Neuroticism and Affective Instability: The Same or Different?
Abstract
Objective: The purpose of this study was to examine the correlates and consequences of two constructs related to affective experience: neuroticism and affective instability. Method: One hundred thirty-two patients were assessed at intake for axis I and II symptoms, general personality traits, and specific impairments, including impairments in interpersonal functioning. The data included responses to structured and semistructured interviews, self-reports of interpersonal problems, and reports of interpersonal problems from significant others. Clinical ratings of axis I and II symptoms and of impairment were made by using the LEAD (i.e., longitudinal, expert, all data) consensus approach. Ninety-one of the 132 patients were reassessed at 12-month follow-up. Results: Neuroticism and affective instability manifested varied concurrent relations, with neuroticism being strongly related to an anxious, avoidant style and affective instability related to more externalizing personality styles. Prospectively, neuroticism predicted later symptoms, occupational impairment, and global dysfunction, whereas affective instability predicted romantic impairment. Conclusions: The findings suggest that neuroticism and affective instability—which are considered core aspects of personality pathology—are related but distinct constructs with unique correlates and different predictive abilities.
Neuroticism, which is a core dimension of many personality models, is defined as a predisposition toward negative affective states such as depression, anxiety, anger, and shame. Numerous studies have documented its central role in both axis I (1 – 3) and axis II disorders (4 – 6) . Neuroticism is negatively related both concurrently and prospectively to impairment in a number of life domains, including those related to physical health (7 – 9) , romance (10 – 11) , and occupational success/satisfaction (12) .
Neuroticism, although clearly a valid and useful construct, does not provide a complete picture of the manner in which mood or affect may be problematic. Westen and colleagues (13) described a number of affective-related constructs such as “affect intensity, lability, tendency to experience pleasant and unpleasant emotions, tendency to experience particular affects, consciousness of affective experience, capacity for experiencing ambivalent emotions, and emotional expression,” many of which are not assessed by most neuroticism scales. Affective lability or instability is one construct that has received little attention as a unitary construct, because it is typically examined within the context of the broader disorders in which it is embedded (e.g., borderline personality disorder, bipolar I disorder, bipolar II disorder). This lack of attention is unfortunate, as these disorders are characterized by significant impairments in life functioning. For example, numerous studies have documented the relations between borderline personality disorder and broad dysfunction. Trull and colleagues (14 , 15) demonstrated that borderline personality disorder is related to academic difficulties and interpersonal problems 2 years later, even when adjustment was made for axis I and II psychopathology. Using multiple rating sources, Skodol et al. (16) found that borderline personality disorder symptoms were related to both self-rated impairment and expert-rated impairment.
Unfortunately, until recently, it has been difficult to discern which characteristics of borderline personality disorder are particularly relevant to these various forms of impairment and dysfunction. A number of studies have examined the factor structure of borderline personality disorder (17 – 20) , and, although debate continues, there is a growing consensus that “affective instability” is a core component of the disorder. In a study in which item response theory analyses were used to examine the utility of DSM-IV borderline personality disorder symptoms, it was found that “affective instability” was the most informative criterion (unpublished 2005 manuscript of Feske et al.). Affective instability may also manifest varied relations with impairment across life domains. For example, Bagge et al. (14) found that affective instability was among the most important predictors of academic/occupational impairment and social maladjustment over a 2-year period and was a significant predictor of academic impairment, even when adjustment was made for Five-Factor Model neuroticism. These findings have spurred a growing interest in developing a better understanding of affective instability, particularly with reference to borderline personality disorder. In this vein, two studies have documented a particular tendency among individuals with borderline personality disorder to fluctuate between normal mood and states of increased anger and anxiety (21 , 22) , and another study found that these fluctuations tend to be random in nature (23) .
Finally, it may be that both affective instability and a tendency to experience negative emotions (e.g., neuroticism) are key components of borderline personality disorder and the resultant impairments. Studies by Westen and colleagues (13 , 24) have supported this interpretation. Their analyses have suggested that affective instability and intense negative affect are two of the most prototypical items that describe borderline personality disorder in adolescent and adult patients. Finally, these symptoms appear to be among the most stable of the borderline personality disorder symptoms over time.
Affectively based borderline personality disorder symptoms such as instability, chronic depression, guilt, anger, and anxiety are among the least likely to have remitted at 6-year follow-up (25) . Similarly, Skodol et al. (16) cited unpublished data of Shea et al. showing that 90% of patients with borderline personality disorder assessed throughout a 1-year period had persistent intense anger and affective instability.
The goal of the current study was to examine the concurrent and predictive relations between neuroticism and affective instability and to examine their unique effects. In particular, we were interested in placing these constructs in broader nomological networks by examining their concurrent relations with general personality traits, personality disorder symptoms, and impairment in interpersonal functioning. We also examined the 1-year predictive powers of neuroticism and affective instability in relation to depression and anxiety symptoms and indices of romantic, social, occupational, and general impairment. Finally, because of the potential for sex differences in these constructs (26 , 27) , we also examined differences in mean levels across sex and whether the constructs operated in a different manner according to sex.
Method
Participants and Procedures
Participants were recruited from inpatient and outpatient programs at Western Psychiatric Institute and Clinic in Pittsburgh. Patients with psychotic disorders, organic mental disorders, and mental retardation were excluded, as were patients with major medical illnesses that influence the CNS and might be associated with organic personality disturbance (exclusions were based on information available from each patient’s previous treatment records). Participants provided written informed consent after all study procedures had been explained. Of the original group of 152 participants, 132 completed the NEO Personality Inventory (28) . Of these 132 participants, 91 (69%) were also assessed at a 12-month follow up. The NEO Personality Inventory and DSM-III-R personality disorder criteria were used in this study because the newer versions of these measures were not yet available at the time these data were collected.
The study group included 76 women (58%) and 56 men (42%); 115 (87%) participants were Caucasian, 16 (12%) were African American, and one (1%) was Asian American. The average age of the participants (N=132) was 34.9 years (SD=9.4, range=20–59). At the time of the assessment, 104 participants (79%) were outpatients and 28 (21%) were inpatients. Axis I ratings were determined by expert consensus at case conference and were based on the results of a structured clinical interview. Table 1 summarizes the participants’ axis I and axis II diagnoses.
We conducted analyses to examine whether there were statistically significant differences between participants with versus without complete data at follow-up. The following 16 variables were compared in these analyses: age, sex, race, treatment condition (inpatient versus outpatient), marital status, education, and symptom counts for the 10 DSM-III-R personality disorders that remain in DSM-IV. We found significant differences for only two of these variables. Compared to those who were present at follow-up, those present only for the time-1 assessment were significantly more likely to have received inpatient treatment (c2=5.40, df=1, p<0.05) and had higher symptom counts for narcissistic personality disorder (t=2.10, df=130, p<0.05).
Measures
Affective instability
The affective instability score used here was rationally constructed by reviewing DSM-III-R personality disorder criteria and identifying items that explicitly reference a predisposition toward affective lability or instability. The four items used in this scale were 1) is easily slighted and is quick to react with anger or to counterattack (paranoid personality disorder), 2) displays rapidly shifting and shallow expression of emotions (histrionic personality disorder), 3) affective instability (borderline personality disorder), and 4) inappropriate, intense anger, or lack of control of anger (borderline personality disorder). The four-item affective instability scale demonstrated acceptable internal consistency (alpha of 0.68, which was close to the median alpha [0.69] of the full criteria for the DSM personality disorders in this study group). The mean for this scale was 1.91 (SD=2.11), and scores ranged from 0 to 8. Given the nature of the items used to construct this scale, the current affective instability construct appears to measure both affective instability and intensity in that the noted affective shifts are to extreme or maladaptive levels.
Neuroticism
Neuroticism was measured with the 48-item self-report scale from the NEO Personality Inventory. The mean was 3.32 (SD=0.48), and scores ranged from 2.15 to 4.33.
The NEO Personality Inventory (28) is an earlier version of the NEO Personality Inventory–Revised, a measure of the Five Factor Model of personality, which includes subscales only for the domains of neuroticism, extraversion, and openness. The NEO Personality Inventory includes 180 items rated on a 5-point scale; 48 items constitute each of the domains of neuroticism, extraversion, and openness, and 18 items are used to assess agreeableness and conscientiousness, respectively. The internal consistency reliabilities for the five domains ranged from 0.82 (agreeableness) to 0.91 (neuroticism), with a mean of 0.87.
Consensus ratings of DSM-III-R personality disorder criteria and impairment
Complete details of the assessment methods are provided in previous reports (29 , 30) . A brief summary is included here. At intake, participants were interviewed for 6–10 hours in a minimum of three assessment sessions. The assessments sessions included structured symptom ratings, structured interviews for axis I and axis II disorders (e.g., the Structured Clinical Interview for DSM-III-R, the Personality Disorder Examination [31] , or Structured Clinical Interview for DSM-III-R Personality Disorders [32] ), and a detailed social and developmental history. The patients also completed self-report questionnaires between interviews. After the evaluation, the primary interviewer presented the case at a 2-hour diagnostic conference with colleagues from the research team. All available data (historical and concurrent) were reviewed and discussed at the conference, including current and lifetime axis I symptoms, symptom status, social and developmental history, and personality features acknowledged on the axis II interviews. Each personality disorder symptom was rated on a scale from 0 to 2. The personality disorder symptom counts used here are simply the addition of these scores across all symptoms for each personality disorder.
Inventory of Interpersonal Problems
The Inventory of Interpersonal Problems (33) is a 127-item self- or other-report measure of difficulties in interpersonal functioning and associated distress. Responses are scored on a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). In the current study, we used intake self- and other-reported personality disorder scores (34) for the following constructs: interpersonal sensitivity, interpersonal ambivalence, aggression, need for approval, and lack of sociability.
Consensus ratings of impairment
Consensus ratings of functional impairment were made for romantic relationships, other social relationships (e.g., friends, family members), and work. These scores were made by using a 5-point scale, ranging from 1 (little or none) to 5 (severe). The ratings used here were from the 12-month follow-up.
Clinical ratings of depression, anxiety, and functioning
Ratings of psychological distress were conducted with two well-validated, commonly used instruments: the Hamilton Depression Rating Scale (HAM-D) (35) and the Hamilton Anxiety Rating Scale (HAM-A) (36) . Hamilton scores were determined by the primary interviewer for each case. The mean intake scores for the HAM-D and HAM-A were 14.8 (SD=8.0) and 15.1 (SD=8.8), respectively. At the 12-month follow-up, the mean HAM-D and HAM-A scores were 8.5 (SD=7.7) and 8.3 (SD=8.0), respectively. Functioning was assessed with the Global Assessment of Functioning (GAF) Scale, with possible scores ranging from 0 to 100. The mean GAF scores at intake and 12-month follow-up were 54.2 (SD=7.5) and 62.7 (SD=9.1), respectively.
Twelve-Month Follow-Up
All intake procedures (e.g., structured interviews for axis I and axis II disorders, symptom ratings, ratings of functioning, NEO Personality Inventory, and Inventory of Interpersonal Problems) were repeated at the 12-month follow-up, with the exception of the social/developmental history. As at intake, all sources of available data (e.g., self-reported data, other-reported data, expert assessments, and current and historical data) were used to inform the consensus ratings.
Statistical Analyses
First, Pearson’s product-moment correlation was used to examine the relations between neuroticism, affective stability, and several concurrently measured variables. We then examined whether the sets of correlations (the dependent r values) were statistically significantly different (e.g., whether the correlation for neuroticism and paranoid personality disorder was significantly different from the correlation for affective instability and paranoid personality disorder) (37) . To control for the number of analyses conducted in this first set, we lowered the p value to 0.01. Next, we used simultaneous linear regression analyses to examine the unique predictive relations between neuroticism and affective instability and six outcomes measured at 12-month follow-up and the overall variance accounted for by these variables (i.e., R 2 ). Two-tailed p values were computed in all analyses.
Results
Characterizing Neuroticism and Affective Instability: Concurrent Relations
Sex
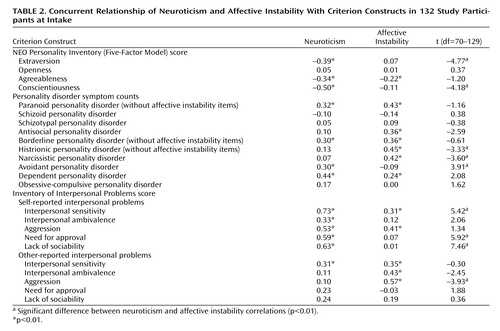
There were no significant sex differences in the measures of neuroticism (t=0.85, df=130, p=0.40) or affective instability (t=0.41, df=130, p=0.69). All bivariate correlations presented in Table 2 were also tested separately for men and women; of the 48 pairs of correlations, only one was significantly different (consistent with a chance finding). As a result, we present the combined correlations in Table 2 .
Interrelation and relations with the Five-Factor Model
Next, we examined the intercorrelation between neuroticism and affective instability. There was a small but significant correlation between the neuroticism and affective instability scales (r=0.27, p<0.01). We also examined the relations between these two constructs and the remaining four Five-Factor Model domains (measured with the NEO Personality Inventory). As Table 2 shows, neuroticism was significantly negatively correlated with extraversion, agreeableness, and conscientiousness. Alternatively, affective instability was only significantly (negatively) correlated with agreeableness. The correlations of neuroticism with extraversion and conscientiousness were significantly stronger than those of affective instability with extraversion and conscientiousness.
Relations with personality disorders
As Table 2 shows, neuroticism was significantly correlated with four of the 10 personality disorders (with the items used for the affective instability scale removed): paranoid, borderline, avoidant, and dependent. Affective instability was significantly correlated with six of the 10 personality disorders: paranoid, antisocial, borderline, histrionic, narcissistic, and dependent. The correlation between neuroticism and avoidant personality disorder was significantly larger than that between affective instability and avoidant personality disorder, whereas the correlations of affective instability with histrionic personality disorder and narcissistic personality disorder were significantly larger than those found for neuroticism.
Relations with interpersonal functioning: self-reports
As Table 2 shows, neuroticism was significantly correlated with all five self-report interpersonal problem indices from the Inventory of Interpersonal Problems: interpersonal sensitivity, interpersonal ambivalence, aggression, need for approval, and lack of sociability. Affective instability was significantly correlated with interpersonal sensitivity and aggression. The correlations between neuroticism and interpersonal sensitivity, need for approval, and lack of sociability were significantly stronger than those found for affective instability.
Relations with interpersonal functioning: reports of others
Neuroticism was significantly correlated only with other-reported interpersonal sensitivity, whereas affective instability was significantly correlated with other-reported interpersonal sensitivity, interpersonal ambivalence, and aggression. The correlation between affective instability and aggression was stronger than the correlation found between neuroticism and this scale.
Neuroticism and Affective Instability as Predictors of 12-Month Outcomes
Simultaneous regression analyses were conducted in which neuroticism and affective instability were used to predict depression, anxiety, and impairment/functioning at 12 months ( Table 3 ). Overall, neuroticism and affective instability accounted for between 6% and 21% of the total variance in the outcomes, results that were significant for five of the six outcomes. Neuroticism was a significant unique predictor of poorer outcomes in four of the six outcomes, whereas affective instability was a significant unique predictor of a poorer outcome in one of the outcomes. Neuroticism predicted depression and anxiety scores, occupational impairment, and lower overall functioning (i.e., GAF score). Affective instability predicted only romantic impairment. There were no outcomes for which both neuroticism and affective instability were significant predictors.
Discussion
Researchers have increasingly attempted to parse affective experience into its various components in order to understand the etiology and consequences of these components. The current study compared the concurrent correlates and outcomes of two affective constructs: neuroticism (the tendency to experience negative emotions such as anxiety, depression, guilt, shame, or anger) and affective instability (the tendency to experience frequently and quickly changing mood states). Neuroticism has been a mainstay in psychiatry and psychology and has served as a useful predictor of psychiatric and physical impairment, as well as other problematic behaviors. On the other hand, affective instability has been examined as part of broader clinical syndromes such as borderline personality disorder, histrionic personality disorder, and variants of bipolar disorder. Several studies have suggested that affective instability is among the most informative and predictive components of borderline personality disorder (14 , 19 , 20 , 22 ; unpublished 2005 manuscript of Feske et al.). Attempts to develop more empirically guided personality disorder diagnoses by researchers such as Clark (38) and Livesley (39) , as well as by Shedler and Westen (40) , using different methods, have converged on the notion that emotional dysregulation/affective instability and neuroticism/chronic dysphoria are core aspects of personality pathology.
The aims of this study were to place these two personality constructs in a broader context by examining their concurrent relations with general personality dimensions, pathological personality constructs, and interpersonal functioning, as well as examining their unique predictive relations with symptoms and functioning at 12-month follow-up. Examining the pattern of concurrent findings, it is evident that neuroticism and affective instability have real differences in both the direction and size of the correlates. In fact, of the 24 pairs of correlations examined, nine (38%) were significantly different (p<0.01) between the two scales. Neuroticism was uniquely associated with introversion, lower conscientiousness, avoidant personality disorder symptoms, self-reported interpersonal sensitivity, need for approval, and a lack of sociability. Conversely, affective instability was uniquely related to cluster B personality disorder symptoms, as well as other-reported levels of interpersonal ambivalence and aggression. Overall, these correlations paint two different pictures. Neuroticism seems to be primarily associated with an anxious, avoidant interpersonal style as well as a lower sense of competence, which may lead to an overdependence or reliance on others for emotional and instrumental support. Neurotic individuals tend to internalize their emotional problems and may experience their significant dysphoria in a quieter, less intrusive manner. Affective instability was associated primarily with an interpersonal style characterized by acting out in an egocentric, unpredictable manner that may lead to aggression, antisociality, or an overly dramatic behavioral style. The dysregulation of affect may lead these individuals to behave impulsively (e.g., self-harming behavior, interpersonal aggression) in order to cope with new affective states.
The current results also address issues of self- and other-perception in relation to these two traits. Individuals with higher levels of neuroticism viewed themselves as having a broad array of interpersonal problems, while reports of significant others (e.g., romantic partners, family members, friends) suggested that neurotic individuals overestimate their interpersonal impairment. This finding is consistent with the idea that these individuals maintain a global negative schema about themselves and others. In contrast, the self-perceptions of individuals with higher levels of affective instability suggested that they see their interpersonal problems as more limited, while their significant others reported that these individuals are more broadly impaired in the interpersonal domain. In contrast to neurotic individuals, who may tend to overestimate interpersonal problems, individuals with affective instability may be prone to underestimate interpersonal difficulties.
Prospectively, neuroticism and affective instability were also associated with different outcomes. Neuroticism predicted symptoms (e.g., depression, anxiety), symptom-related functioning (e.g., GAF scale score), and occupational impairment. Affective instability was solely predictive of impairment in romantic functioning. It may be that the unpredictability and tendency toward explosive anger make it difficult for persons with affective instability to maintain intimate relationships. In fact, the predictability of chronic negative affect, while potentially tiresome and distressing, may cause less interpersonal strain than interaction on a regular basis with someone whose affect is unknowable or unpredictable. For work-related functioning, neuroticism was the sole unique predictor, which is not surprising, given the wealth of literature on this relationship (12 , 41) . Neuroticism, which is a prospective predictor of axis I symptoms, may make it difficult to work because of the likelihood of experiencing significant psychiatric symptoms. In contrast, the formal social boundaries and the potential for more socially isolative or autonomous jobs may make affective instability less problematic in work settings. Affectively labile individuals may be able to modulate their affective experience or expression in work settings because the prohibitions against unchecked mood states may be quite clear or because they find work situations in which interpersonal interactions are less frequent or less likely to trigger instability, given the less intimate nature of the relationships.
Several limitations of the current study must be noted. First, common method variance may have artificially inflated certain relations such as neuroticism with other five-factor model domains (e.g., extraversion and conscientiousness) or affective instability with other personality disorders, particularly the cluster A and B personality disorders (where the affective instability items originated). However, a number of significant cross-method relations were also found. Another limitation of the current study was that the affective instability construct might have been overly weighted toward rapid fluctuations to anger, as two of the four affective instability scale items explicitly addressed the loss of one’s temper and/or intense anger. This weighting may be, in part, a limitation of the DSM personality disorder criteria, in that anger-related fluctuations are more likely to be viewed as associated with problematic personality styles than are other types of affective changes. The current method for assessment of affective instability did not allow for a finer parsing of this construct, such as is possible with the Affective Lability Scales (ALS) (42) . However, the findings of Koenigsberg et al. (22) , who reported a correlation of 0.44 between the ALS total score and the DSM-III-R affective instability symptoms, suggest that the current affective instability scale provided valid data on this construct. The shortness of the affective instability scale, and thus its reduced internal consistency, may have attenuated its correlation with criterion variables and put it at a disadvantage, compared with the longer, more reliable neuroticism scale. It is also noteworthy that the attrition from intake to follow-up (31%) may have affected the longitudinal results because those who did not complete the assessment may have been more seriously impaired (i.e., they were more likely to have been inpatients at intake).
Conclusions
Viewed both concurrently and prospectively, the tendency to experience chronic negative affective states and the tendency to fluctuate between affective states are, despite some overlap, distinct constructs with significantly different correlates and consequences. The fact that neuroticism and affective instability are differentially related to a variety of interpersonal problems and life impairments suggests that both warrant clinical attention and require purposeful attention and assessment.
1. Clark LA, Watson D, Mineka S: Temperament, personality, and the mood and anxiety disorders. J Abnorm Psychol 1994; 103:103–116Google Scholar
2. Krueger RF, McGue M, Iacono WG: The higher order structure of common DSM mental disorders: internalization, externalization, and their connections to personality. Pers Individ Dif 2001; 30:1245–1259Google Scholar
3. Watson D, Clark LA, Harkness AR: Structures of personality and their relevance to psychopathology. J Abnorm Psychol 1994; 103:18–31Google Scholar
4. Lynam DR, Widiger TA: Using the five-factor model to represent the DSM-IV personality disorders: an expert consensus approach. J Abnorm Psychol 2001; 110:401–412Google Scholar
5. Miller JD, Reynolds SK, Pilkonis PA: The validity of the five-factor model prototypes for personality disorders in two clinical samples. Psychol Assess 2004; 16:310–322Google Scholar
6. Morey LC, Gunderson JG, Quigley BD, Shea MT, Skodol AE, McGlashan TH, Stout RL, Zanarini MC: The representation of borderline, avoidant, obsessive-compulsive, and schizotypal personality disorders by the five-factor model. J Personal Disord 2002; 16:215–234Google Scholar
7. Neeleman J, Sytema S Wadsworth M: Propensity to psychiatric and somatic ill-health: evidence from a birth cohort. Psychol Med 2002; 32:793–803Google Scholar
8. Williams PG, O’Brien CD, Colder CR: The effects of neuroticism and extraversion on self-assessed health and health-relevant cognition. Pers Indiv Dif 2004; 37:83–94Google Scholar
9. Costa PT Jr, McCrae RR: Neuroticism, somatic complaints, and disease: is the bark worse than the bite? J Pers 1987; 55:299–316Google Scholar
10. Karney BR, Bradbury TN: The longitudinal course of marital quality and stability: a review of theory, method, and research. Psychol Bull 1995; 118:3–34Google Scholar
11. Kelly EL, Conley JJ: Personality and compatibility: a prospective analysis of marital stability and marital satisfaction. J Pers Soc Psychol 1987; 52:27–40Google Scholar
12. Tokar DM, Fischer AR, Subich LM: Personality and vocational behavior: a selective review of the literature, 1993–1997. Journal of Vocational Behavior 1998; 53:115–153Google Scholar
13. Westen D, Muderrisoglu S, Fowler C, Shedler J, Koren D: Affect regulation and affective experience: Individual differences, group differences, and measurement using a qsort procedure. J Consult Clin Psychol 1997; 65:429–439Google Scholar
14. Bagge C, Nickell A, Stepp S, Durrett C, Jackson K, Trull TJ: Borderline personality disorder features predict negative outcomes 2 years later. J Abnorm Psychol 2004; 113:279–288Google Scholar
15. Trull TJ, Useda D, Conforti K, Doan BT: Borderline personality disorder features in nonclinical young adults: 2. two-year outcome. J Abnorm Psychol 1997; 106:307–314Google Scholar
16. Skodol AE, Gunderson JG, McGlashan TH, Dyck IR, Stout RL, Bender DS, Grilo CM, Shea MT, Zanarini MC, Morey LC, Sanislow CA, Oldham JM: Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry 2002; 159:276–283Google Scholar
17. Clarkin JF, Hull JW, Hurt SW: Factor structure of borderline personality disorder criteria. J Personal Disord 1993; 7:137–143Google Scholar
18. Fossati A, Maffei C, Bagnato M, Donati D, Namia C, Novella L: Latent structure analysis of DSM-IV borderline personality disorder criteria. Compr Psychiatry 1999; 40:72–79Google Scholar
19. Sanislow CA, Grilo CM, McGlashan TH: Factor analysis of the DSM-III-R borderline personality disorder criteria in psychiatric inpatients. Am J Psychiatry 2000; 157:1629–1633Google Scholar
20. Sanislow CA, Grilo CM, Morey LC, Bender DS, Skodol AE, Gunderson JG, Shea MT, Stout RL, Zanarini MC, McGlashan TH: Confirmatory factor analysis of DSM-IV criteria for borderline personality disorder: findings from the Collaborative Longitudinal Personality Disorders Study. Am J Psychiatry 2002; 157:284–290Google Scholar
21. Henry C, Mitropoulou V, New AS, Koenigsberg HW, Silverman J, Siever LJ: Affective instability and impulsivity in borderline personality disorder and bipolar II disorders: similarities and differences. J Psychiatr Res 2001; 35:307–312Google Scholar
22. Koenigsberg HW, Harvey PD, Mitropoulou V, Schmeidler J, New AS, Goodman M, Silverman JM, Serby M, Schopick F, Siever LJ: Characterizing affective instability in borderline personality disorder. Am J Psychiatry 2002; 159:784–788Google Scholar
23. Cowdry RW, Gardner DL, O’Leary KM, Leibenluft E, Rubinow DR: Mood variability: a study of four groups. Am J Psychiatry 1991; 148:1505–1511Google Scholar
24. Westen D, Shedler J, Durrett C, Glass S, Martens A: Personality diagnoses in adolescence: DSM-IV axis II diagnoses and an empirically derived alternative. Am J Psychiatry 2003; 160:952–966Google Scholar
25. Zanarini MC, Frankenburg FR, Hennen J, Silk KR: The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry 2003; 160:274–283Google Scholar
26. Costa PT Jr, Terracciano A, McCrae, RR: Gender differences in personality traits across cultures: robust and surprising findings. J Pers Soc Psychol 2001; 81:322–331Google Scholar
27. Corbitt EM, Widiger TA: Sex differences among the personality disorders: an exploration of the data. Clinical Psychology: Science and Practice 1995; 2:225–238Google Scholar
28. Costa PT Jr, McCrae RR: The NEO Personality Inventory manual. Odessa, Fla, Psychological Assessment Resources, 1985Google Scholar
29. Pilkonis PA, Heape CL, Proietti JM, Clark SW, McDavid JD, Pitts TE: The reliability and validity of two structured diagnostic interviews for personality disorders. Arch Gen Psychiatry 1995; 52:1025–1033Google Scholar
30. Pilkonis PA, Heape CL, Ruddy J, Serrao PS: Validity in the diagnosis of personality disorders: the use of the LEAD standard. Psychol Assess 1991; 3:46–54Google Scholar
31. Loranger AW, Susman VL, Oldham JM, Russakoff M: The Personality Disorder Examination (PDE) Manual. Yonkers, NY, DV Communications, 1988Google Scholar
32. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). New York, New York State Psychiatric Institute, Biometrics Research, 1990Google Scholar
33. Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS: Inventory of Interpersonal Problems: psychometric properties and clinical applications. J Consult Clin Psychol 1988; 56:885–892Google Scholar
34. Pilkonis PA, Kim Y, Proietti JM, Barkham M: Scales for personality disorders developed from the Inventory of Interpersonal Problems. J Personal Disord 1996; 10:355–369Google Scholar
35. Hamilton M: A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62Google Scholar
36. Hamilton M: The assessment of anxiety states by rating. Br J Med Psychol 1959; 32:50–55Google Scholar
37. Cohen J, Cohen P: Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences, 2nd ed. Hillsdale, NJ, Lawrence Erlbaum Associates, 1983Google Scholar
38. Clark LA: Toward a consensual set of symptom clusters for assessment of personality disorder, in Advances in Personality Assessment. Edited by Butcher JN, Spielberger CD. Hillsdale, NJ, Lawrence Erlbaum Associates, 1990, pp 243–266Google Scholar
39. Livesley WJ, Jackson DN, Schroeder ML: A study of the factorial structure of personality pathology. J Personal Disord 1989; 3:292–306Google Scholar
40. Shedler J, Westen D: Dimensions of personality pathology: an alternative to the Five-Factor Model. Am J Psychiatry 2004; 161:1743–1754Google Scholar
41. Salgado JF: The Five-Factor Model of Personality and job performance in the European community. J Appl Psychol 1997; 82:30–43Google Scholar
42. Harvey PD, Greenberg BR, Serper MR: The affective lability scales: development, reliability, and validity. J Clin Psychol 1989; 45:786–793Google Scholar