Sticks, Stones, and Hurtful Words: Relative Effects of Various Forms of Childhood Maltreatment
Abstract
Objective: Childhood maltreatment is an important psychiatric risk factor. Research has focused primarily on the effects of physical abuse, sexual abuse, or witnessing domestic violence. Parental verbal aggression has received little attention as a specific form of abuse. This study was designed to delineate the impact of parental verbal aggression, witnessing domestic violence, physical abuse, and sexual abuse, by themselves and in combination, on psychiatric symptoms. Method: Symptoms and exposure ratings were collected from 554 subjects 18–22 years of age (68% female) who responded to advertisements. The Verbal Abuse Questionnaire was used to assess exposure to parental verbal aggression. Outcome measures included dissociation and symptoms of “limbic irritability,” depression, anxiety, and anger-hostility. Comparisons were made by using effect sizes. Results: Verbal aggression was associated with moderate to large effects, comparable to those associated with witnessing domestic violence or nonfamilial sexual abuse and larger than those associated with familial physical abuse. Exposure to multiple forms of maltreatment had an effect size that was often greater than the component sum. Combined exposure to verbal abuse and witnessing domestic violence had a greater negative effect on some measures than exposure to familial sexual abuse. Conclusions: Parental verbal aggression was a potent form of maltreatment. Exposure to multiple forms of abuse was associated with very large effect sizes. Most maltreated children had been exposed to multiple types of abuse, and the number of different types is a critically important factor.
Childhood abuse has been the focus of increasing concern, particularly when it is sexual or severely physical. This has been further reinforced by studies that suggest that abuse produces enduring effects on brain development (1) . While sexual abuse has come under intense scrutiny as a psychiatric risk factor, emotional maltreatment may be a more elusive and insidious problem. Emotional abuse encompasses several forms of childhood maltreatment, such as the witnessing of domestic violence and exposure to verbal aggression (2) . Generally, exposure to verbal aggression has received little attention as a specific form of abuse, although it may be at least as important as witnessing domestic violence. In one large national study, Vissing et al. (3) found that 63% of American parents reported one or more instances of verbal aggression, such as swearing at and insulting their child. Children who were the target of frequent verbal aggression exhibited higher rates of physical aggression, delinquency, and interpersonal problems than other children (3) .
Maternal verbal abuse during childhood has been associated with a markedly higher risk for development of borderline, narcissistic, obsessive-compulsive, and paranoid personality disorders (4) . These associations remained significant after control for temperament, physical abuse, sexual abuse, neglect, parental psychopathology, and co-occurring psychiatric disorders (4) . Verbal abuse may also have more lasting consequences than other forms of abuse (5) and, in combination with physical abuse and neglect, produce the most dire outcome (6) . However, child protective service agencies, doctors, and lawyers are most concerned about the impact and prevention of physical or sexual abuse (7 , 8) .
Co-occurrence of multiple types of childhood abuse is known to be common, with reported rates of co-occurrence ranging from 3% to 55% (9) . When the effects of exposure to multiple forms of adversity are considered, it appears that the greater the number of forms experienced, the more severe the subsequent pathology (9 , 10) .
We sought to answer two questions. First, is there a discernible impact of exposure to childhood verbal aggression in the absence of physical abuse, sexual abuse, or exposure to domestic violence? Second, what are the relative psychiatric consequences of childhood exposure to verbal aggression, witnessing domestic violence, physical abuse, and sexual abuse, experienced either alone or in combination? Dissociation and “limbic irritability” were selected as two primary variables for analysis, as previous research had shown robust correlations between dissociation and hippocampal size (11) and between limbic irritability and blood flow to the cerebellar vermis as assessed with functional magnetic resonance imaging (12) . We also assessed the effects of exposure on symptoms of depression, anxiety, and anger-hostility.
Method
Subjects
Detailed ratings of symptoms and exposure history were collected from 554 young adults who responded to advertisements requesting healthy subjects or individuals with a history of an unhappy childhood. They ranged in age from 18 to 22 years (mean=19.8, SD=1.4 years); 378 were women, and 176 were men. After complete description of the study to the subjects, written informed consent was obtained. Most of the study subjects (73%) were white, 6% were black, 6% were Hispanic, 10% were Asian, 1% were Native American, and 4% were from other ethnic groups.
Assessments
Exposure to verbal aggression
The Verbal Abuse Questionnaire consists of 15 items that cover the key components of verbal abuse—scolding, yelling, swearing, blaming, insulting, threatening, demeaning, ridiculing, criticizing, belittling, etc. In a separate group of 48 college students, the questionnaire showed high internal consistency as applied to both maternal and paternal behaviors (Cronbach alphas, 0.98 and 0.94, respectively). Scores from the questionnaires for maternal and paternal verbal abuse were averaged as a measure of childhood verbal abuse. More detailed discussion of scale development and psychometric properties is available from the authors.
The Verbal Abuse Questionnaire provides a continuous measure of exposure, which correlated strongly with all of our symptom measures. However, for comparison with other forms of maltreatment that were dichotomized into “presence” or “absence,” we selected a cutoff score to identify subjects exposed to a substantial degree of verbal aggression. From the subjects with no history of physical or sexual abuse a cutoff score was selected that designated the top 10% of scores. We used this score (>40) to delineate a level of verbal aggression that was unusually high but not rare. This upper 10% criterion had face validity, as this also corresponded in this group to the percentage of subjects who endorsed a history of exposure to domestic violence. The effect sizes for the Verbal Abuse Questionnaire as a continuous measure were always greater than the effect sizes for the dichotomous variable, but cutoff scores greater than 40 provided effect sizes that were in close agreement (70%–80% as large).
Exposure to other abuse and trauma
History of exposure to physical abuse was obtained by self-report in response to the following question: “Have you ever been physically hurt or attacked by someone such as husband, parent, another family member, or friend (for example, have you ever been struck, kicked, bitten, pushed, or otherwise physically hurt)?” If so, the subjects were asked to provide information on their relationship to this individual, the number of times they were hurt, ages at initiation and termination of these episodes, whether the abuse received or should have received medical attention, and whether the abuse resulted in permanent injuries or scars. An individual was classified as having experienced physical abuse if he or she reported any episode of inflicted physical injury that received or should have received medical treatment or resulted in permanent injury or if there were at least four reported episodes of what he or she felt were less serious attacks.
Individuals were classified as having experienced sexual abuse if they responded affirmatively to the following question: “Have you ever been forced into doing more sexually than you wanted to do or were too young to understand? (By “sexually” we mean being forced against your will into contact with the sexual parts of your body or his or her body.)” They were also asked to provide information on their relationship to this individual, the number of times they were forced, ages at first and last abuse, and whether or not they felt terrified or had their life or another person’s life threatened.
History of exposure to domestic violence was assessed by using the question “Have you ever witnessed serious domestic violence?”
Limbic irritability
The Limbic System Checklist-33 (13) was created to evaluate the frequency with which subjects experience symptoms often encountered as phenomena of ictal temporal lobe epilepsy, as described by Spiers et al. (14) . These items consist of paroxysmal somatic disturbances, brief hallucinatory events, visual phenomena, automatism, and dissociative experiences. Psychometric studies showed that the Limbic System Checklist-33 has high test-retest reliability (r=0.92, N=16) (13) . Scores were low in normal comparison subjects (<10) and higher in patients with documented temporal lobe epilepsy (>23). Scores on the Limbic System Checklist-33 are dramatically influenced by abuse history (13) , more so than any other variable we have examined (12) .
Psychiatric symptoms
The Dissociative Experience Scale (15) consists of 28 questions that assess the frequency of various dissociative experiences. Scores on each item range from 0 to 100, and they are averaged to provide an index score. Total scores under 20 capture most healthy subjects and patient groups with no appreciable dissociative symptoms.
Self-ratings of other psychiatric symptoms were obtained by using Kellner’s Symptom Questionnaire (16) . This is a 92-item yes/no questionnaire used to elicit ratings of depression, anxiety, anger-hostility, and somatic complaints. It was developed to detect response to psychotropic medications and is sensitive to subtle differences from normal.
Data Analysis
The strength of the association between maltreatment history and self-report symptom scores was assessed by calculating the effect sizes and 95% confidence intervals (CIs) for the differences between subjects who had no exposure to maltreatment and subjects exposed to the different maltreatment categories. Effect size is a more valuable measure for assessing the impact of an experience than the p value, which is strongly affected by group size. Cohen’s d′ values of 0.2, 0.5, and 0.8 are usually interpreted to represent small, medium, and large effects, respectively (17) .
Effect size was used to highlight the differences between subjects exposed to different forms of abuse and healthy comparison subjects. Analysis of variance provided a single statistical measure for the effect of exposure to the various categories of maltreatment on the dependent variables. Finally, a few planned statistical comparisons germane to the main focus of the study were made in order to understand the significant omnibus F values. These tests were done to address different specific types of exposure: 1) emotional abuse versus sexual abuse, 2) emotional abuse versus physical abuse, 3) verbal abuse versus witnessing domestic violence, 4) the combination of verbal abuse and witnessing domestic violence versus familial sexual abuse, and 5) multiple categories of abuse.
Results
Effects on Limbic Irritability
As seen in Figure 1 , there were robust effects of each of the five broad abuse categories (emotional only, sexual only, physical only, any two, all three) on ratings on the Limbic System Checklist-33 (F=21.46, df=5, 542, p<10 –15 , n 2 =0.149). There was no effect of gender on this measure (F=1.13, df=5, 542, p>0.30). Subjects in all of the broad abuse categories had ratings that were higher than those of subjects who had never experienced maltreatment. Emotional abuse had a moderately large effect on the rating of limbic irritability (d′=0.703, 95% CI=0.548–0.858; t=4.95, df=300, p<10 –5 ). Subjects who were exposed only to emotional abuse had ratings that were as high as those of subjects who were exposed only to physical abuse (t=0.72, df=85, p>0.40) or only to sexual abuse (t=–0.83, df=102, p>0.40).
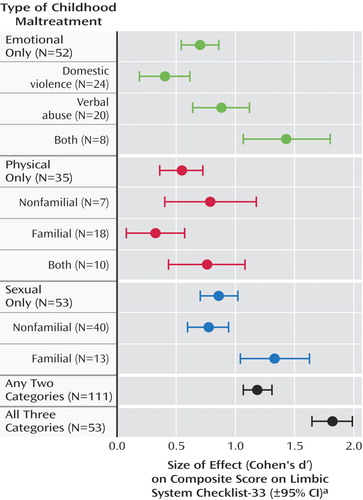
a Based on comparison of subjects with each category of maltreatment and a comparison group (N=250) with no history of exposure to abuse or other form of early adversity. The Limbic System Checklist-33 (13) was created to evaluate the frequency with which subjects experience symptoms often encountered as phenomena of ictal temporal lobe epilepsy.
Subjects who were exposed to two different categories of abuse had higher scores for limbic irritability than subjects exposed to emotional abuse only (t=2.65, df=161, p<0.01) or physical abuse only (t=3.07, df=144, p<0.003). Subjects who reported exposure to all three categories of abuse had significantly higher scores than those exposed to any single category of abuse.
Limbic irritability was also significantly affected by exposure to any of the more specific types of abusive experience within each broad abuse category (verbal, nonfamilial sexual, etc.) (F=4.44, df=8, 372, p<10 –4 ). Exposure to verbal abuse had a relatively large effect size (d′=0.876, 95% CI=0.641–1.111), whereas witnessing domestic violence had a moderate effect size (d′=0.403, 95% CI=0.189–0.617), although this difference could have occurred by chance (t=1.49, df=42, p=0.15). It is interesting that combined exposure to verbal abuse and witnessing domestic violence had a very large effect size (d′=1.428, 95% CI=1.063–1.793), which was essentially equal to the effect size of familial sexual abuse (d′=1.333, 95% CI=1.043–1.623).
Effects on Dissociative Experiences
As seen in Figure 2 , there were robust effects of the broad abuse categories on dissociation (F=13.63, df=5, 540, p<10 –11 , n 2 =0.105), and they did not differ between genders (F=1.88, df=5, 540, p<0.10). Emotional abuse had a large effect on Dissociative Experience Scale ratings (d′=0.910, 95% CI=0.753–1.067). Exposure to physical abuse and sexual abuse had moderate effects (d′=0.533, 95% CI=0.351–0.715, and d′=0.659, 95% CI=0.505–0.813, respectively). Exposure to two different broad categories of abuse was associated with a large effect size (d′=0.902, 95% CI=0.783–1.021) that was similar to the effect size for emotional abuse. Exposure to all three categories was associated with a very large effect size (d′=1.431, 95% CI=1.269–3.024) that was greater than the effect of exposure to physical abuse (t=2.97, df=86, p<0.005) or sexual abuse (t=2.55, df=104, p<0.02) and marginally greater than the effect of emotional abuse alone (t=1.92, df=103, p=0.06).
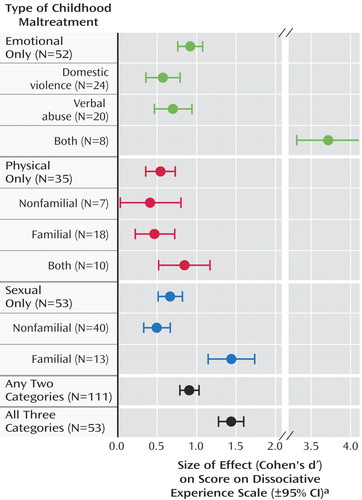
a Based on comparison of subjects with each category of maltreatment and a comparison group (N=249) with no history of exposure to abuse or other form of early adversity.
Exposure to verbal abuse alone and witnessing of domestic violence had moderately strong effects on dissociation ratings (d′=0.690, 95% CI=0.456–0.924, and d′=0.564, 95% CI=0.349–1.343, respectively). Subjects exposed to both verbal abuse and domestic violence (but no other form of maltreatment) had Dissociative Experience Scale scores 4.5 times as high as those of the nonabused subjects (d′=3.719, 95% CI=3.324–4.114). In this limited study group, the effect of combined exposure to verbal abuse and witnessing domestic violence had more impact on dissociation ratings than exposure to familial sexual abuse (t=2.42, df=19, p=0.02).
Effects on Anxiety Symptoms
As seen in Figure 3 , there were robust effects of the broad abuse categories on anxiety (F=14.36, df=5, 541, p<10 –12 , n 2 =0.109), which did not differ between genders (F=1.53, df=5, 541, p<0.20). Emotional abuse alone and sexual abuse alone had moderate effects (d′=0.510, 95% CI=0.356–0.664, and d′=0.684, 95% CI=0.530–0.838, respectively). Exposure to physical abuse alone exerted only a small and nonsignificant effect (d′=0.158, 95% CI=–0.023–0.339; t=0.81, df=283, p=0.16). Exposure to two different broad categories of abuse was associated with a large effect size (d′=0.832, 95% CI=0.714–0.950), and exposure to all three abuse categories was associated with a very large effect size (d′=1.429, 95% CI=1.267–1.591) that was significantly greater than the effect of exposure to any single category of abuse.
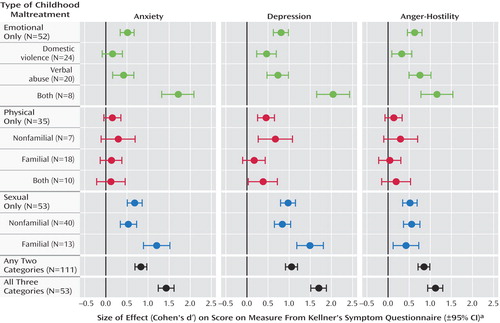
a Based on comparison of subjects with each category of maltreatment and a comparison group (N=250) with no history of exposure to abuse or other form of early adversity. Kellner’s Symptom Questionnaire (16) is a yes/no self-report questionnaire that is sensitive to subtle differences from normal.
Exposure to verbal abuse alone and witnessing domestic violence had relatively weak effects on anxiety ratings (d′=0.422, 95% CI=0.189–0.655, and d′=0.158, 95% CI=–0.056–0.372, respectively). Combined exposure to verbal abuse and witnessing domestic violence had a greater than additive effect (d′=1.718, 95% CI=1.351–2.085). Subjects exposed to both verbal abuse and domestic violence (but no other forms) had anxiety scores that were 2.2 times as high as those of the nonabused subjects (t=4.76, df=256, p<10 –6 ). The effect of combined exposure to verbal abuse and witnessing of domestic violence was as great as the effect of exposure to familial sexual abuse (d′=1.204, 95% CI=0.915–1.493).
Effects on Depression Symptoms
There were robust effects of the broad abuse categories on depression (F=15.91, df=5, 541, p<10 –12 , n 2 =0.121), and they were consistent across genders (F=0.58, df=5, 541, p>0.70). Emotional abuse alone and sexual abuse alone had large effects (d′=0.804, 95% CI=0.648–0.960, and d′=0.971, 95% CI=0.815–1.127, respectively). Exposure to physical abuse alone exerted a moderate effect (d′=0.452, 95% CI=0.271–0.633). Exposure to all three categories exerted a very large effect (d′=1.696, 95% CI=1.530–1.862), which was significantly greater than the effect of exposure to any single category of abuse.
Exposure to verbal abuse alone and witnessing of domestic violence had moderately strong effects on depression (d′=0.730, 95% CI=0.496–0.964, and d′=0.463, 95% CI=0.249–0.677, respectively). Combined exposure to verbal abuse and witnessing domestic violence had a greater than additive deleterious effect (d′=2.042, 95% CI=1.672–2.412). Subjects who were exposed to this combined type of emotional abuse had depression scores that were 2.8 times as high as those of the nonabused subjects (t=5.66, df=256, p<10 –8 ). The effect of combined exposure to verbal abuse and witnessing domestic violence was greater than or equal to the effect of exposure to familial sexual abuse (d′=1.494, 95% CI=1.202–1.786) or exposure to all three categories of abuse (d′=1.696, 95% CI=1.530–1.862).
Effects on Symptoms of Anger-Hostility
There were robust effects of the broad abuse categories on anger-hostility (F=15.18, df=5, 541, p<10 –12 , n 2 =0.119). Emotional abuse alone and sexual abuse alone exerted moderate effects (d′=0.630, 95% CI=0.475–0.785, and d′=0.520, 95% CI=0.367–0.673, respectively). Physical abuse alone exerted only a weak and not statistically significant effect (d′=0.131, 95% CI=–0.049–0.311; t=0.73, df=283, p>0.40) and was eclipsed by the effects of exposure to emotional abuse (t=2.08, df=85, p=0.04). Combined exposure to any two categories of abuse had a large effect size (d′=0.851, 95% CI=0.733–0.969), and exposure to all three categories had an even larger effect size (d′=1.121, 95% CI=0.963–1.279).
Exposure to verbal abuse alone had a moderately strong effect on anger-hostility (d′=0.758, 95% CI=0.523–0.993), and these subjects had scores that were 58% greater than those of the nonabused individuals (t=3.25, df=268, p<0.002). Witnessing domestic violence had a relatively weak effect on these symptoms (d′=0.327, 95% CI=0.113–0.541), and the scores of subjects with this childhood experience were only 25% higher than those of the comparison subjects (t=1.53, df=272, p=0.13). Combined exposure to verbal abuse and witnessing domestic violence had an additive deleterious effect (d′=1.156, 95% CI=0.793–1.519). The effect of combined exposure to verbal abuse and domestic violence was at least as great as the effect of exposure to familial sexual abuse (d′=0.427, 95% CI=0.142–0.712) and was comparable to the effect of exposure to all three types of abuse (d′=1.121, 95% CI=0.963–1.279).
History of Treatment
The impact of multiple exposures to different forms of maltreatment was also mirrored in the percentage of subjects reporting a past history of psychiatric treatment (χ 2 =40.4, df=5, p<10 –7 ). Previous psychiatric care was reported by 3% of the subjects with no history of maltreatment, 0% of those with a history of physical abuse alone, 8% of those who were exposed to emotional maltreatment, and 9% of those who were exposed to sexual abuse. In contrast, 18% of the subjects exposed to any two types of maltreatment and 25% of those exposed to all three categories reported a past history of psychiatric care.
Discussion
Childhood exposure to parental verbal aggression was associated, by itself, with moderate to large effects on measures of dissociation, limbic irritability, depression, and anger-hostility. Exposure to verbal aggression was associated with numerically larger effects on scores on the Limbic System Checklist-33 and Kellner Symptom Questionnaire than was exposure to domestic violence, although these differences could have occurred by chance. Combined exposure to verbal abuse and witnessing of domestic violence was associated with extraordinarily large adverse effects, particularly on dissociation. This finding is consonant with studies that suggest that emotional abuse may be a more important precursor of dissociation than is sexual abuse (18) .
These findings raise the possibility that exposure to verbal aggression may be a stressor that affects the development of certain vulnerable brain regions in susceptible individuals, resulting in psychiatric sequelae (1) . Alternatively, exposure to verbal aggression in childhood may put into force a powerful negative model for interpersonal communication, which is then incorporated as a behavioral response in future relationships. Toth and Cicchetti (19) proposed a cascade of interpersonal events in maltreated children that begins with insecure attachment relationships, moves to negative representational models of the self and of the self in relation to others, and eventuates in impaired perceived competence, poorer social functioning, and lowered self-esteem. Similarly, Crittenden (20) found that exposure to abuse and neglect affects attachment patterns and coping strategies. These possibilities are not mutually exclusive, and each could contribute in important ways.
In the present study group, with our definitions of abuse it appeared that emotional maltreatment was more closely associated with psychiatric sequelae than was physical abuse. It is possible that we would have observed a more deleterious effect of physical abuse if we had adopted a stricter definition. We are conducting further studies with additional measures to test this possibility.
Combined exposure to different categories of abusive experiences often equaled or exceeded the impact of exposure to familial sexual abuse. This is of great importance as it suggests that combined exposure to less blatant forms of abuse may be just as deleterious as the most egregious acts we confront. Fifty-nine percent of the subjects in the present study with a history of maltreatment had been exposed to more than one type of abuse.
These findings are concordant with the results of a large-scale epidemiological study designed to assess the prevalence and health impact of early trauma experiences, the Adverse Childhood Experiences Study (21) . All of the publications resulting from this work point to a relationship between self-reported early exposure to adversity and subsequent problems, including depression (9) , attempted suicide (10) , substance abuse, and an array of medical disorders. A dose-response relationship was observed such that the greater the number of childhood adverse experiences, the greater the risk for a negative health outcome in adulthood. Macfie et al. (22) also reported that exposure to multiple forms of trauma, along with severity and chronicity, was predictive of subsequent psychopathology.
The mechanisms underlying the additive or synergistic effects of exposure to different types of abuse are unknown. It is possible that an additive or greater effect may emerge because abuse at home could prevent a child from seeking help or reassurance from his or her parents when confronted with abuse outside the home. Alternatively, individuals exposed to different types of abuse may experience them at different developmental stages, which would increase the likelihood that abuse occurred during key sensitive periods. A third hypothesis is that exposure to multiple types of abuse increases the frequency of exposure and that, in addition to genetic factors, a certain minimal number of exposures is necessary for the development of an adverse outcome (23) .
The present study is limited by our reliance on self-reports. How do we know if the participants’ abuse histories are valid? We are sensitized to this issue by the debate surrounding false or repressed memories. However, the issue of repressed memories is unlikely to be a significant factor in this research protocol as the events reported were current memories and the study provided no incentive for the subjects to fabricate a history of abuse, as they were never informed of our screening criteria. While we are concerned about potential fabrications, research suggests that the overall bias is in the opposite direction—individuals are more likely to minimize or deny their adverse childhood experiences (24) . Positive reports of maltreatment can be corroborated (25) . While retrospective self-report studies constitute the vast bulk of the literature on the effects of early abuse on adults, prospective studies that confirm its impact are emerging (23 , 26) .
We cannot exclude the possibility that individuals who have a relatively high degree of current psychiatric symptoms may report aspects of their childhood in a more negative light than do individuals who are free of such symptoms (27) . It is also possible that exposure to familial emotional, physical, or sexual abuse is highest in families with mental illness, and thus, genetic factors could contribute to the higher symptom scores we observed in our subjects with exposure to familial abuse. Studies of twins discordant for childhood sexual abuse provide a potentially powerful means of assessing the respective contribution of childhood sexual abuse while controlling for genetic vulnerabilities and shared environment. Kendler et al. (28) reported that the twins with childhood sexual abuse had an overall increased risk for major depression and a substantially increased sensitivity to the depressogenic effects of other stressful life events.
We have used the term “association” to describe the relationship between symptom ratings and retrospective self-reports of abuse. While we hypothesize that there may be a causal relationship, there are other legitimate ways to interpret the data. Indeed, it may be the case that the relationship between abuse reports and symptoms is due to a combination of direct effects of early stress, recall bias, and increased genetic load.
Another limitation is that our probe question for exposure to domestic violence was very broad, and so the definition of domestic violence may not be comparable to definitions in studies that specifically focused on observations of mothers being battered. We know from more detailed assessment of 54 individuals (16 men and 38 women, mean age=20.8 years, SD=1.1) who responded positively to this general probe question on the witnessing of serious domestic violence that 65% had witnessed their mothers being threatened or assaulted, 43% had witnessed siblings being threatened or assaulted, and 17% had witnessed threats or assaults of their fathers. Further, 24% had witnessed the severe beating of the person involved. The effect of exposure to domestic violence might have been greater had we used a more specific and limited definition.
Finally, representative sampling techniques were not used. This means that the impact of maltreatment observed may not generalize to other groups. Sixty-five subjects from the group were recruited for additional studies and went through structured diagnostic interviews, neuropsychological testing, and imaging protocols. They had an average Hollingshead two-factor socioeconomic status of 4.0 (SD=0.8) (upper middle class).
In all likelihood, the overall degree of psychopathology was probably lower in our healthy, predominantly collegiate study group than would be found in a representative sample, although the relative effects of exposure to different forms of abuse should generalize to other populations.
Verbal abuse was associated with effect sizes that were numerically greater than those associated with witnessing domestic violence or familial physical abuse. However, witnessing domestic violence and physical abuse can qualify as a category A(1) traumatic event necessary for the DSM-IV diagnosis of posttraumatic stress disorder (PTSD), while exposure to verbal abuse cannot. We wonder, particularly in children, if threats to one’s mental integrity and sense of self can also be traumatizing. Bremner et al. (29) made an interesting observation: “Surprisingly, emotional abuse items, such as being often shouted at, appeared to have severe consequences in terms of risk for PTSD.” The specific role of verbal abuse in the development of PTSD has yet to be determined. Research is needed to evaluate whether such exposure is causative or whether it contributes to the development of PTSD by amplifying the effects of exposure to traumatic events.
It will likely come as no surprise to clinicians that parental verbal aggression is associated with psychiatric symptoms. The potential effects of exposure to verbal abuse, by itself and in combination with other forms of abuse, need to be carefully considered in research studies focusing on the effects of early experience. Individuals interested in the welfare of maltreated children should not underestimate the consequences of verbal abuse. Finally, careful attention should be given to the number of different types of traumatic experiences a child was exposed to, as this may be even more critical than the specific type of abuse.
1. Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM: The neurobiological consequences of early stress and childhood maltreatment. Neurosci Biobehav Rev 2003; 27:33–44Google Scholar
2. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L: Validity of the childhood trauma questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry 1997; 36:340–348Google Scholar
3. Vissing YM, Straus MA, Gelles RJ, Harrop JW: Verbal aggression by parents and psychosocial problems of children. Child Abuse Negl 1991; 15:223–238Google Scholar
4. Johnson JG, Cohen P, Smailes EM, Skodol AE, Brown J, Oldham JM: Childhood verbal abuse and risk for personality disorders during adolescence and early adulthood. Compr Psychiatry 2001; 42:16–23Google Scholar
5. Ney PG: Does verbal abuse leave deeper scars: a study of children and parents. Can J Psychiatry 1987; 32:371–378Google Scholar
6. Ney PG, Fung T, Wickett AR: The worst combinations of child abuse and neglect. Child Abuse Negl 1994; 18:705–714Google Scholar
7. Manning C, Cheers B: Child abuse notification in a country town. Child Abuse Negl 1995; 19:387–397Google Scholar
8. Saulsbury FT, Campbell RE: Evaluation of child abuse reporting by physicians. Am J Dis Child 1985; 139:393–395Google Scholar
9. Edwards VJ, Holden GW, Felitti VJ, Anda RF: Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the Adverse Childhood Experiences Study. Am J Psychiatry 2003; 160:1453–1460Google Scholar
10. Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH: Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA 2001; 286:3089–3096Google Scholar
11. Stein MB: Hippocampal volume in women victimized by childhood sexual abuse. Psychol Med 1997; 27:951–959Google Scholar
12. Anderson CM, Teicher MH, Polcari A, Renshaw PF: Abnormal T2 relaxation time in the cerebellar vermis of adults sexually abused in childhood: potential role of the vermis in stress-enhanced risk for drug abuse. Psychoneuroendocrinology 2002; 27:231–244Google Scholar
13. Teicher MH, Glod CA, Surrey J, Swett C Jr: Early childhood abuse and limbic system ratings in adult psychiatric outpatients. J Neuropsychiatry Clin Neurosci 1993; 5:301–306Google Scholar
14. Spiers PA, Schomer DL, Blume HW, Mesulam MM: Temporolimbic epilepsy and behavior, in Principles of Behavioral Neurology. Edited by Mesulam MM. Philadelphia, FA Davis, 1985, pp 289–326Google Scholar
15. Bernstein EM, Putnam FW: Development, reliability and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727–735Google Scholar
16. Kellner R: A symptom questionnaire. J Clin Psychiatry 1987; 48:268–273Google Scholar
17. Cohen J: Statistical Power Analysis for the Behavioral Sciences. New York, Academic Press, 1988Google Scholar
18. Sar V, Tutkun H, Alyanak B, Bakim B, Baral I: Frequency of dissociative disorders among psychiatric outpatients in Turkey. Compr Psychiatry 2000; 41:216–222Google Scholar
19. Toth SL, Cicchetti D: Patterns of relatedness, depressive symptomatology, and perceived competence in maltreated children. J Consult Clin Psychol 1996; 64:32–41Google Scholar
20. Crittenden PM: Children’s strategies for coping with adverse home environments: an interpretation using attachment theory. Child Abuse Negl 1992; 16:329–343Google Scholar
21. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS: Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998; 14:245–258Google Scholar
22. Macfie J, Cicchetti D, Toth SL: Dissociation in maltreated versus nonmaltreated preschool-aged children. Child Abuse Negl 2001; 25:1253–1267Google Scholar
23. Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R: Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003; 301:386–389Google Scholar
24. Brewin CR, Andrews B, Gotlib IH: Psychopathology and early experience: a reappraisal of retrospective reports. Psychol Bull 1993; 113:82–98Google Scholar
25. Bifulco A, Brown GW, Lillie A, Jarvis J: Memories of childhood neglect and abuse: corroboration in a series of sisters. J Child Psychol Psychiatry 1997; 38:365–374Google Scholar
26. Noll JG, Trickett PK, Susman EJ, Putnam FW: Sleep disturbances and childhood sexual abuse. J Pediatr Psychol 2005; 0(June 15):401 (epub ahead of print)Google Scholar
27. Pope HG Jr, Hudson JI: Does childhood sexual abuse cause adult psychiatric disorders? essentials of methodology. J Psychiatry Law 1995; 23:363–381Google Scholar
28. Kendler KS, Kuhn JW, Prescott CA: Childhood sexual abuse, stressful life events and risk for major depression in women. Psychol Med 2004; 34:1475–1482Google Scholar
29. Bremner JD, Vermetten E, Mazure CM: Development and preliminary psychometric properties of an instrument for the measurement of childhood trauma: the Early Trauma Inventory. Depress Anxiety 2000; 12:1–12Google Scholar



