Skills Training Versus Psychosocial Occupational Therapy for Persons With Persistent Schizophrenia
Abstract
OBJECTIVE: The authors compared the community functioning of outpatients with persistent forms of schizophrenia after treatment with psychosocial occupational therapy or social skills training, with the latter conducted by paraprofessionals. METHOD: Eighty outpatients with persistent forms of schizophrenia were randomly assigned to receive either psychosocial occupational therapy or skills training for 12 hours weekly for 6 months, followed by 18 months of follow-up with case management in the community. Antipsychotic medication was prescribed through “doctor's choice” by psychiatrists who were blind to the psychosocial treatment assignments. RESULTS: Patients who received skills training showed significantly greater independent living skills during a 2-year follow-up of everyday community functioning. CONCLUSIONS: Skills training can be effectively conducted by paraprofessionals, with durability and generalization of the skills greater than that achieved by occupational therapists who provide their patients with psychosocial occupational therapy. (Am J Psychiatry 1998; 155:1087–1091)
While the efficacy of social skills training in schizophrenia appears well established (1–8), most studies have been conducted in medical school departments of psychiatry with augmented staff who were specially prepared as trainers. Moreover, most of the efficacy trials have used “customary treatment” as the control group. Three major questions that remain largely unanswered are, Can social skills training be effectively conducted by paraprofessionals in an ordinary clinical setting? Do the skills learned in clinic training sessions generalize to the outside world? and Are the effects of skills training discernible when an active comparison group is used?
In most psychiatric hospitals and day hospitals, the prevailing psychosocial treatment is occupational therapy in which expressive art and crafts and recreational activities are the media through which therapists build self-esteem and productivity. However, there have been few empirical evaluations of the efficacy of this approach (9). At the West Los Angeles Veterans Administration (VA) Medical Center, hundreds of patients with serious mental disorders receive this modality each year. In 1981, the VA Central Office established a new form of psychosocial treatment by funding a demonstration program, at the West Los Angeles VA Medical Center, for training in social and independent living skills. Subsequently, a health services research study was begun at this medical center to compare the relative impact of occupational therapy and skills training on persons with persistent and long-term schizophrenia. We shall report the first results from this study in the present article.
METHOD
Subjects
Cohorts of 10–12 outpatients with persistent and unremitting forms of schizophrenia were entered into the study through a randomization procedure that assigned half to psychosocial occupational therapy and half to skills training at the West Los Angeles VA Medical Center. A total of 84 male patients were assigned to receive 6 months of intensive, clinic-based treatment 3 hours per day, 4 days per week. They were seen approximately once per month by psychiatrists who were blind to the psychosocial treatment assignment and who prescribed antipsychotic medication and adjunctive medications by “doctor's choice.” Medication tended to produce some stability in patients' symptoms, but few went into full remission during the study; thus, the assessment of discrete episodes of symptom exacerbation or relapse was not feasible.
Almost all of the subjects were never married; were living in community-based, board-and-care homes; and had one or more persisting psychotic symptoms (i.e., suspiciousness, unusual thoughts, hallucinations, grandiosity, conceptual disorganization) rated as moderate or higher on the Expanded University of California, Los Angeles (UCLA), Brief Psychiatric Rating Scale (BPRS) (10). The average age of the subjects was 37.1 years (SD=8.8), their average education amounted to 12.3 years (SD=1.9), and the average duration of illness was 14.8 years (SD=8.0). Sixty-six percent were Caucasian, 25% were African American, and the remainder were either Hispanic or Asian. There were no significant differences in these background variables between the patient cohorts assigned to the two psychosocial conditions (p values ranged from 0.14 to 0.41; all comparisons were by t test except ethnicity, which was by chi-square).
Written informed consent was obtained after the procedures were fully explained to the subjects and repeated back by them to the investigators. The research procedures were approved by the Medical Center's Research and Human Subject Protection Committee according to the appropriate institutional guidelines. Subjects were free to withdraw from the research protocol at any time without prejudicing their access to treatment elsewhere. Attrition was minimal; only 14 of 84 subjects dropped out during the 2-year period (four in the control group and 10 in the social skills training group; χ2=2.44, df=1, p=0.12). Almost all of the dropouts were accounted for by individuals moving to new geographical areas of the state or country and becoming unavailable for assessments. Attrition was minimized by the continuing care contacts provided by the clinical case managers and the availability of van transportation, lunches, and a “drop-in” socialization center for subjects.
Psychosocial Treatment Conditions
Psychosocial occupational therapy was led by three certified occupational therapists and comprised expressive, artistic, and recreational activities that mediated supportive therapy (9, 11). Patients participated individually and in groups, with encouragement by the therapists to individualize their interests and abilities through arts and crafts, discussion of feelings, and articulation of personal goals.
The skills training was conducted by an occupational therapist and three paraprofessionals who took turns in leading four modules of the UCLA Social and Independent Living Skills Program—basic conversation, recreation for leisure, medication management, and symptom management. Each module consisted of a trainer's manual, a participant's workbook, and a demonstration video; these are described in detail elsewhere (12).
Each module consisted of segments or “skill areas,” and each skill area included specific educational objectives. For example, in the medication management module, the skill area on “identifying benefits of antipsychotic medication” focused on teaching participants to make polite requests of their doctors regarding the type, dose, and benefits of medication. Appendix 1 lists the skill areas for the four modules used in this study.
The faithfulness and consistency of the module leaders to the procedures in the trainer's manuals were rated weekly by their supervisor through use of an observational checklist, and feedback was given as needed to maintain high levels of fidelity. In addition, tests of knowledge and skill related to the modules were administered after training to a subset of subjects from both treatment conditions to assess learning during the intensive phase. There was a highly significant posttraining difference across the 2-year follow-up period (main effect: F=21.05, df=1,56, p<0.0001) favoring the subjects in the skills training condition. Mean scores on the knowledge test were 21.4 for the social skills training group and 13.8 for the control group (both standard errors=1.2). The interaction of treatment by month (6, 12, and 24 months) was not significant (F<1, df=2,54, p=0.47), indicating that knowledge differences were stable across the follow-up period.
There were no significant differences between the chlorpromazine equivalents of antipsychotic drugs prescribed by the psychiatrists for the subjects in the two treatment conditions over the 2-year follow-up period; doses averaged 375.8 and 392.4 mg of chlorpromazine equivalents for the skills training and occupational therapy conditions, respectively. A wide variety of antipsychotic drugs and doses were used, with doctor's choice liberally used to facilitate optimal symptom control in these persistently psychotic outpatients. Treating psychiatrists were asked to identify the psychosocial treatment conditions for each patient under their care at the end of the 2-year study. None of the psychiatrists was able to designate patients at a better than chance level; their cumulative correct and incorrect ratings were 48 and 32, respectively.
Case Management
At the end of the intensive phase, each subject was assigned to a community case manager; case managers received subjects at random from the two psychosocial treatment conditions. The case managers' role and responsibilities included 1) establishing a therapeutic alliance, 2) providing crisis intervention and liaison with the treating psychiatrist, 3) encouraging the continued use of the patient's intensive treatment in community life (i.e., the skills training subjects were encouraged to use their skills in everyday life, and the occupational therapy subjects were encouraged to continue expressive activities in the community), and 4) consulting with social service and other community agencies (e.g., housing, entitlements) to facilitate the tenure and successful survival of the individual in the community. Each episode of interaction between case manager and subject was coded on a contact sheet that assigned times to the various domains of interaction. Post hoc analysis of the contact sheets revealed that most of the case managers' time was spent on responsibilities 1, 2, and 4. There were no differences in the domain-specific or total contact times between the two psychosocial conditions.
In designing this treatment trial, we were faced with the choice of having the same case managers providing services to patients from both intensive psychosocial treatment conditions (in which case the personalities of the case managers would be controlled) or having different case managers providing services to patients representing each of the two intensive psychosocial treatments (in which case bias for the respective psychosocial treatments might have been minimized). We chose the former design element because of cost constraints and because we wanted the crisis intervention skills, general relationship counseling skills, and other clinical competencies to be as similar as possible across the two psychosocial treatment conditions. We realize that bias may have played a part in this design, but the case managers were chosen for their commitment to clinical versus research values (13), and they were accountable to the clinical psychiatrists on this study who were blind to the psychosocial treatment conditions of the patients. In addition, the investigators wanted to give priority to the “services research” aspects of the study, making it as realistically applicable to “real-life” clinical settings as possible (14).
Assessments
The major assessment instrument for utilization of skills in everyday life was the Independent Living Skills Survey (15). With this instrument, the subject is queried about specific activities engaged in during the preceding 6-month period. Dimensions that are tapped by this survey include use of public transportation, money management, job seeking, and social relations. These dimensions were not all isomorphic with the skills targeted for training; hence, the Independent Living Skills Survey is best viewed as a measure of utilization of skills, not necessarily reflecting on a one-to-one basis the training goals. This instrument, as well as others, was administered at baseline, after the 6-month intensive phase, and at 6-month intervals thereafter.
Other, more general, instruments of social functioning were used, such as the Social Activities Scale, the Profile of Adaptation to Life, and the Global Assessment Scale (GAS). The Expanded BPRS (10), Brief Symptom Inventory, Rosenberg Self-Esteem Scale, and Lehman Quality of Life Scale were also administered. Blindness of the prescribing psychiatrists and assessors was promoted by geographically distancing the treatment program from the locales for pharmacotherapy and ratings of outcome and by repeatedly instructing the subjects to refrain from mentioning their psychosocial treatment to their psychiatrist and assessor.
The principal statistical design for the comparison of group outcomes was a mixed model, repeated measures analysis of covariance. When baseline data were available, the dependent variables were raw change scores from baseline. The analytic design was a 2×3 factorial, including main effects of treatment condition (social skills training versus occupational therapy) and follow-up phase (6, 12, and 24 months) and their interaction; baseline level and cohort differences were controlled. Because the dependent measures were change scores (adjusted for baseline), treatment group main effects indicate stable group differences in the amount of change during follow-up. Interactions of group by time would indicate lack of stability of those differences during the follow-up period. Separate subscales were analyzed in separate statistical analyses. As a follow-up to any finding of statistically significant treatment effects, t tests were computed to compare treatment groups at each follow-up point. Separate within-group t tests were used to assess significance of change over time (these within-group effects were estimated at the follow-up midpoint, or at approximately 1 year).
RESULTS
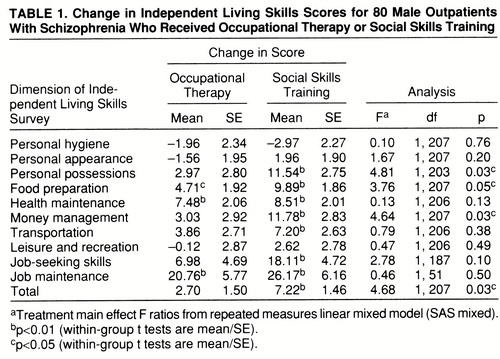
Major results are summarized in tables 1 (independent living skills), 2 (psychosocial functioning), and 3 (psychopathology). The cohort receiving skills training showed significantly greater improvement averaged across the 2-year follow-up period for total scores on the Independent Living Skills Survey (table 1). Although the interaction of treatment by time was not close to statistically significant, we did observe that differences between the treatment groups were most pronounced at 6 months, when treatment had just ended (F=4.93, df=1,246, p=0.03), and steadily decreased over time (12 months: F=2.19, p=0.14; 24 months: F<1, p=0.42; 36 months: F<1, p=0.83, all df=1,246). Several of the subscales of the Independent Living Skills Survey also showed a statistically significant advantage for the skills training group averaged across the follow-up period, including management of personal possessions, food preparation, and money management. While several other subscales of the survey did not reach statistically significant differences between treatment conditions, they did show statistically significant improvement from baseline averaged across the posttreatment period only within the skills trained group (p=0.05 or less), including health maintenance, use of transportation, job seeking, and job maintenance.
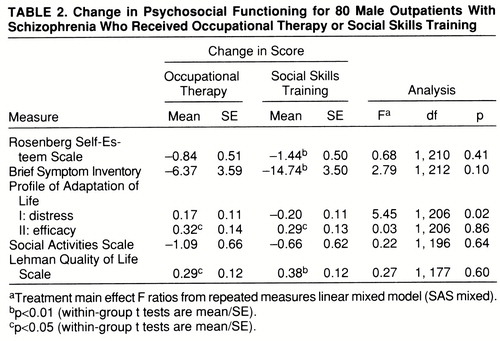
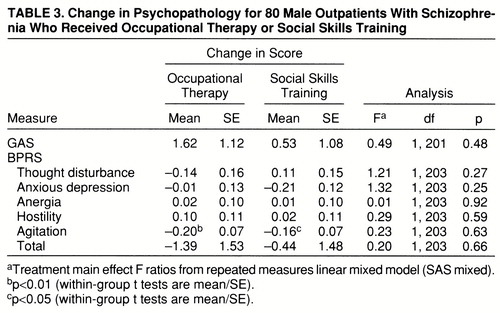
The skills trained group also showed significantly greater improvement than the occupational therapy group during follow-up in the distress factor I of the Profile of Adaptation to Life (table 2). Several other instruments reflected statistically significant pretreatment to posttreatment improvement only within the skills trained group; these included the Self-Esteem Scale and the Brief Symptom Inventory. While pretreatment to posttreatment improvements were noted for both treatment conditions on the Social Activities Scale, the GAS, and the BPRS, none was statistically significant in favor of the skills training condition. There were no significant differences between the treatment groups on any BPRS factors (table 3). Statistically significant improvement in both groups was observed on the BPRS agitation subscale, which encompasses the items excitement, tension, and mannerisms and posturing.
DISCUSSION
One of the controversies that has surrounded the use of social skills training in schizophrenia has focused on the question of generalization of the skills learned in training sessions into the everyday life of patients. The present study replicates the generalization of social skills training found in a recently published study that compared supportive group therapy with training in medication management, symptom management, and social problem solving (16). In that study, self-reported social functioning in the community was measured with the Social Adjustment Scale. Another controlled study of social skills training, which used the Katz Adjustment Scale, found generalization of skills training during hospitalization into community life following discharge (17).
This study can be added to the meta-analyses of controlled studies of social skills training that found evidence for a significant effect size in generalization (6, 7). The findings of improvement in social functioning for those trained in social skills from the present study are even more noteworthy given the marked persistence of psychotic symptoms in most subjects throughout the 2-year study. In addition, subjects had problems with distractibility, poor attention span, and memory deficits. The failure of some investigators to document generalization of social skills training may derive from their failure to appreciate the learning disabilities of schizophrenic patients and the consequent need for training procedures to overcome these disabilities through 1) lengthy and repetitive training sessions that are measured in months or years, not weeks; 2) opportunities and encouragement to practice the skills in real life; and 3) reinforcement for the use of the skills in community life.
For example, unless an individual has opportunities and encouragement in the community to use the self-management and self-administration of medication learned in the medication management module, there is little reason to expect generalization to occur. Community case managers were a key element in the present study's design for encouraging generalization of skills learned in the training sessions. Generalization also requires measures that are sensitive to use of skills in everyday, community life. The Independent Living Skills Survey is one of the few instruments that has been validated as being sensitive to skills used in everyday life. The reality of the steep gradient that patients with schizophrenia must climb to attain or even approximate normal social roles and tasks is not widely appreciated or researched. Thus, the present study offers new insights into assessment technology for social functioning (e.g., Independent Living Skills Survey), as well as determining the efficacy of social skills training through use of a randomized, controlled design.
For this cohort of treatment-refractory, persistently psychotic individuals, major improvements in psychopathology (e.g., BPRS) were not expected, and none was observed except for the agitation subscale, which may have reflected the positive involvement of subjects in the supportive milieus of both treatment conditions, as well as adjustments and fine tuning of their medication after entry into the study by the experienced psychiatrists who served as pharmacotherapists for individuals in both conditions.
As was initially hypothesized, when both between- and within-treatment condition comparisons were conducted, patients in the social skills training condition showed more statistically significant improvements than patients in the occupational therapy condition. Even greater differences between the groups may have been mitigated by the intensive, assertive outreach form of case management that was offered to patients in both psychosocial treatment conditions from their sixth to 24th month of participation in the study.
While the case managers were not blind to the psychosocial treatment conditions, their previous training and experience were more similar to the occupational therapy intervention than social skills training. This clinical background of the case managers, as well as their close supervision by the treating psychiatrists who were blind to psychosocial treatment condition, makes it unlikely that bias entered into their interactions with their assigned patients. In addition, the case managers were all clinicians who were unfamiliar with the research literature and whose major priorities and responsibilities were to sustain and improve the community functioning of their caseload, regardless of psychosocial treatment assignment. Nonetheless, there is the possibility that bias entered into their clinical activities, an occurrence that could not be avoided, given the design of this study. Future efforts to replicate our findings could assign different case managers to the patients who received the different psychosocial treatments; however, this experimental design would also hold the seeds of bias, since no two clinical case managers would be equivalent in personality, rapport, experience, and skill level.
It should be pointed out that the items of the Independent Living Skills Survey are not isomorphic with those in the social skills training curricula. For example, management of personal possessions and money management—two of the survey subscales that showed statistically significant improvement in social skills training subjects when compared with the occupational therapy subjects—were not the focus of any of the formal skills training. Hence, response generalization, as well as stimulus generalization, was noted in the study.
Future directions for social skills training will include integration of assertive case management with the skills training, using in vivo skills training in the community to create even more opportunities, encouragement, and reinforcement for the individual to use enhanced skills and coping abilities in everyday life with natural caregivers. Another evolving innovation is the use of cognitive remediation to improve the basic learning capacities of individuals with schizophrenia (18–20). If intensive neurocognitive training of persons who lack attentional and social perception abilities can be linked to the naturalistic situations in which these abilities must be used, patients might be able to embark on their endeavors in social skills training from a higher plateau and possibly achieve more durable and generalizable results from the training.
APPENDIX 1. Skill Areas for the Four Modules Used to Teach Social and Independent Living Skills to Outpatients With Schizophrenia
1. Medication Management Module
Identifying benefits of antipsychotic medication
Self-administration and evaluation of medication
Serious and mild side effects of antipsychotic medication
Negotiating medication issues with your doctor
Benefits of long-acting, injectable medication
2. Symptom Management Module
Identifying warning signs of relapse
Developing a relapse prevention plan
Coping with persisting psychotic symptoms
Avoiding street drugs and alcohol
3. Recreation for Leisure Module
Identifying benefits of recreational activities
Getting information about recreational activities
Finding out what's needed for a recreational activity
Evaluating and maintaining a recreational activity
4. Basic Conversation Skills Module
Active listening skills
Initiating conversations
Maintaining conversations
Terminating conversations
Putting it all together
 |
 |
 |
Received July 21, 1997; revision received Feb. 3, 1998; accepted March 24, 1998. From the West Los Angeles VA Medical Center and the Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles. Address reprint requests to Dr. Liberman, 528 Lake Sherwood Dr., Thousand Oaks, CA 91361; [email protected] (e-mail). Supported in part by Health Services Research and Development grant 88-093.1 from the Department of Veterans Affairs and by NIMH Clinical Research Center grant MH-30911 (Dr. Liberman). The administrative support of the West Los Angeles VA Medical Center, Community and Rehabilitative Psychiatry Section, is acknowledged. The authors acknowledge the contributions to this research by the therapists—Ethel Kleinschmidt, O.T.R., Surni Kumagai, O.T.R., Sonia Vellani, O.T.R., Ann Powell, O.T.R., Edgar Mitchell, A.A., Bernice Allen, A.A., and Ron Allen, A.A.—and the case managers—Sheila Brooks, M.A., Carol Reimer, M.A., and Mitchell Caine, M.A. Psychiatric services were provided by Greer Sullivan, M.D., George Bartzokis, M.D., and Alex Young, M.D. Statistical analyses were done by Sun Hwang, M.S.
1 Liberman RP, Vaccaro JV, Corrigan PW: Psychiatric rehabilitation, in Comprehensive Textbook of Psychiatry, 6th ed. Edited by Kaplan HI, Sadock BJ. Baltimore, Williams & Wilkins, 1995, pp 2696–2717Google Scholar
2 Penn DL, Mueser KT: Research update on the psychosocial treatment of schizophrenia. Am J Psychiatry 1996; 153:607–617Link, Google Scholar
3 Favrod J, Huguelet P, Chambon O: L'education on traitment neuroleptique pent-elle reduire les couts. L'Encephale 1996; 22:331–336Medline, Google Scholar
4 Liberman RP: International perspectives on skills training. Int Rev Psychiatry 1998; 10:1–9Google Scholar
5 Hogarty GE, Anderson CM, Reiss DJ, Komblith SJ, Greenwald D, Ulrich R, Carter M: Family psychoeducation, social skills training, and maintenance chemotherapy in the aftercare treatment of schizophrenia. Arch Gen Psychiatry 1991; 48:340–347Crossref, Medline, Google Scholar
6 Benton MK, Schroeder HE: Social skills training with schizophrenics: a meta-analytic evaluation. J Consult Clin Psychol 1990; 58:741–747Crossref, Medline, Google Scholar
7 Dilk MN, Bond GR: Meta-analytic evaluation of skills training research for individuals with severe mental illness. J Consult Clin Psychol 1996; 64:1337–1346Crossref, Medline, Google Scholar
8 Liberman RP, Wallace CJ, Blackwell GA, Eckman TA, Vaccaro JV, Kuehnel TG: Innovations in skills training for the seriously mentally ill: the UCLA Social and Independent Living Skills Modules. Innovations & Research 1993; 2:43–59Google Scholar
9 Allen CK: Occupational therapy: functional assessment of the severity of mental disorders. Hosp Community Psychiatry 1988; 39:140–142Abstract, Google Scholar
10 Ventura J, Green MF, Shaner A, Liberman RP: Training and quality assurance in the use of the Expanded Brief Psychiatric Rating Scale: the “drift busters.” Int J Methods Psychiatr Res 1993; 3:221–244Google Scholar
11 Green BL, Wehling C, Talsky GJ: Group art therapy as an adjunct to treatment for chronic outpatients. Hosp Community Psychiatry 1987; 38:988–991Abstract, Google Scholar
12 Liberman RP, Corrigan PW: Designing new psychosocial treatments for schizophrenia. Psychiatry 1993; 56:238–248Medline, Google Scholar
13 Hromco JG, Lyons JS, Nikkel RE: Styles of case management: the philosophy and practice of case managers. Community Ment Health J 1997; 33:415–428Crossref, Medline, Google Scholar
14 Mechanic D: Emerging issues in international mental health services. Psychiatr Serv 1996; 47:371–375Link, Google Scholar
15 Wallace CJ: Functional assessment in rehabilitation. Schizophr Bull 1986; 12:604–630Crossref, Medline, Google Scholar
16 Marder SR, Wirshing WC, Mintz J, McKenzie J, Johnston K, Eckman TA, Lebell M, Zimmerman K, Liberman RP: Two-year outcome for social skills training and group psychotherapy for outpatients with schizophrenia. Am J Psychiatry 1996; 153:1585–1592Link, Google Scholar
17 Liberman RP, Wallace CJ: Social skills training for schizophrenics: a controlled clinical trial. Psychiatry Res 1985; 15:239–247Crossref, Medline, Google Scholar
18 Green MF: What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 1996; 153:321–330Google Scholar
19 Green MF: Cognitive remediation in schizophrenia: is it time yet? Am J Psychiatry 1993; 150:178–187Google Scholar
20 Kern RS, Green MF, Goldstein MJ: Modification of performance on the Span of Apprehension, a putative marker of vulnerability to schizophrenia. J Abnorm Psychol 1995; 104:385–389Crossref, Medline, Google Scholar



