Ten-Year Prospective Follow-Up Study of the Naturalistic Course of Dysthymic Disorder and Double Depression
Abstract
Objective: The purpose of this study was to describe the 10-year course and outcome of dysthymic disorder. Method: The authors conducted a naturalistic, prospective, longitudinal follow-up of 97 adults with early-onset dysthymic disorder and 45 adults with nonchronic major depressive disorder selected from consecutive admissions to several outpatient facilities. Follow-up data were obtained for 90% of the cohort. Assessments were conducted at baseline, 30, 60, 90, and 120 months. Measures included the Longitudinal Interval Follow-Up Evaluation and the Hamilton Depression Rating Scale. Results: The Kaplan-Meier estimated recovery rate from dysthymic disorder was 73.9%, with a median time to recovery of 52 months. Among patients who recovered, the estimated risk of relapse into another period of chronic depression was 71.4%. Chronic depressive relapses took a variety of forms and were not limited to dysthymia. Nonetheless, the distinction between chronic and nonchronic forms of depression was relatively stable over the follow-up period. Mixed-effects models indicated that patients with dysthymic disorder experienced a significantly slower rate of improvement in symptoms over time and exhibited significantly greater depression at the 10-year point, compared to patients with nonchronic major depression. Conclusions: Dysthymic disorder has a protracted course and is associated with a high risk of relapse. The nature of chronic depressive episodes varies over time within individuals, indicating that the various manifestations of chronic depression in DSM-IV do not represent distinct disorders. However, the distinction between chronic and nonchronic forms of depression is relatively stable and may provide a useful basis for subtyping in genetic and neurobiological research.
Dysthymic disorder is a chronic, low-grade depressive condition that affects as many as 6% of individuals in the community (1) and 36% of outpatients in mental health settings (2) . Although dysthymic disorder is characterized by mild to moderate symptoms, more than 75% of individuals with dysthymic disorder have exacerbations that meet the criteria for a major depressive episode, a phenomenon known as “double depression” (3) .
Despite the central role of chronicity in defining dysthymic disorder, there are few data on its long-term course. With the exception of one study of pediatric patients (4) , all longitudinal studies of dysthymic disorder have had follow-up periods of 2 years or less (5 – 11) . The limited duration of follow-up constitutes an important gap in the research on dysthymic disorder, as it is difficult to determine the rates and timing of recovery and relapse in chronic disorders and to examine their stability over time without long-term follow-up.
In an earlier paper, we reported data from the first 5 years of a 10-year prospective follow-up study of the naturalistic course of outpatients with early-onset dysthymic disorder (many of whom had double depression) and a “near-neighbor” comparison group of outpatients with nonchronic major depressive disorder (12) . We found that the estimated 5-year recovery rate from dysthymic disorder was 53% and that there was a 45% chance of relapse into another chronic depressive episode. In addition, patients with dysthymic disorder and double depression experienced significantly higher levels of depression and spent more time in depressive episodes and less time fully recovered than patients with nonchronic major depressive disorder.
This article presents the major findings from the full 10-year study. We addressed three issues. First, by doubling the length of follow-up, we were able to provide more complete data on the rates and timing of recovery and relapse in dysthymic disorder. Second, we examined the specificity of chronic depressive relapses in dysthymic disorder (i.e., whether patients with relapses had relapses of dysthymic disorder or of other forms of chronic depression, such as chronic major depressive disorder). This issue is important in light of recent studies questioning the distinction between various forms of chronic depression (13 – 15) . Third, recent studies have reported that chronic and episodic depressions exhibit different patterns of familial aggregation, suggesting that they may represent distinct subtypes (13 , 16) . However, if this distinction is to be useful for genetic and neurobiological studies, it should be relatively stable over time. Hence, we extended our previous comparison of the course of chronic versus episodic depression from 5 to 10 years with the aim of determining the long-term stability of the distinction between chronic and episodic depression.
Method
Subjects
The study subjects and methods have been described previously (12 , 16) . The initial study group included 97 outpatients with DSM-III-R early-onset dysthymic disorder (with or without a superimposed major depressive disorder episode) and 45 outpatients with nonchronic major depressive disorder. We focused on the early-onset (onset at age <21 years) subtype, because it is the prototypical form of dysthymic disorder (17 , 18) . Patients with nonchronic major depressive disorder were required to have had onset of the disorder before age 35 years to better match the dysthymic disorder patients in demographic characteristics and age at onset of disorder. The patients were 18–60 years old and were selected from consecutive admissions to the Stony Brook University Outpatient Psychiatry Department and Psychological Center. Several patients were also referred from the University Counseling Center and a community mental health center.
At least one follow-up was completed with 87 (89.7%) patients with dysthymic disorder and 40 (88.9%) patients with nonchronic major depressive disorder. Of the 127 patients completing at least one follow-up, seven (5.5%) completed two assessments, 22 (17.3%) completed three assessments, and 88 (69.3%) completed all four assessments. The mean length of follow-up was 112.4 months (SD=24.2) for the dysthymic disorder patients and 114.4 months (SD=20.0) for nonchronic major depressive disorder patients (t=0.65, df=125, p=0.65). Dysthymic disorder patients who did and did not complete at least one follow-up did not differ on any of the demographic and clinical variables listed in Table 1 . Nonchronic major depressive disorder patients who did and did not complete at least one follow-up differed only in age and age at onset of major depressive disorder. Compared to patients without any follow-up assessments, patients with one or more follow-ups were younger (mean=29.9 years, SD=7.7, compared to mean=44.8, SD=10.8; t=3.94, df=43, p<0.001) and had an earlier age at onset of major depressive disorder (mean=23.3, SD=6.0, compared to mean=30.0, SD=7.1; t=2.10, df=42, p=0.04).
In this naturalistic study, treatment was not controlled. However, we obtained detailed information about treatment from patients and medical records. Treatment was rated by using 4-point scales measuring the adequacy of antidepressant medication and the intensity of psychotherapy (19) . Treatment ratings were collapsed into two dichotomous variables: 1) probably or definitely received adequate pharmacotherapy versus no or inadequate pharmacotherapy and 2) weekly or biweekly psychotherapy versus less frequent or no psychotherapy. Written informed consent was obtained from all study participants after a complete description of the study.
Evaluations
The baseline evaluation, conducted shortly after admission, included the Structured Clinical Interview for DSM-III-R (SCID) (20) , 24-item Hamilton Depression Rating Scale (HAM-D) (21) , and Personality Disorder Examination (22) . As reported elsewhere, the interrater reliability of the baseline diagnoses was good to excellent (12 , 16) .
Follow-up evaluations were conducted at 30, 60, 90, and 120 months after study entry. They included the Longitudinal Interval Follow-Up Evaluation (19) and 24-item HAM-D. The Longitudinal Interval Follow-Up Evaluation is a semistructured interview used to assess the course of axis I disorders and treatment. To facilitate recall and dating of episodes of psychopathology, we added a section at the beginning of the interview that included questions to elicit the occurrence and dates of major life changes and stressors during the follow-up period (1) .
Following Longitudinal Interval Follow-Up Evaluation conventions, recovery was defined as a period of at least 2 consecutive months with no more than one or two mild depressive symptoms (psychiatric status rating of <2 for major depressive disorder and 1 for dysthymic disorder). Relapse into chronic depression was defined as meeting the symptom criteria for dysthymic disorder and/or major depressive disorder (psychiatric status rating of >5 for major depressive disorder or 3 for dysthymic disorder) for at least 24 consecutive months with no more than 1 month of full remission (psychiatric status rating of <2 for major depressive disorder and 1 for dysthymic disorder) or 2 consecutive months of partial remission (psychiatric status rating of 3 or 4 for major depressive disorder and 2 for dysthymic disorder) after having met the criteria for recovery. We did not distinguish between relapse (the reemergence of the index episode) and recurrence (the development of a new episode), because there are insufficient data for this distinction in dysthymic disorder.
In the assessment of long-term diagnostic stability, a stable chronic depressive course was defined as no more than 6 consecutive months without depressive symptoms (psychiatric status rating of <2 for major depressive disorder and 1 for dysthymic disorder) for the full duration of the follow-up period. A stable nonchronic depressive course was defined as full recovery from the index depressive episode within 24 months and no subsequent period of chronic depression. In addition, we compared the groups on the proportion of patients who experienced a nonchronic major depressive disorder episode (i.e., duration of less than 24 months preceded and followed by at least 2 months of full recovery) at any point during the follow-up.
The follow-up interviews were conducted by master’s-level and doctoral-level clinicians who were unaware of the patients’ baseline diagnostic and clinical data. To assess interrater reliability, the two main study raters conducted separate Longitudinal Interval Follow-Up Evaluation and HAM-D interviews (N=32 and N=13, respectively). Kappa for recovery from dysthymic disorder was 0.66; the intraclass correlation for the HAM-D was 0.96.
Data Analysis
Chi-square tests and Fisher’s exact tests were used for between-group comparisons of categorical baseline demographic and clinical variables and onset of bipolar disorder during follow-up, and t tests were used for comparison of continuous variables. Recovery and relapse into chronic depression were examined by using the life table method and Kaplan-Meier estimation (23) . Comparisons of diagnostic stability were made with odds ratios and Fisher’s exact tests. Analysis of variance and Tukey’s honestly significant difference procedure were used to compare groups on the proportion of patients who met the criteria for mood disorder at follow-up. All tests were two-tailed.
HAM-D scores were examined by using mixed-effects growth curve models (23) . Diagnostic group was a fixed effect, and time (in months) was a random effect. Time was coded so that the intercepts of patients’ growth curves reflected their estimated scores at 10-year follow-up. There was a significant quadratic effect for time, reflecting a greater decrease in depression between the baseline and 30-month follow-up than between subsequent assessments. This pattern reflected the fact that the baseline evaluation was conducted when patients entered treatment and presumably were at a peak level of depression, whereas the timing of subsequent assessments was independent of patients’ treatment and clinical status. As the models failed to converge when both the linear and quadratic trends were treated as random variables, the quadratic parameter was fixed.
Although we used a naturalistic study design, we conducted survival and mixed-effects analyses to examine the association between treatment and subsequent course. The first set of analyses examined the associations between intensity of antidepressant pharmacotherapy and psychotherapy and recovery from dysthymic disorder in patients with dysthymic disorder. Monthly treatment scores were entered as time-varying covariates in separate Cox proportional hazards models for pharmacotherapy and psychotherapy. The analyses were lagged, so that treatment scores reflected the month before recovery or censoring. Neither pharmacotherapy (hazard ratio=1.04, 95% confidence interval [CI]=0.58–1.86, p=0.90) nor psychotherapy (hazard ratio=1.18, 95% CI=0.68–2.07, p=0.56) significantly predicted recovery from dysthymic disorder.
The second set of analyses examined the associations between treatment and HAM-D scores over time. The mean level of intensity of pharmacotherapy or psychotherapy in the 3 months before each assessment were random level-1 (within-person) variables, and diagnostic group (dysthymic disorder versus nonchronic major depressive disorder) was a fixed level-2 (between-persons) variable. Collapsed across groups, more pharmacotherapy in the 3 months before each follow-up assessment predicted significantly greater depressive symptoms (coefficient=0.892, SE=0.353; t=2.53, df=118, p=0.01). Although this result could mean that pharmacotherapy had an adverse effect on course, it is more likely that patients with poorer prognoses received more pharmacotherapy. The association between pharmacotherapy and subsequent depressive symptoms did not differ between groups (coefficient=–0.109, SE=0.888; t=–0.12, df=118, p=0.90). Psychotherapy in the 3 months before each follow-up assessment did not predict depressive symptoms (coefficient=0.209, SE=0.310; t=0.67, df=118, p=0.50), and the association between psychotherapy and subsequent depression did not differ between groups (coefficient=–0.960, SE=0.652; t=–1.47, df=118, p=0.14). In light of the limited associations between treatment and course, treatment was not included as a covariate in the analyses reported below.
Results
Fifty-one (58.6%) of the 87 patients with dysthymic disorder who had at least one follow-up assessment entered the study with a superimposed major depressive disorder episode, and 68 (78.2%) had a lifetime history of major depressive disorder. Their mean age at onset of dysthymic disorder was 10.5 years (SD=4.9). Patients with dysthymic disorder and nonchronic major depressive disorder did not differ in age, sex, race, marital status, socioeconomic status (24) , or age at onset of major depressive disorder. However, patients with dysthymic disorder had fewer years of education and higher rates of concurrent anxiety and personality disorders ( Table 1 ).
Manic/Hypomanic and Major Depressive Episodes
Five (5.7%) of the 87 patients in the dysthymic disorder group and two (5.0%) of the 40 patients in the nonchronic major depressive disorder group developed manic or hypomanic episodes during follow-up (p=1.00, Fisher’s exact test). These patients’ diagnoses were changed to bipolar disorder, and they were excluded from all further analyses.
During the course of the follow-up, 69 (84.1%) of the remaining 82 patients with dysthymic disorder and 27 (71.1%) of the remaining 38 patients with nonchronic major depressive disorder experienced a major depressive disorder episode (p=0.14, Fisher’s exact test). Of the 19 dysthymic disorder patients who entered the study with no lifetime history of major depressive disorder, 15 (78.9%) developed a first episode during follow-up (Kaplan-Meier estimated 10-year risk=82.6%). Overall, by the end of follow-up, 95.1% (78 of 82) of the patients with dysthymic disorder had a lifetime major depressive disorder episode.
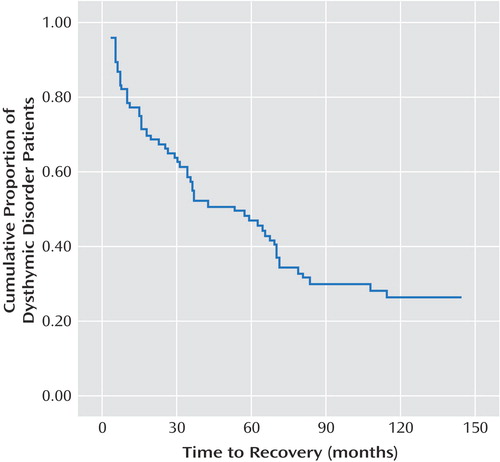
Recovery From Dysthymic Disorder
Fifty-seven (69.5%) of the 82 patients with dysthymic disorder recovered during the course of the follow-up. With adjustment for censored observations, the estimated recovery rate for dysthymic disorder was 73.9%. The mean interval between entry into the study and recovery was 64 months (95% CI=51–76; median=52). The survival function ( Figure 1 ) showed that the rate of recovery was greatest during the first 3 years of follow-up, and the slope appeared to approach the 0.20 line asymptotically after the sixth year. The estimated recovery rates of dysthymic disorder patients who entered the study with and without a superimposed major depressive disorder episode did not differ (70.2% and 78.1%, respectively; log-rank test=0.59, df=1, p=0.44).
The scoring conventions for the Longitudinal Interval Follow-Up Evaluation require that patients have no more than one or two mild symptoms for two consecutive months to be classified as recovered. However, this period may be too brief, as DSM-IV allows patients to have 2-month remissions within a dysthymic disorder episode. Therefore, we examined the effects of extending the duration criteria for recovery from dysthymic disorder to 6 months and 12 months to eliminate patients with transient remissions. With cutoff points of 6 months and 12 months, the Kaplan-Meier estimated recovery rates were 66.8% and 59.2%, respectively.
Relapse Into Chronic Depression
We examined relapse into chronic depression in the 57 dysthymic disorder patients who had recovered according to the Longitudinal Interval Follow-Up Evaluation criteria. Four patients who were followed for less than 24 months after recovery were excluded, because, by definition, they could not meet the criteria for relapse. The median interval between recovery from dysthymic disorder and the last month of follow-up was 98 months. Twenty-nine (54.7%) of the 53 patients had a relapse. With adjustment for censored observations, the estimated relapse rate was 71.4%. The mean interval between recovery and relapse was 68 months (95% CI=54–81, median=65). The survival function ( Figure 2 ) showed that the risk of relapse was greatest during the first 3 years after recovery and that it decreased substantially after 6 years. The estimated relapse rate for the 28 dysthymic disorder patients who entered the study with a superimposed major depressive disorder episode (53.6%) was lower than for the 25 dysthymic disorder patients without a superimposed major depressive disorder episode (80.0%), but this difference did not reach significance (log-rank test=0.08, df=1, p=0.78).

The nature of the chronic depressive relapses varied. Focusing on the first 24 months of the relapse and considering only the first relapse if several relapses occurred, eight (27.6%) of the 29 patients with a relapse met the full criteria for dysthymic disorder (at least 2 consecutive years of dysthymic disorder without a major depressive disorder episode), seven (24.1%) met the criteria for a chronic major depressive disorder episode (at least 2 consecutive years of meeting the full major depressive disorder criteria), and 14 (48.3%) had periods of chronic depression that did not meet the full criteria for either dysthymic disorder or chronic major depressive disorder. In these cases, the relapse either 1) began with the patient’s meeting the symptom criteria for dysthymic disorder and then developing a superimposed major depressive disorder episode within the first 2 years or 2) began with the patient’s experiencing a major depressive disorder episode that partially remitted within 2 years, leaving residual symptoms that met the symptom criteria for dysthymic disorder.
Investigators rarely have the luxury of a lengthy follow-up period before declaring a relapse. Hence, it would be useful to know if it is necessary to wait 2 years to determine if a patient meets the full duration criteria for chronic depression. We calculated the number of false positives if relapse was defined as 12 consecutive months of meeting the symptom criteria for dysthymic disorder or major depressive disorder. Only patients who were followed for at least 24 months after recovery from dysthymic disorder were considered. As noted earlier, 29 patients experienced relapses lasting at least 24 months. In addition, there were five patients whose symptoms did not persist long enough to meet the full criteria for relapse but who had met the symptom criteria for dysthymic disorder or major depressive disorder for at least 12 consecutive months after recovering from dysthymic disorder. Thus, of 34 patients with a reemergence that met the dysthymic disorder or major depressive disorder symptom criteria for at least 12 consecutive months, 29 (85.3%) ultimately met the full criteria for a chronic depressive relapse.
Comparison of Course of Depression
Next, we compared the course of depression in patients with dysthymic disorder and nonchronic major depressive disorder. First, we examined HAM-D scores at the baseline and follow-up assessments using mixed models ( Table 2 and Figure 3 ). For these analyses, we divided the dysthymic disorder group by whether or not they entered the study while experiencing a superimposed major depressive disorder episode. The patients with dysthymic disorder alone and those with double depression exhibited significantly lower rates of improvement, compared with the patients with nonchronic major depressive disorder, with regard to both linear and quadratic slope parameters (linear: coefficient=0.248, SE=0.053 [t=4.71, df=117, p<0.001] and coefficient=0.171, SE=0.053 [t=3.25, df=117, p=0.002], respectively; quadratic: coefficient=–0.0031, SE=0.0004 [t=–7.01, df=591, p<0.001] and coefficient=–0.0018, SE=0.0005 [t=–4.09, df=591, p<0.001], respectively). Patients with dysthymic disorder alone and patients with double depression also had significantly higher estimated HAM-D scores at the 10-year point (intercept) than patients with nonchronic major depressive disorder (coefficient=5.70, SE=2.03 [t=2.80, df=117, p=0.006] and coefficient=9.83, SE=2.18 [t=4.52, df=117, p<0.001], respectively).

The two groups of patients with dysthymic disorder did not differ on the linear slope parameter (coefficient=–0.076, SE=0.057; t=–1.33, df=117, p=0.18). However, they differed significantly on the quadratic slope parameter (coefficient=0.0013, SE=0.0005; t=2.55, df=591, p=0.01), as patients with double depression exhibited a sharper decline in HAM-D scores between the baseline and 30-month follow-up assessments. Finally, the patients with double depression at baseline had higher estimated HAM-D scores at the 10-year point, compared to the patients with dysthymic disorder alone, but this difference did not reach statistical significance (coefficient=4.13, SE=2.25; t=1.84, df=117, p=0.07).
Second, we used the longitudinal ratings on the Longitudinal Interval Follow-Up Evaluation to calculate the proportion of the follow-up period during which each patient met the symptom criteria for major depressive disorder or dysthymic disorder and the proportion of the follow-up during which they were completely recovered from all depressive disorders ( Table 3 ). Both subgroups of dysthymic disorder patients spent a significantly greater proportion of the follow-up period meeting the criteria for a depressive disorder and a significantly smaller proportion of the follow-up completely recovered from all depressive disorders than patients with nonchronic major depressive disorder. However, the two subgroups of dysthymic disorder patients did not differ.
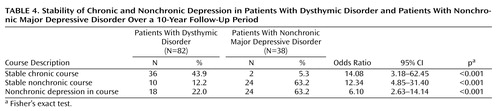
Diagnostic Stability of Chronic and Nonchronic Depression
Finally, we examined the long-term diagnostic stability of chronic and nonchronic depression ( Table 4 ). The odds of exhibiting a chronic depressive course were 14 times greater for patients with dysthymic disorder than for patients with nonchronic major depressive disorder (p<0.001), and the odds of having a nonchronic depressive course were 12 times greater for patients with nonchronic major depressive disorder than for patients with dysthymic disorder (p<0.001). Finally, although 22% of the patients with dysthymic disorder experienced a nonchronic major depressive disorder episode at some point during the follow-up, the odds of having a nonchronic episode during the follow-up were six times greater for patients with nonchronic major depressive disorder (p<0.001).
Discussion
This article reports the major findings from what we believe is the first prospective, long-term follow-up study of adults with dysthymic disorder and double depression. Long-term follow-up studies are critical for mapping the course of chronic disorders, as lengthy observation periods are necessary to observe a sufficient number of recoveries and relapses, and are especially important for dysthymic disorder because chronicity is one of its defining characteristics and a key feature in distinguishing it from major depressive disorder.
Consistent with the definition of dysthymic disorder as a chronic disorder, the course of the index dysthymic disorder episode was protracted, with a median time to recovery of 52 months from study entry. However, over the long term, the probability of recovery was relatively high, with an estimated recovery rate of 74%. This rate is about 50% higher than the estimated recovery rate in the first 5 years of follow-up (12) , supporting the value of extending the observation period. Most recoveries occurred within the first 3 years of follow-up; after 6 years, the probability of recovering was low.
Apart from our earlier report (12) , we are unaware of any data on the risk of chronic depressive relapse after recovery in dysthymic disorder. We found that the estimated relapse rate was 71%, indicating that most patients who recover from dysthymic disorder go on to have further episodes of chronic depression. Most relapses occurred within the first 3 years after recovery, with the risk of relapse dropping substantially after 6 years. These data may be helpful in informing decisions regarding the duration of maintenance treatment. Although many patients had lengthy intervals between recovery and relapse (median=65 months), they were not necessarily symptom-free; many experienced major depressive disorder episodes or subthreshold depressive symptoms that resolved in less than 2 years. Again, the additional 5 years of observation was informative, as the estimated relapse rate was approximately 50% higher than in our earlier report (12) .
Our criteria for recovery and relapse were based on convention, rather than data. A 2-month period of minimal or no symptoms may be too brief to define recovery from a chronic disorder, particularly because the DSM-IV criteria for dysthymic disorder allow up to 2 months of remission. Therefore, we examined the effects of extending the definition of recovery to 6 months and 12 months. With these more stringent definitions, the rates of recovery decreased, but even when 12 months of remission were required, the majority of patients with dysthymic disorder (59%) recovered.
By the same token, requiring 2 years at full symptom criteria may be too restrictive a definition of relapse into chronic depression. Therefore, we explored the effects of reducing the duration criteria to 12 months. Although some patients experienced a reemergence of symptoms for 12 months and then recovered before meeting the 24-month criterion, 85% of the patients meeting these less restrictive criteria went on to meet the full duration criteria.
The nature of patients’ chronic depressive relapses varied over time. Among patients with dysthymic disorder who recovered and relapsed, the relapses were just as likely to meet the criteria for chronic major depressive disorder as for dysthymic disorder, and the largest proportion were a mixture of dysthymic disorder and chronic major depressive disorder features that did not meet the criteria for either disorder. These data are consistent with our findings that dysthymic disorder patients who entered the study while in a superimposed major depressive disorder episode (double depression) and those with dysthymic disorder alone exhibited similar courses. Moreover, both sets of results are consistent with recent findings of few differences in clinical features, family history, and treatment response between patients with dysthymic disorder, double depression, and chronic major depressive disorder (13 – 15) . Taken together, these data call into question the validity of the distinctions between the various forms of chronic depression in DSM-V and suggest that chronic depression is better conceptualized as a single condition with varying levels of symptom severity over time.
Although the manifestations of chronic depression changed over time, the distinction between chronic and nonchronic depression was relatively stable. The odds of patients with dysthymic disorder exhibiting a stable chronic depressive course were 14 times greater than for patients with nonchronic major depressive disorder. Conversely, the odds of patients with nonchronic major depressive disorder experiencing a stable nonchronic depressive course were more than 12 times greater than for patients with dysthymic disorder. Together with previous findings of differences between chronic and nonchronic depressive patients in family history of psychopathology, early adversity, comorbidity, and cognitive style (2 , 8 , 13 , 25–27) , our findings indicate that the chronic-nonchronic distinction is an important source of heterogeneity in depression that should be taken into account in clinical and etiological research.
This distinction was also supported by the dysthymic disorder and nonchronic major depressive disorder patients’ trajectories of depressive symptoms over time. Compared to patients with nonchronic major depressive disorder, patients with dysthymic disorder exhibited a slower rate of improvement over time and a higher level of symptoms at the 10-year assessment. Overall, the patients with dysthymic disorder spent approximately 60% of the follow-up period meeting the symptom criteria for a depressive disorder, compared to 21% for the patients with nonchronic major depressive disorder. Together, these results suggest that although dysthymic disorder is generally conceptualized as a milder disorder than nonchronic major depressive disorder, it is often a more severe condition when considered from a longitudinal perspective.
This study had a number of strengths, including a prospective, longitudinal design with five assessments over the course of 10 years, use of semistructured interviews conducted by interviewers who were unaware of patients’ baseline diagnoses, and a “near-neighbor” comparison group of patients with nonchronic major depressive disorder. However, the study also had several limitations. First, the size of the study group was moderate. Second, patients reported on lengthy follow-up intervals. Although long follow-up periods are appropriate for chronic conditions, the dating of recovery and relapse should be regarded as approximations. Third, the study group was limited to outpatients, and we examined only the early-onset subtype of dysthymic disorder; hence these results may not apply to inpatient or community groups and to late-onset dysthymic disorder. Fourth, the majority of dysthymic disorder patients had a current or past history of major depressive disorder; hence the study group did not consist of patients with “pure” dysthymic disorder. However, data from this and other studies (4 , 8 , 12 , 13 , 16–18) have indicated that rather than being considered a distinct syndrome, superimposed major depressive disorder episodes are part of the natural history of dysthymic disorder. Fifth, although the dysthymic disorder and nonchronic major depressive disorder patients had a similar age at onset of major depressive disorder, in the former group the onset of major depressive disorder was preceded by dysthymic disorder. Thus, we cannot disentangle the effects of a dysthymic disorder diagnosis from the age at first depressive symptoms. Finally, we used a naturalistic design, and hence it is difficult to evaluate how treatment influenced patients’ course.
1. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen H-U, Kendler KS: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry 1994; 51:8–19Google Scholar
2. Markowitz JC, Moran ME, Kocsis JH, Frances AJ: Prevalence and comorbidity of dysthymic disorder among psychiatric outpatients. J Affect Disord 1992; 24:63–71Google Scholar
3. Keller MB, Klein DN, Hirschfeld RMA, Kocsis JH, McCullough JP, Miller I, First MB, Holzer CP III, Keitner GI, Marin DB, Shea T: Results of the DSM-IV mood disorders field trial. Am J Psychiatry 1995; 152:843–849Google Scholar
4. Kovacs M, Akiskal HS, Gatsonis C, Parrone PL: Childhood-onset dysthymic disorder: clinical features and prospective naturalistic outcome. Arch Gen Psychiatry 1994; 51:365–374Google Scholar
5. Barrett JE: Naturalistic change after two years in neurotic depressive disorders. Compr Psychiatry 1984; 25:404–418Google Scholar
6. Gonzales LR, Lewinsohn PM, Clarke GN: Longitudinal follow-up of unipolar depressives. J Consult Clin Psychol 1985; 53:461–469Google Scholar
7. Keller MB, Lavori PW, Endicott J, Coryell W, Klerman GL: “Double depression”: two-year follow-up. Am J Psychiatry 1983; 140:689–694Google Scholar
8. Klein DN, Taylor EB, Dickstein S, Harding K: Primary early-onset dysthymia: comparison with primary nonbipolar nonchronic major depression on demographic, clinical, familial, personality, and socioenvironmental characteristics and short-term outcome. J Abnorm Psychol 1988; 97:387–398Google Scholar
9. McCullough JP, Kasnetz MD, Braith JD, Carr KF, Cones JH, Fielo J, Martelli MF: A longitudinal study of an untreated sample of predominantly late onset characterological dysthymia. J Nerv Ment Dis 1988; 176:658–667Google Scholar
10. McCullough JP, McCune KJ, Kaye AL, Braith JA, Friend R, Roberts WC, Belyea-Caldwell S, Norris SW, Hampton C: One-year prospective replication study of an untreated sample of community dysthymia subjects. J Nerv Ment Dis 1994; 182:396–401Google Scholar
11. Ubelacker LA, Keitner GI, Ryan CE, Miller IW: Characterizing the long-term course of individuals with major depressive disorder. J Nerv Ment Dis 2004; 192:65–68Google Scholar
12. Klein DN, Schwartz JE, Rose S, Leader JB: Five-year course and outcome of dysthymic disorder: a prospective, naturalistic follow-up study. Am J Psychiatry 2000; 157:931–939Google Scholar
13. Klein DN, Shankman SA, Lewinsohn PM, Rohde P, Seeley JR: Family study of chronic depression in a community sample of young adults. Am J Psychiatry 2004; 161:646–653Google Scholar
14. McCullough JP, Klein DN, Keller MB, Holzer CE, Davis SM, Kornstein SG, Howland RH, Thase ME, Harrison WM: Comparison of DSM-III-R chronic major depression and major depression superimposed on dysthymia (double depression): a study of the validity and value of differential diagnosis. J Abnorm Psychol 2000; 109:419–427Google Scholar
15. McCullough JP, Klein DN, Borian FE, Munsaka MS, Howland RH, Riso LP, Keller MB: Group comparisons of DSM-IV subtypes of chronic depression: validity of the distinctions, part 2. J Abnorm Psychol 2003; 112:614–622Google Scholar
16. Klein DN, Riso LP, Donaldson SK, Schwartz JE, Anderson RL, Ouimette PC, Lizardi H, J Aronson TA: Family study of early-onset dysthymia: mood and personality disorders in relatives of outpatients with dysthymia and episodic major depression and normal controls. Arch Gen Psychiatry 1995; 52:487–496Google Scholar
17. Akiskal HS: Dysthymic disorder: psychopathology of proposed chronic depressive subtypes. Am J Psychiatry 1983; 140:11–20Google Scholar
18. Kocsis JH, Frances AJ: A critical discussion of DSM-III dysthymic disorder. Am J Psychiatry 1987; 144:1534–1542Google Scholar
19. Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC: The Longitudinal Interval Follow-Up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry 1987; 44:540–548Google Scholar
20. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R, Version 1.0 (SCID). Washington, DC, American Psychiatric Press, 1990Google Scholar
21. Miller IW, Bishop S, Norman WH, Maddever H: The modified Hamilton Rating Scale for Depression: reliability and validity. Psychiatry Res 1985; 14:131–142Google Scholar
22. Loranger AW, Susman VL, Oldham JM, Russakoff M: The Personality Disorder Examination (PDE) Manual. Yonkers, NY, DV Communications, 1988Google Scholar
23. Singer JD, Willett JB: Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford, UK, Oxford University Press, 2003Google Scholar
24. Hollingshead AB: Four-Factor Index of Social Status. New Haven, Conn, Yale University, Department of Sociology, 1975Google Scholar
25. Garyfallos G, Adamopoulou A, Karastergiou A, Voikli M, Sotiropoulou A, Donias S, Giouzepas J, Paraschos A: Personality disorders in dysthymia and major depression. Acta Psychiatr Scand 1999; 99:332–340Google Scholar
26. Lizardi H, Klein DN, Ouimette PC, Riso LP, Anderson RL, Donaldson SK: Reports of the childhood home environment in early-onset dysthymia and episodic major depression. J Abnorm Psychol 1995; 104:132–139Google Scholar
27. Riso LP, du Toit PL, Blandino JA, Penna S, Darcy S, Duin JS, Pacoe EM, Grant MM, Ulmer CS: Cognitive aspects of chronic depression. J Abnorm Psychol 2003; 112:72–80Google Scholar