Treatments for Later-Life Depressive Conditions: A Meta-Analytic Comparison of Pharmacotherapy and Psychotherapy
Abstract
Objective: To improve interventions for depressed older adults, data are needed on the comparative effects of pharmacotherapy versus psychotherapy. Given that most older adults with clinically significant depressive symptoms do not have major depression, data on treatments for minor depression and dysthymia are especially needed. Method: Meta-analysis was used to integrate the results of 89 controlled studies of treatments focused on acute major depression (37 studies) and other depressive disorders (52 studies conducted with mixed diagnostic groups, including patients with major depression, minor depression, and dysthymia). A total of 5,328 older adults received pharmacotherapy or psychotherapy in these studies. Results: Clinician-rated depression scores improved, on average, by 0.80 standard deviation (SD) units; self-rated depression scores improved by 0.76 SD units. Clinician-rated depression improved by 0.69 SD units in pharmacotherapeutic studies and by 1.09 SD units in psychotherapeutic studies. Self-rated depression improved by 0.62 SD units and 0.83 SD units, respectively. An interesting finding was the stronger improvements in clinician-rated depression among control subjects participating in medication studies, compared to those in psychotherapeutic studies. Conclusions: Available treatments for depression work, with effect sizes that are moderate to large. Comparisons of psychotherapy and pharmacotherapy must be interpreted with caution, in part because medication studies are more likely to use a credible active placebo, which may lead to smaller adjusted effect sizes in medication studies. Given that psychotherapy and pharmacotherapy did not show strong differences in effect sizes, treatment choice should be based on other criteria, such as contraindications, treatment access, or patient preferences.
In the United States and other Western countries, older adults are the fastest-growing segment of the population. Depression is one of the most common mental disorders in advanced age. Estimates of the point prevalence of major depression in community-dwelling older adults range from 1.5 to 5.0% (1) . Minor depression and dysthymia are present in another 10% (1 – 3) . All depressive conditions contribute to medical illness and disability in late life (4) , increase the risk of institutionalization (5) , and amplify the risk for all-cause mortality (6) and suicide (7 , 8) . Minor depression and dysthymia account for comparable levels of disability and distress (9 , 10) .
In order to improve interventions with depressed older adults, more knowledge of the comparative effects of different forms of therapy is needed. The present meta-analysis focuses on the effects of pharmacotherapy versus psychotherapy. Although three consensus statements recommending treatments for late-life depression have been issued, none was informed by a comprehensive meta-analysis (11 – 13) . Previous meta-analyses (14 , 15) were inconclusive, as they were based on a small number of studies that focused exclusively on major depression. Yet only a minority of significantly depressed older adults suffer from that disorder. Therefore, our meta-analysis also examined the effects of treatments for minor depression and dysthymia. Given that rigorous placebo-controlled studies reveal nonspecific effects (16) , we excluded uncontrolled studies.
Advantages and Disadvantages of Commonly Used Pharmacotherapies and Psychotherapies for Depressed Older Adults
The antidepressant drugs used in unipolar later-life depression include selective serotonin reuptake inhibitors (SSRIs), other agents with varied mechanisms of action (e.g., venlafaxine, mirtazapine), and older classes such as tricyclic antidepressants and monoamine oxidase inhibitors (MAOIs) (1) . SSRIs and other newer agents have become first-line treatments for most primary care physicians, psychiatrists, and other medical specialists because of their relative tolerability and ease of use in terms of dosing schedules. Nonetheless, many older adults are reluctant to accept pharmacotherapy (17) and may be prone to drug side effects (including organ-specific side effects) and drug-drug interactions.
The most commonly studied psychotherapeutic treatment of depression is cognitive behavior therapy, which is focused on changing maladaptive patterns of thinking, feeling, and behaving (18) . Other forms of psychotherapy for which there is empirical support are interpersonal psychotherapy (19) , psychodynamic therapy (20) , and eclectic therapy (21) .
The advantages of psychotherapy include the lack of drug side effects and drug-drug interactions. Given that psychosocial stressors may engender or exacerbate depressive episodes (22) , the focus in psychotherapy of enhancing social supports, resolving interpersonal stressors, or increasing coping abilities may be useful and desirable (23) . Moreover, many older adults are more likely to accept psychotherapy than pharmacotherapy (17) . An often-mentioned disadvantage of psychotherapy relative to medication is the slower response (24) , but there are structural disadvantages too, including language, financial, and transportation barriers and the lack of psychotherapists who are trained to work with older adults (23) .
Prior Comparative Meta-Analyses
The first meta-analysis that tried to compare pharmacotherapy and psychotherapy for depressed older adults ultimately excluded psychotherapeutic studies from the analysis because the authors could identify only two reports (15) . Gerson et al. (14) compared 41 medication studies with four psychotherapy studies conducted with patients 55 years of age and older who had been diagnosed with major depression. The outcome variable was change in clinician-rated depression as measured with the Hamilton Rating Scale for Depression (25) . Uncontrolled studies were included. Psychotherapy showed significantly smaller improvements than antidepressants, but this difference disappeared after the authors statistically controlled for baseline depression. The exclusive focus on major depression precluded the authors from drawing conclusions about treatments for other forms of depression. By including uncontrolled studies, the authors were unable to calculate effect size measures that controlled for change due to nonspecific factors, such as placebo effects and spontaneous remission.
Goals of the Present Meta-Analysis
We compared the effects of pharmacotherapy and psychotherapy in clinically depressed older adults, including the effects of different forms of treatment (e.g., tricyclic antidepressant versus SSRI). We analyzed whether effect sizes vary as a function of clinical variables, treatment setting, and demographic variables.
One potentially important clinical variable is depression severity. A meta-analysis of psychotherapeutic interventions (26) found lower levels of improvement in older adults with major depression than in those with other forms of depression, but this was not replicated in a subsequent meta-analysis (27) . In a meta-analysis of mixed-age groups, the effects of pharmacotherapy were greater in patients who were more depressed before treatment (28) . In the present study, we computed separate effect sizes for studies conducted exclusively on groups of patients with major depression and those conducted on groups that also included patients with minor depression and dysthymia.
A second potentially important clinical variable is medical comorbidity, including the presence of neurodegenerative disorders. Although several studies showed no differences in treatment effects as a function of medical burden (29 , 30) , others showed less improvement (31) or more improvement (32) in patients with greater medical burden. In this meta-analysis, we compared effect sizes for studies conducted on groups defined by the presence of medical comorbidity (e.g., major depression in people with heart disease) and groups defined solely by the presence of a depressive disorder.
With respect to the effects of treatment setting, interventions with inpatients and outpatients may vary in quality, intensity, and length. These differences could have implications for treatment effectiveness (33) . In the present meta-analysis, we compared effect sizes of treatments conducted on groups composed entirely of inpatients versus those that included a mix of inpatients and outpatients.
Finally, treatment effects may also vary by demographic characteristics, particularly age and gender. For example, a meta-analysis of psychotherapy with older adults (34) and another conducted on patients across the adult age range (35) both demonstrated lower levels of improvement in older patients. Given that women are more likely to become depressed than men (36) , there may also be gender differences in the effects of interventions. A meta-analysis of eight studies did not show gender differences in treatment effects (37) , perhaps because of inadequate power.
Method
Data Set
A comprehensive data set of studies that investigated the effects of pharmacological and psychotherapeutic interventions with depressed older adults was identified by searching electronic data bases (MEDLINE, Cochrane Data Base, PsycINFO, PSYNDEX) with the following search terms: [depression or depressed] and [intervention or clinical trial or therapy] and [elderly or old age]); the entries were cross-referenced. The criteria for inclusion in the meta-analysis were as follows:
1. The participants had a mean or median age of 60 years or greater.
2. The study participants met the criteria for major depressive disorder, minor depressive disorder, or dysthymic disorder according to ICD-10, DSM-III, DSM-III-R, or DSM-IV, including the criteria for minor depression in the appendix to DSM-IV. (The language used to describe mood disorders other than major depression and dysthymic disorder is variable, including terms such as clinical depression, minor depression, “subsyndromal” or “subthreshold” depression, or depression of mild and moderate intensity [13] . Many intervention studies defined the level of depression by using cutoffs from the Hamilton Depression Rating Scale [25] or other depression scale. If the cutoff for major depression was not met for all patients—usually it was for most patients—but all patients had depression scores above the normal level, this study was categorized as including depressive disorders other than major depression.)
3. An intervention subgroup was compared to a control subgroup, e.g., patients assigned to placebo or a waiting list. (All pharmacological and four psychotherapeutic studies used a drug placebo. In addition, six psychotherapeutic studies used an irrelevant activity as an attention-placebo condition, two psychotherapeutic studies used usual care, and the remaining 22 studies used a waiting list control group.)
4. Statistics could be computed or estimated for change in self-rated and/or clinician-rated depression (e.g., means and standard deviations, d values) and/or rate of response or remission.
The use of random assignment was a criterion for the evaluation of study quality. We did not limit our search to randomized studies because random assignment is often difficult to implement, particularly in group treatment contexts. For example, in studies of group psychotherapy a minimum number of participants must be recruited in a brief interval to start the group, so patients are often consecutively (nonrandomly) assigned.
A list of the 89 eligible studies is available online at http://www2.uni-jena.de/svw/devpsy/staff/download/appendixmp.pdf. Thirty-one studies were excluded because they included nondepressed people (15 studies), duplicated data sets that were already included in the meta-analysis (six studies), did not meet our age cutoff (three studies), were limited to maintenance therapy (three studies), had an inadequate control group (one study), reported only the results of responders (one study), or did not report separate results for patients receiving psychotherapy and pharmacotherapy (two studies). Studies of maintenance therapy, combination treatments (medication and psychotherapy), and collaborative treatments were excluded because of an insufficient number of available studies. For example, none of the studies included in a recent meta-analysis of the effects of combination treatments was conducted with older adults (38) .
Most articles were in English (81 studies), four were in German, one was in Italian, one was in Chinese, and two were in French. The majority of articles were from The Journal of Clinical Psychiatry (10 studies), The American Journal of Psychiatry (eight studies), the Journal of Consulting and Clinical Psychology (four studies), Clinical Gerontologist (four studies), and other journals and books (60 studies). An additional three studies were reported in presentations at conventions and were published as abstracts. A native speaker translated the Chinese paper, and one of us (M.P.) read the other foreign-language papers. On the basis of 20% of the studies, two coders of the study characteristics achieved an average interrater agreement (Cohen’s kappa) of 0.87. Disagreements were resolved by consensus.
Measures
Clinical characteristics
Clinician-rated depressive symptom severity was measured with the Hamilton depression scale (61 studies), the Montgomery-Åsberg Depression Scale (39) (four studies), and other scales (10 studies). Self-rated severity of depressive symptoms was assessed with the Beck Depression Inventory (40) (21 studies), the Geriatric Depression Scale (41) (20 studies), and other scales (19 studies). Twenty-nine studies did not assess self-rated depression, and 14 did not measure clinician-rated depression.
Thirty-seven studies were exclusively focused on treatments of major depression, six studies included minor depression and dysthymia, and 46 studies included patients with major depression, minor depression, or dysthymia. In statistical analysis, this variable was dichotomous and was rated as 1 (major depression; 37 studies) or 0 (major depression plus other diagnoses; 52 studies). We also coded whether all participants were diagnosed as having physical illness or cognitive impairment; this variable was rated as 1 (comorbidity present; 17 studies) or 0 (no comorbidity; 72 studies). Few studies provided sufficient information to enable us to compute a more differentiated measure of comorbidity and examine its effects on treatment outcome. Similarly, the data were insufficient to allow us to examine the effects of psychiatric comorbidity.
Remission and response
Remission was measured as the percentage of patients who were no longer clinically depressed (according to a structured clinical interview or the cutoff on a depression scale) or who no longer met diagnostic criteria for major depression (24 studies). Treatment response was measured as the percentage of patients who showed remission (24 studies), who had a score of 1 or 2 on the Clinical Global Impression severity and improvement scales (42) (nine studies), who showed a reduction in Hamilton score of 50% or more (five studies), or who met another criterion (three studies). Forty-eight studies did not provide sufficient information for us to examine response.
Quality of report
The criteria for report quality were mainly based on the recommendations of Jüni et al. (43) . The three individual criteria were use of random assignment (1=yes, 0=no), use of raters masked or blinded to assignment (1=yes, 0=no/not reported), and use of intention-to-treat analysis (1=yes, 0=no).
Statistical Integration of Research Findings
We entered the year of publication, the numbers of patients in the intervention and control groups, mean age, gender distribution, clinical characteristics (two dichotomous variables: major depression only, presence of medical comorbidity), treatment setting and duration, clinician-rated and self-rated depression scores and their respective change scores, rates of treatment response and remission, and the three study quality indicators.
Calculations for the meta-analysis of change in clinician- and self-rated depression were performed in six steps, by using random-effects models (44) , which are recommended when there is variability in effect sizes among studies beyond subject-level sampling error and when all sources of heterogeneity cannot be identified. As a large number of individual drugs and individual psychotherapeutic procedures have been used to treat depression, heterogeneity of treatment effects is probable. The steps in our calculations were as follows.
1. We computed the effect size (d) for each study as the difference in the posttreatment measure between the treatment and control conditions divided by the pooled SD (45) . Effect sizes were also derived from F values, exact p values, and alpha levels. The effect size estimates were adjusted for bias due to differences in baseline values between the therapy and control condition (46) and due to overestimation of the population effect size (common for small groups) (47) . When effects of more than one treatment were evaluated, we computed a separate effect size for each treatment group. When two outcome measures were used (e.g., two self-rating scales), the mean effect size was computed across the measures. Outliers that were more than two SDs from the mean of the effect sizes were recoded to the value of two SDs (45 , 46 , 48) .
2. Weighted mean effect sizes were computed (44) .
3. The homogeneity of effect sizes was computed by using the homogeneity statistic Q, which is distributed approximately as χ 2 with k – df, where k is the number of effect sizes (treated subgroups).
4. The significance of the mean was tested by dividing the weighted mean effect size by the estimated SD; confidence intervals (CIs) that included 95% of the effects were subsequently computed for each effect size. Differences between two conditions were interpreted as significant when the 95% intervals did not overlap.
5. Weighted ordinary least squares regression analyses (44) were conducted to identify predictors of outcome.
6. As a tool for interpreting the practical significance of the results, we used the binomial effect size display (48) . If the treatment and control groups are of equal size and patients with above-average and below-average improvements are split at the median, then the percentage of patients with above-average improvements in the treatment condition is computed as 0.5 + r/2 and the percentage of above-average improvement in the control group is 0.5 – r/2; r is computed by transforming the mean effect size d.
For comparing the proportions of responders in the treatment and control groups, we computed Mantel-Haenszel statistics of the odds ratio (49) . This effect size statistic compares two groups in terms of the relative odds of a status or event, such as being a responder, and is the quotient of the probability of responding (p) and nonresponding (1 – p). The odds ratio for responding in the treatment and control groups is computed by dividing the odds of responding in the treatment condition by the odds of responding in the control group.
First, odds ratios were computed for each study. Then a weighted Mantel-Haenszel summary estimate was computed (49) ; confidence intervals that included 95% of the effects were subsequently computed for each odds ratio. Finally, the significance and homogeneity of the odds ratio were tested by chi-square statistics (49) .
Results
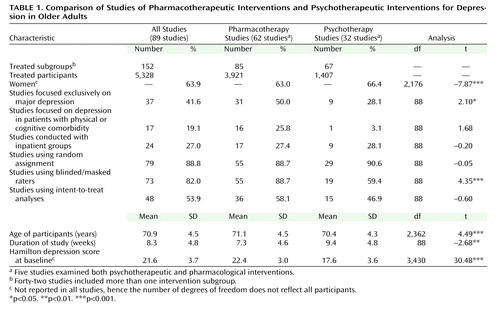
As shown in Table 1 , 62 studies investigated the effect of pharmacotherapy and 32 examined the effect of psychotherapy; five studies examined both kinds of intervention. No significant differences between pharmacotherapy and psychotherapy appeared in the percentages of studies focused exclusively on patients with comorbidity, studies conducted with inpatients, and studies using random assignment. Medication studies were about 2 weeks shorter, more likely to be conducted on groups with major depression exclusively, and more likely to use masked ratings. Patients in medication studies were about a year older, slightly less likely to be women, and slightly more depressed at baseline.
Treatment Responses
First, we computed the effects of pharmacotherapeutic and psychotherapeutic interventions. Separate analyses were computed for clinician-rated depression and self-rated depression ( Table 2 ). Negative d values indicate a stronger decline of depression in the intervention group than in the control group. For example, d=–1.00 would indicate a stronger improvement with treatment of 1.00 SD.
As shown in Table 2 , interventions produced an average improvement in clinician-rated depression of 0.80 SD units. For self-rated depression, the improvement was 0.76 SD units. When we apply Cohen’s guidelines (50) , the effect on clinician-rated depression may be described as large, whereas the effect on self-rated depression may be considered moderate. Rosenthal (48) suggested the binomial effect size display as a tool for interpreting the practical importance of meta-analytic results. For clinician-rated depression, 68.6% of the members of the treatment groups and 31.4% of the control group members showed above-average improvement. The corresponding figures for self-rated depression are 67.8% (treatment) and 32.2% (control condition).
For clinician-rated depression, psychotherapeutic interventions showed larger effect sizes than pharmacotherapeutic interventions. This is shown by the absence of overlap of the confidence intervals and also by the binomial effect size display; 66.3% of the patients receiving pharmacotherapy and 72.4% of those receiving psychotherapy showed above-average improvement in clinician-rated depression. For self-rated depression, the two interventions yielded comparable effect sizes; 64.8% of the patients receiving pharmacotherapy and 69.2% of those in psychotherapy showed above-average improvements.
As pharmacological studies differ from psychotherapeutic studies in the use of an active placebo (16) , we further analyzed whether changes in the control group members differed between these treatment types. As indicated by the absence of overlap of the confidence intervals, we found stronger improvements in clinician-rated depression in the control groups in the medication trials (psychotherapy: k=23, d=–0.33, 95% CI=–0.53 to –0.13; medication: k=59, d=–0.91, CI=–1.23 to –0.60). When we used a different statistical method that did not control for nonspecific changes in control group members (14) , pharmacotherapy and psychotherapy showed similar effect sizes for clinician-rated depression (k=32, d=–1.75, CI=–1.96 to –1.53 versus k=69, d=–1.61, CI=–1.88 to –1.34) and self-rated depression (k=22, d=–0.80, CI=–1.09 to –0.52 versus k=48, d=–1.17, CI=–1.35 to –0.99). Thus, when we controlled for nonspecific changes in the control groups, we uncovered a slight advantage for psychotherapy on clinician-rated depression; failing to control for nonspecific changes obscured the difference between psychotherapy and medication.
Separate analyses of the five studies that included pharmacotherapeutic, psychotherapeutic, and control conditions showed no differences in effects for clinician-rated depression (pharmacotherapy: k=4, d=–0.54, CI=–1.00 to –0.09; psychotherapy: k=4, d=–0.41, CI=–0.82 to –0.00) and self-rated depression (k=3, d=–0.27, CI=–0.50 to –0.03 versus k=3, d=–0.19, CI=–0.41 to 0.04).
Next, we compared the effects of different medication classes and different psychotherapies. With respect to the pharmacotherapies, we were able to compare SSRIs with tricyclic antidepressants, MAOIs, and other drugs. The other drugs were acetyl- l -carnitine, an ACTH (4-9) analogue (Org 2766), alprazolam, bupropion, medifoxamine, fluvoxamine, iproniazid, l -sulpiride, methylphenidate, mianserin, minaprine, mirtazapine, nomifensine, trazodone, tryptophan, venlafaxine, viloxazine, and a combination of dihydroergocristine and l -5-hydroxytryptophan.
With regard to psychotherapy, we were able to compare cognitive behavior therapy against other psychotherapies. The other psychotherapies included eclectic psychotherapies, focused visual imagery group therapy (focusing the imagination on personal strengths and positive aspects of losses), interpersonal psychotherapy, psychodynamic therapy, and reminiscence. We also compared group therapy and individual psychotherapy. There were no significant differences in improvement of clinician-rated depression between the drug groups ( Table 2 ). However, the effect of cognitive behavior therapy on clinician-rated depression was greater than the effects of other forms of psychotherapy, SSRIs, other drugs, and all medications combined. With regard to change in self-rated depression, SSRIs were less effective than tricyclic antidepressants, MAOIs, other drugs, and both groups of psychotherapy. Given that only four studies of SSRIs were available, this result should be interpreted with caution.
Next, we investigated the effects of the clinical characteristics of the study groups. Analyses suggested that pharmacotherapy (k=39, d=–0.79, CI=–0.95 to –0.64, z=–10.01, p<0.001) and psychotherapy (k=16, d=–0.96, CI=–1.23 to –0.69, z=–6.87, p<0.001) were similarly effective in decreasing observer-rated depression in studies focused exclusively on major depression. However, in studies that also included patients with minor depression and/or dysthymia, the effect of psychotherapy was larger (k=19, d= –1.21, CI=–1.42 to –1.00, z=–11.48, p<0.001) than the effect of pharmacotherapy (k=38, d=–0.59, CI=–0.76 to –0.41, z= –6.40, p<0.001). The pattern of findings remained unchanged when we reran these analyses without the six studies focused on minor depression or dysthymia. The significant differences were confined to analyses of changes in clinician-rated depression; no differences were found for self-rated depression.
The reports on 41 studies (with 59 subgroups) included the proportion of responders. About 47% of patients in the treatment groups and about 27% of the control group members were responders. As shown in Table 3 , the relative odds of responding to the treatment condition (the quotient of the odds of responding divided by the odds of nonresponding) was 0.88, as compared to 0.37 in the control condition. Pharmacotherapy and psychotherapy yielded comparable odds, with overlapping 95% confidence intervals of the odds ratios.
Similar findings were observed when we analyzed the percentage of patients in remission. Again, the overlapping 95% confidence intervals indicate that there were no significant differences ( Table 3 ).
Multivariate Regression Analyses
The analyses reported thus far did not adjust for covariates. Next, we computed two weighted multiple linear regressions. As shown in Table 4 , statistical control for group characteristics suggests that psychotherapy yields a higher effect size than medication for clinician-rated depression.
Discussion
In the early 1990s, a common belief was that psychotherapeutic interventions would be of less use than pharmacotherapy for depressed older adults. This idea, given credibility in a consensus statement (11) , was supported by a previous meta-analysis (14) . Unlike the previous meta-analysis, our search was not confined to studies of major depression; it included studies that examined treatments for other forms of clinical depression. The present meta-analysis shows that psychotherapy and pharmacotherapy yield comparable effect sizes overall, but the findings are even more interesting upon closer inspection. Although there are inherent methodological differences between medication and psychotherapy studies, this meta-analysis has generated an important, testable hypothesis: older adults with minor depression or dysthymia may be more likely to benefit from psychotherapeutic interventions than from antidepressants. Rigorous studies are needed to test this hypothesis before psychotherapy can legitimately be offered as a first-line treatment for these common conditions.
The better effect of psychotherapy observed in the present meta-analysis is attributable largely to our expanded inclusion criterion, as we found no advantage of psychotherapy in studies on major depression. Although the difference between the previous meta-analysis (14) and this one might be ascribed to the inclusion of recently published studies, there was no association between treatment effect size and year of publication for psychotherapy studies (self-rated depression: r=0.13, df=51; clinician-rated depression: r=–0.07, df=34). However, more recent medication studies showed higher effect sizes (self-rated depression: r=0.44, df=27; clinician-rated depression: r=0.25, df=76; p<0.05 in both cases), indicating progress in the development of drugs with potent effects. Nonetheless, the inclusion of recently published studies cannot explain the fact that the present meta-analysis failed to replicate the reported lower effect size for psychotherapy than for pharmacotherapy (14) .
The larger effect of psychotherapy in the present meta-analysis than in the previous one is, in part, based on the use of different effect size measures. Because not controlling for unspecific changes in the control group could lead to an overestimation of treatment effects (16) , the present effect size measure is superior (45 , 46 , 48) to that used in the previous meta-analysis (14) . However, as the pharmacotherapeutic but not the psychotherapeutic studies used an active placebo, our effect size measure may overestimate the advantage of psychotherapy. Although the findings are limited by the study group sizes, when we focused on the five studies that compared psychotherapy and pharmacotherapy against an active placebo, there were no differences in effect sizes.
Several limitations specific to the present meta-analysis have to be considered. First, only five of the 89 studies compared both pharmacotherapy and psychotherapy against a control condition. It is possible that patients participating in studies of pharmacotherapy and psychotherapy differ in the motivation to initiate or adhere to a particular treatment. Given that changes in these and other unmeasured differences in treatment process characteristics may influence change in the treatment and control conditions, we partially controlled for them by computing improvement with the treatment condition relative to change in depression with the control condition. Second, the present meta-analysis is limited to studies of pharmacotherapy and psychotherapy. Comparisons of effects for other treatments (e.g., ECT) are needed. Third, given that study designs vary between pharmacotherapeutic and psychotherapeutic studies, comparisons have to be made with caution, particularly given that subjects in medication studies could be masked to treatment assignment. However, meta-analyses that compared open-label and double-blinded pharmacotherapeutic interventions did not show a significant effect of blinding on the effect size (16) , and the stronger effect of psychotherapy on clinician-rated depression in the current meta-analysis was observed in multivariate analyses that controlled for baseline and methodological differences. Fourth, long-term effects could not be investigated because of an insufficient number of studies. Fifth, very few studies were available on the treatment of patients 75 years and older, and the available data did not allow rigorous analyses of other demographic subgroups, defined, for example, in terms of race or ethnicity. Sixth, we focused on the clinical efficacy of treatments in controlled studies. Comparisons of the results obtained in ordinary clinical practice and comparisons of cost-effectiveness are needed. Seventh, although our empirical database was considerably larger than that of previous meta-analyses, there were still small numbers of studies for some comparisons, such as for changes in self-rated depression in studies with SSRIs or MAOIs. Eighth, we were not able to compare the effects of interventions for psychiatric inpatients versus primary care or specialty care medical patients. Nor were we able to examine effect size as a function of illness duration or age at onset. Ninth, some of the reviewed studies did not report exact effect sizes; in those cases, the effect size for p<0.05 or p<0.01 was used for our analysis. As the exact p level was probably often smaller than the reported level of significance, the estimated effect sizes underestimated the exact effect sizes.
Despite these limitations, two main conclusions regarding future research needs can be drawn. First, more controlled studies that randomly assign older depressed patients to pharmacotherapy, psychotherapy, and control conditions are needed. A subsequent meta-analysis of carefully controlled studies that include at least three arms would yield more definitive data than are currently available. Given the possibility that psychotherapy might be more effective for patients with minor depression or dysthymia, it would be particularly important for controlled studies to be conducted with patients across the spectrum of mood disorders, and not restricted to those with major depression. Our call for carefully controlled studies of monotherapies may sound quaint in this era of studies examining the effectiveness of multicomponent combination interventions, but these ambitious projects may not yield feasible, accessible services (51) , and the paucity of simple, carefully designed studies in which patients were randomly assigned to psychotherapy versus pharmacotherapy versus placebo is remarkable. Yet even this call for simpler, cleaner research comes with a caveat. Patients in psychotherapy studies cannot be meaningfully masked to treatment condition, a structurally equivalent placebo for psychotherapy does not exist, and medication is dispensed by a human being, who has the potential to touch patients’ lives, beyond the pure effect of the pill. Methodological or statistical innovations may be able to address if not resolve the inherent differences. Second, efforts are needed to improve the potency of both forms of treatments for depressed older adults. Fewer patients profited from treatment than would be desirable. According to clinical criteria, almost 50% were no longer depressed or had improved considerably at the end of treatment, as compared to 27% of control subjects. It is important to develop drugs with more potent effects and fewer contraindications and side effects. The potency of psychotherapy could be enhanced by identifying active ingredients and developing methods to enhance treatment motivation, adherence, and engagement.
With regard to clinical practice, our data suggest that, when available, both kinds of interventions can be offered to depressed older adults, as long as there are no contraindications. Even though the effect size for psychotherapy was higher in studies that included patients with minor depression or dysthymia, it would be premature to recommend psychotherapy over pharmacotherapy for these conditions. The difference in effect size, although statistically significant, was based on differences in the level of change in control group members, and very few studies directly compared pharmacotherapeutic and psychotherapeutic interventions against a control condition. The available data suggest that treatment choice for all depressive conditions should be based on contraindications, treatment availability, costs, and preferences of the older adults.
1. Gareri P, Falconi U, De Fazio P, De Sarro G: Conventional and new antidepressant drugs in the elderly. Prog Neurobiol 2000; 61:353–396Google Scholar
2. Hendrie HC, Callaham CM, Levitt EE: Prevalence rates of major depressive disorders: the effects of varying diagnostic criteria in an older primary care population. Am J Geriatr Psychiatry 1995; 3:119–131Google Scholar
3. Lyness JM, Caine ED, King DA, Cox C, Yoediono Z: Psychiatric disorders in older primary care patients. J Gen Intern Med 1999; 14:249–254Google Scholar
4. Beekman AT, Penninx BW, Deeg DJ, Ormel J, Bram AW, van Tilburg W: Depression and physical health in later life: results from the Longitudinal Aging Study Amsterdam. J Affect Disord 1997; 46:219–231Google Scholar
5. Woo J, Ho SC, Yu AL, Lau J: An estimate of long-term care needs and identification of risk factors for institutionalization among Hong Kong Chinese aged 70 years and over. J Gerontol A Biol Med Sci 2000; 55:M64–M69Google Scholar
6. Fröjdh K, Håkansson A, Karlsson I, Molarius A: Deceased, disabled or depressed: a population-based 6-year follow-up study of elderly people with depression. Soc Psychiatry Psychiatr Epidemiol 2003; 38:557–562Google Scholar
7. Henriksson MM, Marttunen MJ, Isometsa ET, Heikkinen ME: Mental disorders in elderly suicide. Int Psychogeriatr 1995; 7:275–286Google Scholar
8. Conwell Y, Duberstein PR, Caine ED: Risk factors for suicide in later life. Biol Psychiatry 2002; 52:193–204Google Scholar
9. Wagner HR, Burns BJ, Broadhead WE, Yarnall KS: Minor depression in family practice: functional morbidity, co-morbidity, service utilization and outcomes. Psychol Med 2000; 30:1377–1390Google Scholar
10. Waern M, Runeson BS, Allebeck P, Beskow J, Rubenowitz E, Skoog I, Wilhelmsson K: Mental disorder in elderly suicides: a case-control study. Am J Psychiatry 2002; 159:450–455Google Scholar
11. NIH Consensus Development Panel on Depression in Late Life: Diagnosis and treatment of depression in late life. JAMA 1992; 268:1018–1024Google Scholar
12. Lebowitz BD, Pearson JL, Schneider LS, Reynolds CF, Alexopoulos GS, Livingston M: Diagnosis and treatment of depression in late life: consensus statement update. JAMA 1997; 278:1186–1190Google Scholar
13. Charney DS, Reynolds CF III, Lewis L, et al: Depression and Bipolar Support Alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Arch Gen Psychiatry 2003; 60:664–672Google Scholar
14. Gerson S, Belin TR, Kaufman A, Mintz J, Jarvik L: Pharmacological and psychological treatments for depressed older patients: a meta-analysis and overview of recent findings. Harv Rev Psychiatry 1999; 7:1–28Google Scholar
15. Klawansky S: Meta-analysis on the treatment of depression in late life, in Diagnosis and Treatment of Depression in Late Life. Edited by Schneider LS, Reynolds CF. Washington, DC, American Psychiatric Press, 1997, pp 333–352Google Scholar
16. Khan A, Detke M, Khan SR, Mallinckrodt C: Placebo response and antidepressant clinical trial outcome. J Nerv Ment Dis 2003; 191:211–218Google Scholar
17. Rokke PD, Scogin F: Depression treatment preferences in younger and older adults. J Clin Geropsychol 1995; 1:243–258Google Scholar
18. Laidlaw K, Thompson LW, Dick-Siskin L, Gallagher-Thompson D: Cognitive Behavior Therapy With Older People. New York, John Wiley & Sons, 2003Google Scholar
19. Reynolds CF III, Miller MD, Pasternak RE, Frank E, Perel JM, Cornes C, Houck PR, Mazumdar S, Dew MA, Kupfer DJ: Treatment of bereavement-related major depressive episodes in later life: a controlled study of acute and continuation treatment with nortriptyline and interpersonal psychotherapy. Am J Psychiatry 1999; 156:202–208Google Scholar
20. Thompson LW, Gallagher D, Breckenridge JS: Comparative effectiveness of psychotherapies for depressed elders. J Consult Clin Psychol 1987; 55:385–390Google Scholar
21. Dhooper SS, Green SM, Huff MB, Austin-Murphy J: Efficacy of a group approach to reducing depression in nursing home elderly residents. J Gerontol Soc Work 1993; 20:87–100Google Scholar
22. Kraaij V, Arensman E, Spinhoven P: Negative life events and depression in elderly persons: a meta-analysis. J Gerontol B Psychol Sci Soc Sci 2002; 57(1):P87–P94Google Scholar
23. Wei W, Sambamoorthi U, Olfson M, Walkup JT, Crystal S: Use of psychotherapy for depression in older adults. Am J Psychiatry 2005; 162:711–717Google Scholar
24. Agency for Health Care Policy and Research: Depression in Primary Care: Detection, Diagnosis, and Treatment: AHCPR Publication 93-0552. Rockville, Md, Agency for Healthcare Research and Quality, 1993Google Scholar
25. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Google Scholar
26. Scogin F, McElreath L: Efficacy of psychosocial treatments for geriatric depression: a quantitative review. J Consult Clin Psychol 1994; 62:69–74Google Scholar
27. Cuijpers P: Psychological outreach programs for the depressed elderly: a meta-analysis of effects and dropouts. Int J Geriatr Psychiatry 1998; 13:41–48Google Scholar
28. Khan A, Leventhal RM, Khan SR, Brown WA: Severity of depression and response to antidepressants and placebo: an analysis of the Food and Drug Administration database. J Clin Psychopharmacol 2002; 22:40–45Google Scholar
29. Kemp BJ, Corgiat M, Gill B: Effects of brief cognitive-behavioral group psychotherapy on older persons with and without disabling illness. Behavior, Health, and Aging 1991–1992; 2:21–27Google Scholar
30. Small GW, Birkett M, Meyers BS, Koran LM: Impact of physical illness on quality of life and antidepressant response in geriatric major depression: Fluoxetine Collaborative Study Group. J Am Geriatr Soc 1996; 44:1220–1225Google Scholar
31. Oslin DW, Datto CJ, Kallan MJ, Katz IR: Association between medical comorbidity and treatment outcomes in late-life depression. J Am Geriatr Soc 2002; 50:823–828Google Scholar
32. Schweizer E, Rickels K, Hassman H, Garcia-Espana F: Buspirone and imipramine for the treatment of major depression in the elderly. J Clin Psychiatry 1998; 59:175–183Google Scholar
33. Guaiana G, Barbui C, Hotopf M: Amitriptyline versus other types of pharmacotherapy for depression. Cochrane Database Syst Rev 2003(2):CD004186Google Scholar
34. Engels GI, Vermey M: Efficacy of nonmedical treatments of depression in elders: a quantitative analysis. J Clin Geropsychol 1997; 3:17–35Google Scholar
35. Dobson KS: A meta-analysis of the efficacy of cognitive therapy for depression. J Consult Clin Psychol 1989; 57:414–419Google Scholar
36. Blazer D: Depression in Later Life. St Louis, CV Mosby, 1993Google Scholar
37. Entsuah A, Huang H, Thase ME: Response and remission rates in different subpopulations with major depressive disorders administered venlafaxine, selective serotonin reuptake inhibitors, or placebo. J Clin Psychiatry 2001; 62:869–877Google Scholar
38. Pampallona S, Bollini P, Tibaldi G, Kupelnick B: Combined pharmacotherapy and psychological treatment for depression: a systematic review. Arch Gen Psychiatry 2004; 61:714–719Google Scholar
39. Montgomery SA, Åsberg M: A new depression scale designed to be more sensitive to change. Br J Psychiatry 1979; 143:382–389Google Scholar
40. Beck AT, Steer RA: Manual of the Revised Beck Depression Inventory. San Antonio, Tex, Psychological Corp, 1979Google Scholar
41. Yesavage JA, Brink TL: Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 1983; 17:37–49Google Scholar
42. Guy W (ed): ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Washington, DC, US Department of Health, Education, and Welfare, 1976, pp 218–222Google Scholar
43. Jüni P, Witschi A, Bolsch R, Egger M: The hazards of scoring the quality of clinical trials for meta-analysis. JAMA 1999; 282:1054–1060Google Scholar
44. Hedges LV, Vevea JL: Fixed- and random-effects models in meta-analysis. Psychol Methods 1998; 3:486–504Google Scholar
45. Glass GV, McGaw B, Smith ML: Meta-Analysis in Social Research. Beverly Hills, Calif, Sage Publications, 1981Google Scholar
46. Mullen B: Advanced Basic Meta-Analysis. Hillsdale, NJ, Lawrence Erlbaum Associates, 1989Google Scholar
47. Hedges LV: Distribution theory for Glass’s estimator of effect size and related estimators. J Educational Statistics 1981; 6:107–128Google Scholar
48. Rosenthal R: Meta-Analytic Procedures for Social Research. Beverly Hills, Calif, Sage Publications, 1991Google Scholar
49. Fleiss JL: Statistical Methods for Rates and Proportions, 2nd ed. New York, John Wiley & Sons, 1981Google Scholar
50. Cohen J: A power primer. Psychol Bull 1992; 112:155–159Google Scholar
51. Lebowitz BD: Clinical trials in late life: new science in old paradigms. Gerontologist 2004; 44:452–458Google Scholar