Influence of Ethical Safeguards on Research Participation: Comparison of Perspectives of People With Schizophrenia and Psychiatrists
Abstract
OBJECTIVE: Several safeguards have been developed to protect research volunteers, but little is known about how the people involved in this research—the stakeholders—view these efforts to assure participant rights and well-being. The authors’ goal was to examine these perspectives. METHOD: As part of a larger study, 60 people with schizophrenia and 69 psychiatrists rated the protectiveness and influence on patients’ willingness to participate in research of five safeguards: informed consent, alternative decision makers, institutional review boards, data safety monitoring boards, and confidentiality measures. RESULTS: All safeguards were perceived by both the participants with schizophrenia and by the psychiatrists as protective: on a scale of 1–5 on which 1=not protective at all and 5=very much protects, the mean scores ranged from 3.54 to 4.07. Four of the five safeguards were perceived by both the people with schizophrenia and by the psychiatrists as positively influencing patients’ participation decisions. On a scale of 1–5 on which 1=much less willing and 5=much more willing to participate, the mean scores for these four safeguards ranged from 3.86 to 4.30. The mean score for the safeguard of an alternative decision maker, however, was 3.09. The ratings of protectiveness made by both the people with schizophrenia and the psychiatrists were correlated with their ratings of patients’ willingness to participate in studies. CONCLUSIONS: Ethical commitment to research volunteers is expressed in safeguards. These efforts appear to be viewed positively by key stakeholders and may influence research participation decision making.
The principles of respect for individuals, beneficence, and justice together serve as the ethical foundation for serious illness research involving human volunteers (1). Over the past three decades, these principles have found their real-world translation in the safeguard practices of investigators and institutions (2). Informed consent procedures, inclusion of alternative decision makers, review by institutional review boards and, more recently, by data safety monitoring boards, and confidentiality safeguards represent five of the most salient ethical practices that have been developed.
In the United States, extraordinary effort is committed to the implementation of these safeguards, especially in higher-risk protocols or in studies requiring enrollment of subjects with greater potential vulnerability in the research situation (2–6). It is hoped that these safeguards will help assure the rights and well-being of people with serious mental illness, who may have very severe symptoms or fluctuating decision-making abilities and who are at risk for stigma, poverty, institutionalization, and limited access to care (2–7). Little is known, however, about how key stakeholders view these safeguards regarding their protectiveness or effect on decision making regarding research participation. Our goal was to explore these perspectives.
Method
For this institutional-review-board-approved, NIMH-funded study, we developed a questionnaire including 298 quantitative scaled questions and six qualitative items for people with schizophrenia. The instrument assessed views of ethically important considerations in mental illness research and related areas. People with schizophrenia were recruited by community outreach or physician referral. Diagnosis was confirmed by chart review. A trained interviewer administered the survey by reading each question and recording responses. Most participants completed the survey in 2.5 to 3 hours, which sometimes occurred over more than one session to minimize fatigue.
For the portion of the study presented in this report, we carefully described five safeguard activities in simple, neutral, and straightforward terms. The participant was asked to evaluate the protectiveness of the activities and to indicate the influence of the activities on their willingness to participate in a research protocol.
An abbreviated written questionnaire was developed for psychiatrists. They were asked to evaluate the protectiveness of the activities and to predict their influence on patients’ willingness to participate in research. All faculty and resident psychiatrists at the University of New Mexico School of Medicine (N=105) were invited to participate; 69 (66%) did so.
Data were confidentially encoded. All participants received $30.
The 5-point rating scale responses were subjected to repeated-measures multivariate analysis of variance (MANOVA) with rater group (people with schizophrenia versus psychiatrists) and gender as between-subjects independent variables. The demographic composition of rater groups was compared by using Pearson’s chi-square analysis. Repeated-measures dependent variables were correlated for each safeguard within rater groups by using Pearson’s correlations (r). Effect size was reported as Cohen’s d (the standardized difference between means).
Results
Forty-eight (80%) of the 60 participants with schizophrenia were men and 54 (90%) were unmarried. Their mean age was 44.3 years (SD=10.7). The majority (N=36 [60%]) were white, and 13 (22%) were of Hispanic origin. Scores on the Brief Symptom Inventory (8) ranged from 0 to 3.77; mean=1.37 for global severity; mean=1.57 for psychoticism, mean=1.55 for paranoid ideation, mean=1.49 for anxiety, mean=1.46 for depression, and mean=1.43 for interpersonal sensitivity. All participants had adequate reading and auditory comprehension for our project as measured by the Woodcock Reading Mastery Test (9) and the Boston Diagnostic Aphasia Examination (10).
Thirty-eight (55%) of the 69 participating psychiatrists were men and 49 (71%) were married or living with a partner; their mean age was 42.4 (SD=10.9). The psychiatrists and patients differed significantly in gender composition (χ2=8.97, df=1, p<0.01), marital status (χ2=50.09, df=1, p<0.001), and ethnicity (χ2=17.58, df=1, p<0.001).
People with schizophrenia and psychiatrists rated the protection of the five safeguard activities on a scale of 1=not protective at all to 5=very much protects (Figure 1). All five were perceived as protective (means ranged from 3.54 to 4.07). Confidentiality protection, institutional review boards, informed consent, and data and safety monitoring boards were rated as more protective (means ranged from 3.82 to 4.07) than alternative decision makers (mean=3.54) (F=4.27, df=4, 122, p<0.01, for safeguard item main effect; maximum Cohen’s d=0.45).
Psychiatrists rated strict confidentiality as more protective than other safeguards (mean=4.16 versus means ranging from 3.62 to 3.88) (simple effect, least significant difference p<0.05; maximum d=0.52). People with schizophrenia rated alternative decision makers as less protective than other safeguards (mean=3.46 versus means ranging from 3.88 to 4.14) (simple effect, least significant difference p<0.05, maximum d=0.53). Perceived protectiveness did not differ by gender (MANOVA main effect p<0.15) or by rater group (MANOVA main effect p<0.79).
People with schizophrenia rated the influence of the safeguards on their willingness to volunteer for research on a 5-point scale on which 1=much less willing, 3=no influence, and 5=much more willing, and psychiatrists predicted the influence of these safeguards on patients’ willingness to volunteer (Figure 1). Patients rated four of the activities as increasing their willingness to participate in research (means ranged from 3.86 to 4.30), but they rated alternative decision makers as having no influence (mean=3.09) (F=25.38, df=4, 122, p<0.0001, for item effect; maximum d=1.13). Psychiatrists’ ratings matched those of the people with schizophrenia (i.e., there was no rater effect, MANOVA p<0.89). Ratings did not differ by gender (MANOVA main effect p<0.71).
Perceived protectiveness was correlated with influence on willingness to participate in research for both rater groups, more strongly for people with schizophrenia (mean r=0.61, N=60, range=0.51–0.76, all p<0.001) than for psychiatrists (mean r=0.35, N=69, range=0.24–0.48, all p<0.05).
Discussion
Understanding the perspectives of individuals with serious mental illness is an important commitment for mental illness researchers who seek to uphold ethical principles in their work. Efforts to safeguard the rights and well-being of research volunteers represent the concrete expression of these principles in everyday protocol practices. In this small but novel project, we found that people with schizophrenia and psychiatrists both saw all five safeguard efforts as protective and that they perceived four of the five as influencing patients’ decision making regarding research participation.
We wish to highlight four points, all of which may be seen as “double-edged.” First, our data suggest that safeguard efforts inspire the confidence of prospective research volunteers and that accurate information about safeguards may facilitate protocol recruitment. Further empirical work is needed, however, to demonstrate that our participants’ beliefs about the effectiveness of safeguards are not misplaced (3, 4, 6, 11). Second, safeguard activities are fully dependent on the judgment, knowledge, and skills of the individuals who enact them. It is of concern that psychiatric researchers and their staff may have little preparation for the ethically sensitive aspects of their work (12, 13). Third, in this study, alternative decision makers were seen by people with schizophrenia as only mildly protective and as not influential. Psychiatrists had the same view. Because proposed policies regarding mental illness research rely on the inclusion of alternative decision makers, however, we must learn about the situations in which alternative decision makers will be seen as acceptable and valuable by participants (4, 7). Finally, this project relies on self-report data, and the findings may not generalize to other groups. We hope that this early work with key stakeholders will inspire further study of safeguard practices in mental illness research.
Received Dec. 9, 2003; revision received April 29, 2004; accepted May 17, 2004. From the Department of Psychiatry and Behavioral Medicine, Medical College of Wisconsin, Milwaukee; and the Health Sciences Center Institute for Ethics and the Department of Family and Community Medicine, University of New Mexico, Albuquerque. Address reprint requests to Dr. Roberts, Department of Psychiatry and Behavioral Medicine, Medical College of Wisconsin, 8701 Watertown Plank Rd., Milwaukee, WI 53226; [email protected] (e-mail). Supported by NIMH Career Development Award 1K02 MH-01918 and by National Institute on Drug Abuse grant 1R01 DA-13139.
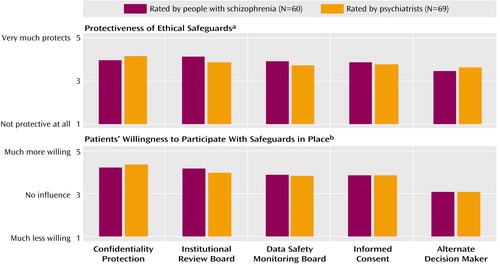
Figure 1. Ratings of Research Safeguards by People With Schizophrenia and Psychiatrists
aThere was a significant main effect for safeguard (p<0.01) but not for rater (person with schizophrenia or psychiatrist) (p<0.79) in the repeated-measures multivariate analysis of variance (MANOVA) using safeguard as a repeated measure and rater and gender as independent variables.
bThere was a significant main effect for safeguard (p<0.0001) but not for rater (person with schizophrenia or psychiatrist) (p<0.89) in the repeated-measures MANOVA.
1. National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research: The Belmont Report: Ethical Principles and Guidelines for the Protection of Human Subjects of Research. Washington, DC, US Government Printing Office, 1979Google Scholar
2. Brody B: The Ethics of Biomedical Research: An International Perspective. New York, Oxford University Press, 1998Google Scholar
3. Faden RR: Human-subjects research today: final report of the Advisory Committee on Human Radiation Experiments. Acad Med 1996; 71:482–483Crossref, Medline, Google Scholar
4. Dresser R: Mentally disabled research subjects: the enduring policy issues. JAMA 1996; 276:67–72Crossref, Medline, Google Scholar
5. Roberts L, Roberts B: Psychiatric research ethics: an overview of evolving guidelines and current ethical dilemmas in the study of mental illness. Biol Psychiatry 1999; 46:1025–1038Crossref, Medline, Google Scholar
6. Preserving the Public Trust: Accreditation and Human Research Participant Programs. Washington, DC, Institute of Medicine, 2001Google Scholar
7. National Bioethics Advisory Commission: Research Involving Subjects With Mental Disorders That May Affect Decisionmaking Capacity. Rockville, Md, National Bioethics Advisory Commission, 1998Google Scholar
8. Derogatis LR, Melisaratos N: The Brief Symptom Inventory: an introductory report. Psychol Med 1983; 13:595–605Crossref, Medline, Google Scholar
9. Woodcock Reading Mastery Test. Circle Pines, Minn, American Guidance Service, 1998Google Scholar
10. Goodglass H, Kaplan E: Boston Diagnostic Aphasia Examination. New York, Psychological Corp, 1972Google Scholar
11. Shamoo AE: Ethics in Neurobiological Research With Human Subjects. Amsterdam, Gordon and Breach, 1997Google Scholar
12. Rosenstein DL, Miller FG, Rubinow DR: A curriculum for teaching psychiatric research bioethics. Biol Psychiatry 2001; 50:802–808Crossref, Medline, Google Scholar
13. Roberts LW, McCarty T, Lyketsos C, Hardee JT, Jacobson J, Walker R, Hough P, Gramelspacher G, Stidley CA, Arambula M, Heebink DM, Zornberg GL, Siegler M: What and how psychiatry residents at ten training programs wish to learn ethics. Acad Psychiatry 1996; 20:131–143Crossref, Medline, Google Scholar



