The Cognitive Origins of Specific Types of Schizophrenic Speech Disturbances
Abstract
Objective: Cognitive impairments associated with schizophrenia might be expected to have a marked impact on the ability to produce coherent speech, yet associations between cognitive performance and speech disorder have typically been weak. Findings on this question may have been limited by measurement methods and by the heterogeneity of speech disorder. This study examined the contributions of impairments in sustained attention and sequencing abilities to schizophrenic speech disorder, measured in terms of communication failures and divided into different types of disorder. Method: Samples of natural speech were collected from severely ill inpatients with schizophrenia and nonpsychiatric comparison subjects and rated for frequencies of six types of communication failures: four structural and two nonstructural types. Subjects also completed a battery of cognitive tests assessing several facets of attention and sequencing ability. Hierarchical regression was used to identify cognitive contributors to communication failures. Results: Impaired sustained attention was associated with more frequent structural and nonstructural communication failures. As predicted, impaired sequencing, and in particular conceptual sequencing, also made a substantial contribution to the structural communication failures, but not to the nonstructural ones. These findings held when global level of impairment was controlled statistically. Performance on the tests of attention and sequencing explained 56% of the variance in structural speech disorder. Conclusions: Schizophrenic speech disorder is heterogeneous in form and in cognitive underpinnings. Impairments in attention and sequencing abilities are highly predictive of communication failures related to language structure.
Disordered speech is a central symptom of schizophrenia (1) and one that may persist even when other psychotic symptoms improve (2) . It is a major contributor to the chronic social disability often associated with the illness (3 , 4) . If the pathological processes underlying speech disorder could be identified clearly, they could be targeted specifically in the development of both cognitive remediation programs and cognition-focused pharmacotherapeutic agents. Although much effort has gone into identifying the processes underlying schizophrenic speech disorder, its causes are still not well understood (see reference 5 for a review).
Schizophrenia involves marked deficits in attention (6) and ordering, or sequencing, ability (7 , 8) . These deficits may be part of what causes speech disorder. A speaker with poor attentional capacity might lose coherence either by being too easily distracted by competing thoughts and associations or by forgetting the original discourse plan before its completion; a speaker with impaired sequencing ability might be unable to order words and phrases adequately for the communication of intended meanings (1 , 8) . If impairments in these functions do underlie schizophrenic speech disorder, there should be specific associations between performance on tests of attention and sequencing and measures of severity of speech disorder. In general, attempts to identify such associations have had limited success. When significant associations have been identified at all, they have usually been modest, especially after generalized deficit effects have been factored out (5) .
In this study, we took into consideration two possible reasons for the weakness of previous findings in this area: the ways in which speech disorder has been measured and the probable heterogeneity of speech disorder. Most research on schizophrenic speech disorder has used measures designed to target the formal thought disorder that presumably underlies the speech disorder (1 , 9) . A small number of studies have measured speech disorder in terms of characteristics of language structure, such as agrammaticality or inadequacies of structure and complexity (10 , 11) . Although formal thought disorder and faulty language structure make speech more difficult to follow, neither of these approaches to the measurement of speech disorder focuses on loss in clarity of meaning per se. Rather, the focus of measurement is on whatever is presumed to underlie the disorder in the speech—either thought disorder or an inability to structure language. A third approach that differs from these two assesses speech disorder strictly in terms of impairment in the communication of meaning (12 , 13) . This is a pragmatic approach based on the idea that the primary purpose of speech is to communicate meaning and that therefore the most direct way to measure deficiencies of speech, or speech disorder, is in terms of failures in the transmission of meaning from speaker to listener. This communication approach has some conceptual advantages over the other perspectives (14) . Furthermore, studies that have used more communication-oriented measures of speech disorder have tended to find stronger associations with cognitive test performance than those using measures of formal thought disorder or linguistic dysfunction (5 , 14) . Perhaps the most notable exception to the generally weak associations between cognitive test performance and speech disorder (after controlling for generalized deficit effects) was reported by Harvey and colleagues (15) , who identified a strong association between auditory distractibility and the frequency of incompetent references in speech. Their study was unusual in two ways: it used a purely communication-oriented measure of speech, and it found a strong effect.
The second probable reason for the often disparate and weak findings is that schizophrenic speech disorder is not a unitary symptom (3 , 16) . It is heterogeneous in form and probably also in cognitive origins, whether defined as thought, linguistic, or communication disturbance. When speech disorder is assessed in terms of communication failures, as in the present study, there are a number of different ways in which meanings in speech may be unclear. For example, words or phrases may be unclear because they lack specificity; or they may have more than one definitional meaning and be presented without any discriminating context; or a reference may be presented in the absence of its referent; or meaning may be lost as a result of grammatical breakdown (13) . Cognitive impairment also is heterogeneous in schizophrenia, with differences among patients in types and combinations of deficiencies. Different types of communication failures could well reflect different underlying cognitive impairments (8 , 16) . If this is the case, then attempts to identify cognitive correlates of speech disorder lose power when they look at speech disorder globally. With respect to communication failures, some instances are structural, based on interclausal relationships between different words or phrases in the speech, whereas others are nonstructural, related only to incorrect or unclear individual words or phrases (13) . The structural types of communication failure appear to be reflective of poor sequencing abilities, whereas the nonstructural types do not.
In this study, we were interested in identifying cognitive contributors to communication failures in the realms of attention and sequencing ability. In preliminary findings on a small sample of stable outpatients with schizophrenia, we found indications of sizable correlations between attention and sequencing impairments and structural communication disturbances (8) . In this study, we looked at a sample of severely ill inpatients with a wide range in level of communication disturbance. We administered tests of sustained attention, simple sequencing, complex sequencing, and conceptual sequencing to the patients and to nonpsychiatric comparison subjects and assessed participants’ speech for six different types of communication failure, four of them structural and two nonstructural. We hypothesized that 1) the patients would show poorer performance than comparison subjects on all the cognitive measures, and their speech would contain higher frequencies of each of the six types of communication failure; 2) poor sustained attention would be related to all six types of communication failure; 3) poor sequencing and conceptual sequencing would make additional contributions to the variance in the structural failures but not the nonstructural failures; and 4) performance on the measures of attention, sequencing, and conceptual sequencing would account for a substantial amount of the variance in the structural communication failures.
Method
Participants
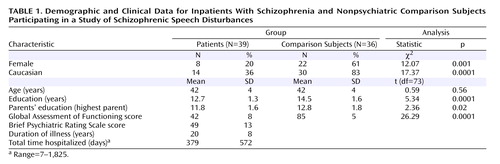
Table 1 presents basic demographic and clinical data for patients and comparison subjects. The patient group consisted of 39 inpatients in a Department of Veterans Affairs (VA) hospital who met DSM-IV-TR criteria for schizophrenia. They were drawn from the schizophrenic subset of a sample examined in a larger study of language disturbances in psychiatric inpatients (14) . They were severely and chronically ill individuals who had been living in community, nursing care, or family care settings and had been rehospitalized because of an acute exacerbation of psychotic symptoms. The patients’ level of functioning at the time of testing ranged from moderately to severely impaired according to the Global Assessment of Functioning Scale (GAF). We excluded patients who had a history suggestive of possible neurological disease or damage, a history of solvent abuse, or a history of alcohol dependence severe enough to have required detoxification and patients who met criteria for any kind of substance abuse or dependence during the past year. Eighteen patients had earlier histories of substance abuse (alcohol [N=15], cocaine [N=10], heroin [N=1], and marijuana [N=1]). Patients whose first language was not English were excluded because the study used measures of natural speech. We also excluded patients whose speech was so extremely disordered that it could not be divided reliably into discrete instances and types of communication failure. All patients were receiving psychotropic medication; 20 were receiving conventional antipsychotics, 17 were receiving atypical antipsychotics, and two were not receiving antipsychotic medication. Ten also received anticholinergics; eight, mood stabilizers; eight, antidepressants; and 12, anxiolytics.
Comparison subjects were 36 state university employees from the civil service sector, which includes food service, maintenance, and other workers on campus. The exclusion criteria for the patient group also applied to comparison subjects. In addition, potential participants who reported ever having experienced psychotic symptoms were excluded.
Procedures
The study was approved by the institutional review boards of Kent State University and the Louis Stokes Cleveland VA Medical Center. The procedures of the study were fully explained to each participant, and written informed consent was obtained; for individuals who had guardians, consent was also obtained from the guardians. The interviews, tests, and symptom ratings were then carried out by four doctoral student research assistants who were trained on all the measures. Interviewers attained good levels of interrater reliability on all the scales prior to the study, and their ratings were monitored periodically to guard against drift.
Clinical Measures
The Schedule for Affective Disorders and Schizophrenia—Lifetime Version (SADS-L, 17), adapted slightly for use with DSM-IV criteria, was administered to each patient and comparison subject. A clinical psychologist with extensive research diagnostic experience made the final diagnoses on the basis of the information from these interviews and from hospital records.
Level of functioning was measured with the GAF from DSM-IV-TR. GAF scores were used in some of the analyses to control for generalized deficit effects. Co-ratings of 10 patients indicated a high intraclass correlation on this measure (intraclass correlation coefficient [ICC]=0.93).
Symptom severity was rated with the Brief Psychiatric Rating Scale (BPRS) (18) . The severity of illness index was calculated as the sum of all BPRS subscale scores except the conceptual disorganization subscale. This subscale was excluded to avoid overlap with the measure of communication disturbances, because the index was used to test correlations between severity of illness and communication disturbances. Co-ratings of 10 patients indicated good interrater reliability (ICC=0.90).
Speech Measures
A 10-minute conversational speech sample was obtained from each participant on topics such as daily activities, routines, hobbies, and leisure activities. Emotional topics were avoided because speech disorder may be exacerbated by arousal of negative emotion in some patients (19) . The interviewers asked relevant, open-ended questions and made comments as necessary to keep participants talking and to direct them away from emotion-laden topics. Speech samples were audiotaped and later transcribed and proofread for accuracy.
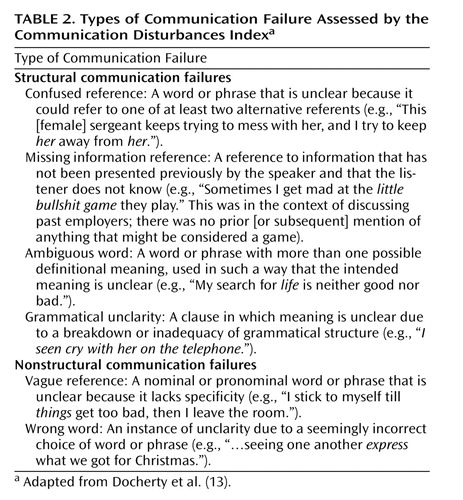
The transcribed speech samples were rated using the Communication Disturbances Index (13) . The variables assessed by this instrument are defined and illustrated in Table 2 . The Communication Disturbances Index is related to measures of formal thought disorder (20) and linguistic structure (10) , but it focuses explicitly on failures in the communication of meaning in speech rather than on underlying thought disorder or language structural weaknesses as such. The total number of words is tallied, instances of communication failure are counted, and the frequency of each type of communication failure per 100 words of speech is calculated. Instances of disturbance are counted only if they render an utterance ambiguous or obscure in meaning. Thus, for example, wrong words are counted only if the speaker’s intended meaning is not clear; grammatical failures are counted only if the poor grammar makes the meaning difficult to ascertain; vague references are counted only if their lack of specificity impairs comprehension of the intended meaning.
Four types of failures are structural, in the sense that they reflect errors that are interclausal. They are utterances that are unclear in meaning because of problems in relationships between different segments, or clauses, of the speech. These include the confused reference—unclear because its referent, although present in another clause in the speech, is not clearly identifiable as the intended referent because of structural characteristics of the speech; the missing information reference—structural because it makes reference to an earlier referent, but the earlier referent, which should be in a previous clause, is absent; the ambiguous word—structurally deficient in its lack of context; and the grammatical unclarity—unclear because of structural breakdown. The two nonstructural failures are the vague reference and wrong word usage. They are nonstructural because they are words or phrases that are themselves unclear, without reference to other segments or clauses of the speech.
Speech samples were rated blindly by two individuals trained in the method. One rated all the speech samples, and the second rated 20 samples that were randomly selected within groups. Interrater reliability computed for the 20 co-rated speech samples was acceptable for all six types of communication failure. Intraclass correlations were as follows: confused references, ICC=0.92; missing information references, ICC=0.83; ambiguous words, ICC=0.84; grammatical unclarities, ICC=0.82; vague references, ICC=0.78; wrong words, ICC=0.87; total structural failures, ICC=0.92; total nonstructural failures, ICC=0.88.
Cognitive Measures
The test of sustained attention was a visual continuous performance task (21) . Clearly defined (i.e., undegraded) black digits appeared on a white screen, one at a time, at a rate of one per second, for 8 minutes. Subjects were instructed to press a button every time the target digit appeared. Sensitivity scores were used as the measure of sustained attention. These scores take into account both hit rate and false alarm rate. The test consists of six blocks of 80 trials.
Simple sequencing ability was measured with the Trail Making test A (22) , which requires the subject to draw a line linking sequential numbers that are scattered on a page; performance is measured as time to completion of the task. More complex sequencing ability was assessed with the Trail Making test B (22) , which is similar to test A except that it requires subjects to link alternating numbers and letters. This test has a heavier working memory load than test A, and it also requires the ability to shift back and forth between two sets in order to sequence the items correctly. Performance is measured as time to completion. An upper limit of 6 minutes was allowed; for participants who had not completed the test by then, the maximum score (360 sec) was assigned.
Conceptual sequencing was measured with the abstraction subtest of the Shipley Institute of Living Scale (23) . In this test, the beginnings of 20 different sequences of numbers or letters are presented and subjects are asked to complete the sequences. Each sequence is based on a different overarching concept. Completion of a sequence requires identification of the concept and generation and ordering of smaller concepts (numbers or letters) in the service of the larger concept. Subjects were given 10 minutes to complete the test. The range of possible scores is 0 to 40.
Analysis
Distributions of the communication disturbance variables and the Trail Making test A scores were positively skewed, so they were log-transformed for the analyses. Scores on visual continuous performance task sensitivity were negatively skewed, so they were exponentially transformed. The analysis was done in three parts. First, patients and comparison subjects were compared on Communication Disturbances Index ratings and cognitive test performance. Next, correlations were computed between cognitive test performance and the measures of speech disorder in the patients. Finally, the individual contributions of cognitive impairments to each type of speech disorder were assessed by means of regressions in which the cognitive measures were entered in ascending order of complexity as predictors of each speech disorder variable. A control for generalized impairment effects was applied. All reported p values are two-tailed.
Results
Cognitive and Communication Variables
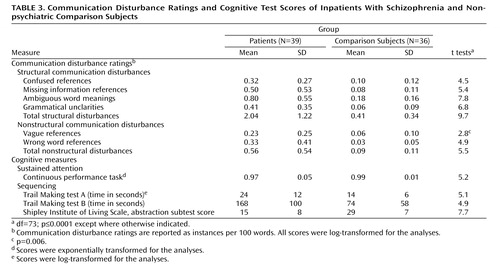
Communication disturbance ratings and cognitive test scores for patients and comparison subjects are presented in Table 3 . Analyses of variance were used to compare the two groups on the measures of communication disturbance and cognitive functioning. Although the comparison subjects’ speech contained instances of all six types of communication failure, the patients’ speech contained much higher frequencies of every type. Patients also performed significantly worse than comparison subjects on all four cognitive tests.
Demographic Group Differences
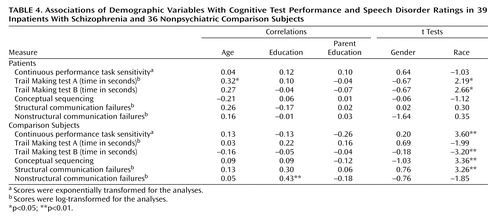
The patient and comparison groups differed in gender and ethnic composition, education, and parental education. Associations of these demographic variables with communication failures and neurocognitive test performance in each group are presented in Table 4 . Gender and parental education were unrelated to the speech or cognitive variables in both groups. Level of education was related only to the speech variables, and only in the comparison group; comparison subjects with more education made more frequent communication failures. In the comparison group, African American participants performed more poorly on the cognitive tests and speech measures than Caucasians. In the patient group, however, African American participants tended to perform better than the Caucasians. This difference reached statistical significance on both Trail Making tests. Within racial groups, Caucasian patients performed significantly and substantially more poorly than comparison subjects on all the measures. Among African Americans, patients also performed more poorly, but the differences were smaller and nonsignificant.
Medication Effects
Patients receiving atypical antipsychotics performed better than other patients on the test of conceptual sequencing (mean=19.5 [SD=10.0] versus mean=12.5 [SD=6.6]; t=2.45, df=37, p<0.02). Patients receiving anticholinergics performed more poorly than other patients on the Trail Making test B (mean=237 [SD=119] versus mean=145 [SD=84]; t=2.65, df=37, p<0.02). There were no other associations between medications and the language or cognitive variables.
Correlations Between Cognitive and Communication Variables
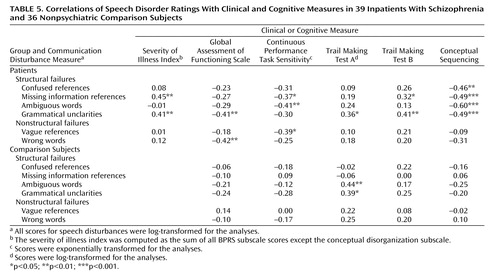
Correlations between communication disturbance ratings and cognitive test scores in the patient and comparison groups are presented in Table 5 . As expected, in the patient group communication failures were related negatively to performance on the test of attention, supporting the idea that attentional impairment affects the ability to produce coherent speech. The associations with attentional functioning were statistically significant for some types of communication disturbances and not others, but there was no real indication of specificity. All the correlations were in the same direction, and the differences between the correlation coefficients, assessed using t tests for correlations in correlated samples, were not significant. The sequencing tests, on the other hand, were related to structural communication failures and not nonstructural ones. Grammatical unclarities, the most structural type of disturbance of all, were significantly related to all three measures of sequencing. Furthermore, all four of the structural disturbances were strongly related to conceptual sequencing, the most complex type of sequencing assessed. The difference in the correlations between conceptual sequencing and total structural versus nonstructural failures was significant (t=4.79, df=72, p<0.001). In the comparison group, the associations paralleled those in the patient group but were smaller and mostly nonsignificant. Fisher r-to-z tests indicated that the association between total structural failures and conceptual sequencing was significantly higher among patients than comparison subjects (z=2.79, p<0.01).
Contributions of Attention and Sequencing Impairments to Speech Disorders
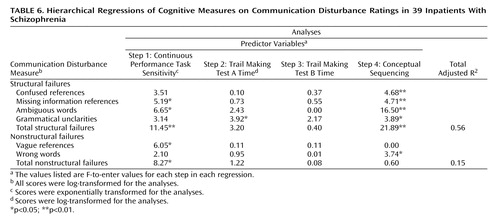
Cognitive functions are not independent of each other. Higher-level capacities may be expected to depend at least in part on lower-level processes. For example, in this study, the continuous performance task was the measure of sustained attention, but sustained attention is also necessary for the higher-level process of sequencing. Thus, poor attention will affect performance on the continuous performance task and also on the test of simple sequencing. Similarly, both attention and simple sequencing capacity are necessary for complex and conceptual sequencing. To examine the individual contributions of each cognitive weakness to speech disorder, including the contributions of impairments in higher-level cognitive processes beyond the effects of weaknesses in lower-level processes, we computed hierarchical regressions on each type of speech disorder. Cognitive test scores were entered in order of complexity, as follows: continuous performance task, Trail Making test A, Trail Making test B, and conceptual sequencing. The dependent variables were the communication failure ratings. The results of these regressions are presented in Table 6 .
Several of the structural and nonstructural communication disturbances took significant contributions from the scores on the test of attention. Scores on simple and complex sequencing, generally speaking, contributed little to the speech variables, structural or nonstructural, beyond the effects of attention, except for a significant effect of simple sequencing on grammatical unclarities. However, as expected, scores on conceptual sequencing made a significant contribution to the frequency of each of the structural speech variables beyond the effects of the lower-level tests and a substantial contribution to the summed frequency of all four types of structural communication failures. These cognitive tests, taken together, explained 56% of the variance in structural speech disorder. Both attention and conceptual sequencing made significant contributions to the total, with the largest part coming from conceptual sequencing. The nonstructural speech variables took much smaller contributions from conceptual sequencing. The effect on wrong word references was significant at a low level, but overall there was little relationship. The cognitive test scores accounted for 15% of the variance in the total frequency of nonstructural communication disturbances, and virtually all of this came from the measure of attention.
Consideration of Generalized Deficit Effects
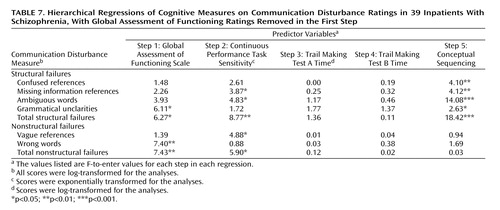
In looking for specific associations between cognitive functions and speech disorder, it is important to control for generalized deficit effects (24) . The differential in findings for the structural versus nonstructural failures supports the idea that the associations are specific rather than reflections of differences among subjects in global levels of impairment. However, we also took the precaution of factoring out a measure of global level of functioning by rerunning the regressions with GAF ratings entered in the first step, followed by the cognitive tests in the same order as before. These results are presented in Table 7 .
Global impairment was related to both structural and nonstructural failures, but the patterns of associations between the speech and cognitive variables were still generally the same even after removal of the effects of GAF score, except that the low-level association between the wrong-word disturbances and complex sequencing disappeared.
Discussion
The findings of this study provide solid evidence that impairments in attention and sequencing capacities are related to schizophrenic speech disorder. Deficient sustained attention contributed significantly to both structural and nonstructural communication failures, and deficient sequencing capacity, especially in the realm of conceptual sequencing, contributed substantially to structural communication failures beyond the effects of poor sustained attention. All of these associations were present even after differences among patients in global level of functioning were taken into account. Performance on the tests of attention, sequencing, and conceptual sequencing explained 56% of the variance in structural communication failures in patients’ speech. This is a very large proportion of the variance compared with previous findings on cognitive contributors to speech disorder (5) .
These strong findings support the efficacy of measuring speech disorder in terms of its effect, communicative impairment, at least for this purpose. The approach of dividing speech disorder into different types based on apparent differences in cognitive underpinnings was also supported, in that conceptual sequencing impairment was a major contributor to structural communication failures but not to nonstructural ones. Furthermore, even within the category of structural disturbances, the different types of failures were related to somewhat different cognitive impairment profiles. Future research might be able to delineate further the cognitive process contributors to specific types of communication failures by using a wider array of cognitive tests, perhaps including measures of working memory and concept formation, among other possibilities.
A possible alternative explanation for the relative strength of the associations found in this study compared with earlier efforts is that our measures of communication failures might assess speech disorder of a different type from that assessed by measures of thought disorder or linguistic structure, and it could be a type more highly related to attention and sequencing. The Communication Disturbances Index is associated with measures of formal thought disorder and structural abnormalities in language, but the associations are not particularly strong. However, the index, which counts instances of disorder solely on the basis of comprehensibility, was designed as much as possible to count all instances in which the conveyance of meaning is impaired for any reason. It counts loss of meaning for diverse reasons, including lack of specificity of words or phrases, lack of necessary referents, ambiguity of referents, use of unknown, ambiguous, or inaccurate words, and grammatical breakdown. From a loss-of-meaning perspective, it is a fairly comprehensive measure of speech disorder. For this reason we think it unlikely that the index simply measures more attention- and sequencing-dependent types of speech disorder than the other kinds of measures.
In the comparison subjects, the associations between cognitive and speech variables were smaller and generally nonsignificant. This may indicate that attentional and sequencing weaknesses have little impact on speech coherence unless they are relatively severe. It should be noted, however, that only the correlations between conceptual sequencing and structural failures were significantly higher in patients than in comparison subjects. Furthermore, the ranges of scores in the comparison group were smaller than in the patient group, which might have diminished correlations in the comparison group. Thus, it is possible that the associations observed in patients are also present in nonpatients to the same degree and that speech is more impaired in patients than in comparison subjects only because patients have more severe cognitive impairment.
In any case, the strong relationships between cognitive impairments in patients and speech disorder found with this limited battery of cognitive tests suggest that the bases of schizophrenic incoherent speech, or “formal thought disorder,” may not be particularly mysterious or obscure. These symptoms are probably largely, if not wholly, the natural consequence of marked deficits in a variety of basic cognitive functions, including, among others, simple sustained attention and conceptual sequencing capacity. If pharmacological and cognitive training interventions could be developed that targeted specifically these cognitive impairments as well as others that may be found to be related to communication failure, they could improve patients’ capacity to communicate, which could have profound positive effects on the quality of their lives.
1. Andreasen NC: Thought, language, and communication disorders. Arch Gen Psychiatry 1979; 36:1315–1321Google Scholar
2. Marengo J, Harrow M, Herbener ES, Sands J: A prospective longitudinal 10-year study of schizophrenia’s three major factors and depression. Psychiatry Res 2000; 97:61–77Google Scholar
3. Harvey PD, Docherty NM, Serper M, Rasmussen M: Cognitive deficits and thought disorder, II: an eight-month follow-up study. Schizophr Bull 1990; 16:147–156Google Scholar
4. Anthony WA, Rogers ES, Cohen M, Davies RR: Relationship between psychiatric symptomatology, work skills, and future vocational performance. Psychiatr Serv 1995; 46:353–358Google Scholar
5. Kerns JG, Berenbaum H: Cognitive impairments associated with formal thought disorder in people with schizophrenia. J Abnorm Psychol 2002; 111:211–224Google Scholar
6. Nuechterlein KH: Vigilance in schizophrenia and related disorders, in Neuropsychology, Psychophysiology, and Information Processing. Edited by Steinhauer SR, Gruzelier JH. New York, Elsevier, 2002, pp 397–443Google Scholar
7. Woelwer W, Gaebel W: Impaired Trail Making Test-B performance in patients with acute schizophrenia is related to inefficient sequencing of planning and acting. J Psychiatr Res 2002; 36:407–416Google Scholar
8. Docherty NM, Hall MJ, Gordinier SW, Cutting LP: Conceptual sequencing and disordered speech in schizophrenia. Schizophr Bull 2000; 26:723–735Google Scholar
9. Johnston MH, Holzman PS: Assessing Schizophrenic Thinking. San Francisco, Jossey-Bass, 1979Google Scholar
10. Sledge WH, Hoffman RE, Hawkins K, Docherty NM, Quinlan DM, Rakfeldt J: Linguistic deviance in schizophrenia: preliminary report, in Communication and Mental Illness. Edited by France J, Kramer S. New York, Jessica Kingsley, 2001, pp 371–392Google Scholar
11. Hoffman RE, Stopek S, Andreasen NC: A comparative study of manic vs schizophrenic speech disorganization. Arch Gen Psychiatry 1986; 43:831–838Google Scholar
12. Rochester SR, Martin JR: Crazy Talk: A Study of the Discourse of Schizophrenic Speakers. New York, Plenum, 1979Google Scholar
13. Docherty NM, DeRosa M, Andreasen NC: Communication disturbances in schizophrenia and mania. Arch Gen Psychiatry 1996; 53:358–364Google Scholar
14. Docherty NM: Cognitive impairments and disordered speech in schizophrenia: thought disorder, disorganization, and communication failure perspectives. J Abnorm Psychol 2005; 114:269–278Google Scholar
15. Harvey PD, Earle-Boyer EA, Levinson JC: Distractibility and discourse failure: their association in mania and schizophrenia. J Nerv Ment Dis 1986; 174:274–279Google Scholar
16. Barch DM, Berenbaum H: Language production and thought disorder in schizophrenia. J Abnorm Psychol 1996; 105:81–88Google Scholar
17. Spitzer RL, Endicott J: Schedule for Affective Disorders and Schizophrenia—Lifetime Version, 3rd ed. New York, New York State Psychiatric Institute, Biometrics Research, 1979Google Scholar
18. Lukoff D, Liberman RP, Nuechterlein KH: Symptom monitoring in the rehabilitation of schizophrenic patients. Schizophr Bull 1986; 12:578–593Google Scholar
19. Docherty NM: Affective reactivity of symptoms as a process discriminator in schizophrenia. J Nerv Ment Dis 1996; 184:535–541Google Scholar
20. Docherty NM, Gordinier SW: Immediate memory, attention, and communication disturbances in schizophrenia patients and their relatives. Psychol Med 1999; 29:189–197Google Scholar
21. Nuechterlein KH, Parasuraman R, Qiyuan J: Visual sustained attention: image degradation produces rapid sensitivity decrement over time. Science 1983; 220:327–329Google Scholar
22. Reitan RM, Davidson LA: Clinical Neuropsychology: Current Status and Applications. New York, Hemisphere, 1974Google Scholar
23. Zachary RA: Shipley Institute of Living Scale Revised Manual. Los Angeles, Western Psychological Services, 1986Google Scholar
24. Chapman LJ, Chapman JP: The measurement of differential deficit. J Psychiatr Res 1978; 14:303–385Google Scholar