholar
42. Endicott J, Nee J, Harrison W, Blumenthal R: Quality-of-Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacol Bull 1993; 29:321–326Google Scholar
43. Ware J Jr, Kosinski M, Keller SD: A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34:220–233Google Scholar
44. Mundt JC, Marks IM, Shear MK, Greist JH: The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry 2002; 180:461–464Google Scholar
45. Fisher L, Dixon D, Herson J, Frankowski R, Hearron M, Peace K: Intention-to-treat in clinical trials, in Statistical Issues in Drug Research and Development. Edited by Ke P. New York, Marcel Dekker, 1990Google Scholar
46. Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, McGrath PJ, Rosenbaum JF, Sackeim HA, Kupfer DJ, Luther J, Fava M: Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry 2006; 163:1905–1917Google Scholar
47. Rush AJ, Beck AT, Kovacs M, Hollon SD: Comparative efficacy of cognitive therapy and pharmacotherapy in the treatment of depressed outpatients. Cognit Ther Res 1977; 1:17–37Google Scholar
48. Thase ME, Simons AD, Cahalane J, McGeary J, Harden T: Severity of depression and response to cognitive behavior therapy. Am J Psychiatry 1991; 148:784–789Google Scholar
49. Thase ME, Friedman ES, Berman SR, Fasiczka AL, Lis JA, Howland RH, Simons AD: Is cognitive behavior therapy just a “nonspecific” intervention for depression? a retrospective comparison of consecutive cohorts treated with cognitive behavior therapy or supportive counseling and pill placebo. J Affect Disord 2000; 57:63–71Google Scholar
50. Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, Markowitz JC, Nemeroff CB, Russell JM, Thase ME, Trivedi MH, Zajecka J: A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med 2000; 342:1462–1470Google Scholar
51. Hollon SD, DeRubeis RJ, Shelton RC, Amsterdam JD, Salomon RM, O’Reardon JP, Lovett ML, Young PR, Haman KL, Freeman BB, Gallop R: Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Arch Gen Psychiatry 2005; 62:417–422Google Scholar
52. Thase ME, Dubé S, Bowler K, Howland RH, Myers JE, Friedman E, Jarrett DB: Hypothalamic-pituitary-adrenocortical activity and response to cognitive behavior therapy in unmedicated, hospitalized depressed patients. Am J Psychiatry 1996; 153:886–891Google Scholar
53. Drugs vs talk therapy: 3,079 readers rate their care for depression and anxiety. Consum Rep 2004; 69(10):22–29Google Scholar
54. Gum AM, Arean PA, Hunkeler E, Tang LQ, Katon W, Hitchcock P, Steffens DC, Dickens J, Unutzer J: Depression treatment preferences in older primary care patients. Gerontologist 2006; 46:14–22Google Scholar
55. Jaycox LH, Asarnow JR, Sherbourne CD, Rea MM, LaBorde AP, Wells KB: Adolescent primary care patients’ preferences for depression treatment. Adm Policy Ment Health 2006; 33:198–207Google Scholar
56. Lowe B, Schulz U, Grafe K, Wilke S: Medical patients’ attitudes toward emotional problems and their treatment: what do they really want? J Gen Intern Med 2006; 21:39–45Google Scholar
57. Bryant MJ, Simons AD, Thase ME: Therapist skill and patient variables in homework compliance: controlling an uncontrolled variable in cognitive therapy outcome research. Cognit Ther Res 1999; 23:381–399Google Scholar
58. Shaw BF, Elkin I, Yamaguchi J, Olmsted M, Vallis TM, Dobson KS, Lowery A, Sotsky SM, Watkins JT, Imber SD: Therapist competence ratings in relation to clinical outcome in cognitive therapy of depression. J Consult Clin Psychol 1999; 67:837–846Google Scholar
59. DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, O’Reardon JP, Lovett ML, Gladis MM, Brown LL, Gallop R: Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch Gen Psychiatry 2005; 62:409–416Google Scholar
60. Jacobson NS, Hollon SD: Cognitive-behavior therapy versus pharmacotherapy: now that the jury’s returned its verdict, it’s time to present the rest of the evidence. J Consult Clin Psychol 1996; 64:74–80Google Scholar
61. Elkin I, Gibbons RD, Shea MT, Sotsky SM, Watkins JT, Pilkonis PA, Hedeker D: Initial severity and differential treatment outcome in the National Institute of Mental Health Treatment of depression Collaborative Research Program. J Consult Clin Psychol 1995; 63:841–847Google Scholar
62. Klein DF, Ross DC: Reanalysis of the National Institute of Mental Health Treatment of Depression Collaborative Research Program General Effectiveness Report. Neuropsychopharmacology 1993; 8:241–251Google Scholar