Clinical Relevance of the Distinction Between Alcohol Dependence With and Without a Physiological Component
Abstract
OBJECTIVE: DSM-IV indicates that diagnoses of substance dependence should be further characterized with regard to the presence of a physiological component, defined by tolerance or withdrawal. This study evaluated the possible meaning of this distinction in alcohol-dependent men and women. METHOD: As part of the Collaborative Study on the Genetics of Alcoholism, structured interviews were carried out with 3,395 DSM-III-R-defined alcohol-dependent individuals divided into 2,949 subjects (86.9%) with evidence of tolerance and/or withdrawal (group 1), 51.3% of whom evidenced withdrawal symptoms, and 446 subjects (13.1%) without a physiological component (group 2). Data were evaluated to determine differences between the two groups. RESULTS: Group 1 reported greater severity of alcohol dependence as demonstrated by a larger maximum number of drinks in 24 hours, more persons reporting binges, more alcohol-related life problems, more relevant DSM-III-R criteria endorsed, more physiological complications, and more alcohol-related emotional/psychiatric symptoms such as depression and anxiety. Each of these severity indicators for problems in group 1 was significant in the presence of the others in a logistic regression, and similar items remained significant when tolerance alone, withdrawal alone, or their combination was used as the criterion for group 1 membership; however, for withdrawal a larger proportion of the variance was explained by the predictor variables. The regression results were independent of gender, proband status, and history of antisocial personality disorder. CONCLUSIONS: The results support the clinical relevance of distinguishing between alcohol-dependent patients with and without a physiological component. The data indicate a potential advantage to limiting that definition to withdrawal only.
Between 1700 and the present, about 50 potential typologies and subgroupings for alcohol and drug problems were proposed (1–6). Most of these rubrics, but not all, incorporated aspects of physiological components of substance-related syndromes, such as tolerance and withdrawal, as criterion items. In the recent decade there has been greater agreement in defining severe substance-related syndromes, with a compromise regarding the importance of physiological aspects of withdrawal that grew out of the broad concept of dependence developed by Edwards and Gross (ICD-10, 7, 8). In order to describe a complex, multifaceted process that applies across substances, tolerance and withdrawal became part of the substance use disorder spectrum but were no longer viewed as required elements. This reflects the belief that devastating levels of problems can develop with use of some drugs without tolerance or withdrawal and the recognition that there were insufficient data documenting that the physiological conditions were of greater importance than other aspects of “dependence” (9–11).
At the same time, there might not be sufficient data to justify this lessened emphasis on tolerance and withdrawal (7, 12, 13). Consideration of the physiological components of substance dependence could, at least theoretically, help clinicians avoid classifying mild cases as dependent, enhance the distinction between drugs with higher and lower abuse liabilities, identify individuals most in need of immediate medical treatment, and help justify the costs of more intensive care (9). Additional potential benefits include the recognition of the potential reinforcing role of continued substance use to relieve withdrawal symptoms and the importance of physiological symptoms as markers of a greater probability of relapse (9, 14, 15). Finally, the emphasis on tolerance and withdrawal can also serve as a framework for the concept that dependence might relate to biological mechanisms and might have important implications for genetic research (16–18).
Reflecting these issues, the framers of DSM-IV requested that clinicians and researchers gather more data by subtyping substance dependence as having developed with or without accompanying tolerance or withdrawal. To date, several attempts have been made to comply with this request by using cross-sectional comparisons. Regarding alcohol, a study of 344 subjects with at least one alcohol problem from among 521 patients from a variety of treatment settings (9) found no convincing evidence that tolerance and withdrawal were related to a greater number of DSM-IV dependence problems. Similar conclusions were generated for cocaine, opiates, amphetamines, sedative-hypnotics, and cannabinols. For no substance was tolerance or withdrawal linked to exceptionally high scores on the Addiction Severity Index. Another study of 399 cocaine-using subjects (10) found low to modest Sommer's D relationships between withdrawal or tolerance and Addiction Severity Index ratings of social problems (correlation=0.26), employment difficulties (correlation=0.21), associated drug or psychiatric problems (correlation=0.17), and alcohol use (correlation=0.20). Overall, there is little consistent support for a relationship between more severe concurrent problems and tolerance/withdrawal of opiates, sedatives, and canna~binols (9).
Several investigators have evaluated the potential relevance of tolerance and/or withdrawal to short-term clinical outcome in longitudinal studies. Regarding cocaine, with use of Sommer's D statistic, a 1-year follow-up of 94 (63%) of 150 cocaine-using subjects (10) found that tolerance and/or withdrawal at treatment intake had a correlation as high as 0.42 with Addiction Severity Index psychiatric symptoms during follow-up and as high as 0.27 with Addiction Severity Index scores on social functioning. Other correlations were as high as 0.20 with employment during the follow-up period, 0.17 with alcohol or drug use, and 0.14 with legal problems, although for these last three results, other DSM-IV items were related to Addiction Severity Index items at as high or higher levels. Another follow-up showed little evidence of any close relationship between physiological dependence at intake and outcomes for subjects with problems with a variety of drugs (10). Thus, there are few data which argue convincingly that physiological components of dependence effectively predict outcome in persons with substance-related problems (9, 10, 19).
In summary, while few studies have evaluated the centrality of diagnostic items that indicate physiological dependence, the proportions of substance-dependent individuals who exhibit tolerance and/or withdrawal symptoms differ markedly across different drugs and treatment settings (10, 12, 20–22). In addition, these physiological symptoms have long been emphasized by clinicians, indicating that further study regarding their diagnostic importance is needed. This article evaluates concurrent clinical validators or correlates of alcohol dependence with and without a physiological component in a large, diverse, and intensely studied population.
METHOD
The six-center-wide Collaborative Study on the Genetics of Alcoholism is a large family investigation designed to identify genetic factors in alcohol use, abuse, and dependence (20, 23–25). After a full explanation of the procedures, appropriate subjects in these centers gave written informed consent to participate. The subjects were consecutive alcohol-dependent individuals who entered selected alcohol and drug treatment programs and who met both the DSM-III-R criteria and the Feighner definite criteria (26) for alcohol dependence and alcoholism. They were included regardless of additional diagnoses; the only exclusions occurred for persons who were unable to speak English, those with evidence of severe debilitating diseases such as AIDS, those with histories of intense intravenous drug use, and those who had fewer than five relatives available for interview.
Evaluations were carried out with use of the Semi-Structured Assessment for the Genetics of Alcoholism interview (20, 23) by highly trained personnel who screened for 17 axis I diagnoses as well as antisocial personality disorder. Interviewers received intensive training on the Semi-Structured Assessment for the Genetics of Alcoholism, all completed interviews were reviewed by senior editors, and clinicians reviewed all data when diagnostic information was unclear. In addition to interviews with the probands (initial index cases), identical structured interviews were carried out with all available biological relatives, and data were evaluated in a manner similar to that used for the probands.
The section on alcohol of the Semi-Structured Assessment for the Genetics of Alcoholism is quite detailed. Subjects are queried regarding recent drinking history, patterns of alcohol use, periods of abstinence, and an extensive series of life experiences related to alcohol. Included among these are items relevant to establishing diagnoses of alcohol dependence, abuse, or harmful use as evidenced by the diagnostic criteria proposed by Feighner et al. (26), the Research Diagnostic Criteria (27), DSM-III-R, DSM-IV, and ICD-10. Similar data related to multiple diagnostic schemes are gathered regarding dependence on most drugs of abuse and for major psychiatric disorders, including most of the major anxiety and mood disorders.
Data were also gathered from comparison subjects at each of the six centers. These individuals were identified through a variety of mechanisms, including random selection from drivers' license records, advertisements, random selection of individuals attending medical or dental clinics, and respondents to a questionnaire mailed to randomly selected subjects at a university campus (20, 24, 25).
The present analyses compared DSM-III-R-defined alcohol-dependent individuals who reported histories indicating the presence or absence of a physiological component. All data came from face-to-face interviews in which the Semi-Structured Assessment for the Genetics of Alcoholism was used; the 3,395 subjects included 1,180 probands (34.8%), 2,054 DSM-III-R-defined alcohol-dependent relatives of the probands (60.5%), and 161 alcohol-dependent comparison subjects or relatives of comparison subjects (4.7%). To test the procedures suggested by DSM-IV, the alcohol-dependent subjects were placed into two major groups on the basis of endorsement in the semistructured interview of one or more of the following items as being appropriate for them at sometime during the course of their alcohol dependence. Consistent with the guidelines set forth in DSM-IV, evidence for selection for group 1, indicating the presence of a physiological component, included 1) having developed tolerance (i.e., at any time in one's life, needing to consume at least 50% more alcohol than usual to get the same effect), 2) having developed an alcohol withdrawal syndrome at some time during one's alcoholic career (e.g., reporting two or more of the symptoms listed in DSM-III-R for alcohol withdrawal, with one of these being “shakes”), and 3) ever using a substance to avoid or relieve withdrawal symptoms. Group 2 included those individuals who met the DSM-III-R criteria for alcohol dependence but without evidence of tolerance, of having experienced an alcohol withdrawal syndrome, or of having used a substance to avoid withdrawal symptoms. Analyses that required a distinction between substance-induced and independent psychiatric conditions used the time-line approach described in more detail elsewhere (24, 25, 28, 29).
The chi-square test (with Yates's correction where appropriate) was used to test for differences between groups in categorical data, and Student's t test was used for comparison of means across groups. Because of the large number of subjects involved in the analyses, with the possibility that relatively trivial group differences would appear to be statistically significant, data were also examined regarding the magnitude of effect (small, medium, or large) of the statistical differences according to the method of Cohen (30) (the d statistic for Student's t test and the w statistic for the chi-square test). Finally, a logistic regression analysis was used to determine the potential relevance of the most prominent factors that differentiated the groups with and without physiological dependence, offering the opportunity to evaluate the effect of each predictor while controlling for the impact of other factors.
RESULTS
Group 1 contained 2,949 subjects (86.9%) with evidence of tolerance and/or aspects of withdrawal at some time during their alcoholic course, while group 2 contained 446 subjects (13.1%) with no evidence of a physiological component in the course of their alcoholism. In group 1 almost half (48.7%) of the subjects reported tolerance alone, 3.8% reported at least one of the two indicators of withdrawal or withdrawal relief in the absence of tolerance, and 47.5% noted a history of alcohol-related tolerance and at least one of the two aspects of withdrawal.
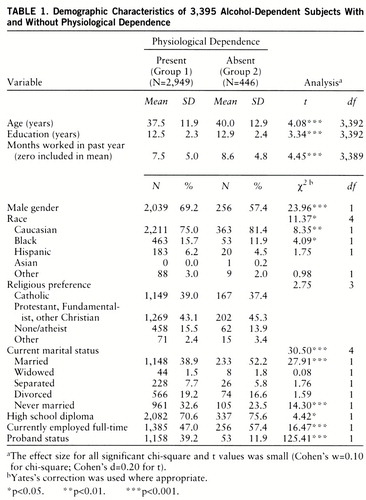
Table 1 presents the demographic characteristics of the two groups. Significant differences (all at the level of small effect sizes) included a higher proportion of male subjects and a lower proportion of subjects who were currently or ever married in group 1 (those with physiological dependence). Subjects in that group were also somewhat younger, less educated, less likely to be employed, less likely to be Caucasian, and more likely to be probands (initial index cases).
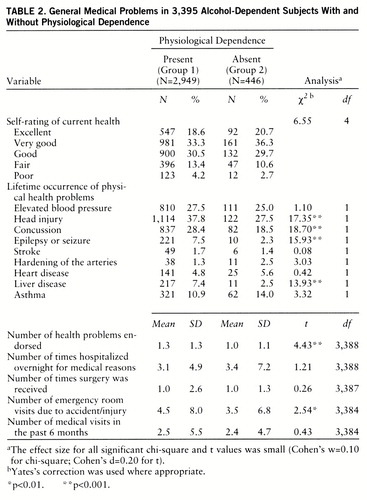
Table 2 shows data on whether ever having met criteria for physiological dependence was associated with a history of more general (i.e., not alcohol-related) medical problems in the two groups. Subjects in group 1 were more likely to report histories of head trauma, concussion, seizure disorder, and any type of liver disease. Recognizing that individual disorders in this panoply of physical disorders are not likely to be independent, we compared a single overall measure of the number of the nine medical items endorsed in group 1 and group 2. A small but significantly greater number of general physical health problems was found among the subjects with physiological dependence. Consistent with the increased risk of medical disorders, individuals in group 1 had more emergency room visits. However, the two groups did not differ in lifetime number of hospitalizations, number of surgeries, or prior 6-month history of medical visits.
Table 3 shows the relation between group membership and intensity of alcohol use and alcohol problem histories. Regarding the pattern of alcohol intake, subjects with physiological dependence demonstrated a 50% higher maximum number of drinks in 24 hours. Group 1 subjects also showed an earlier age at onset of regular drinking and of first intoxication and reported fewer periods of abstinence lasting 3 or more months since the onset of regular drinking. The prevalence of 26 of the more frequently observed major life events associated with alcohol use in this population was also examined. Group 1 subjects were significantly more likely to have reported 23 of these events, and the average number of the 26 categories they endorsed was almost twice as high as the number in group 2. For the six DSM-III-R dependence items not used in group assignment (i.e., excluding criteria related to tolerance or withdrawal), the average number of those items endorsed by group 1 subjects was also significantly higher than for group 2. Finally, the proportion of probands' interviewed first-degree relatives who were alcohol-dependent was significantly higher for group 1 subjects (45.2%, N=1,309 of 2,893) than for group 2 subjects (24.3%, N=37 of 152) (χ2=14.61, df=1, p<0.001, Cohen's d=0.20 [small effect size]). Relatives of probands were used to avoid counting an individual more than once if he or she was related to multiple subjects in this family study, and only personally interviewed relatives were evaluated to optimize the quality of the information used.
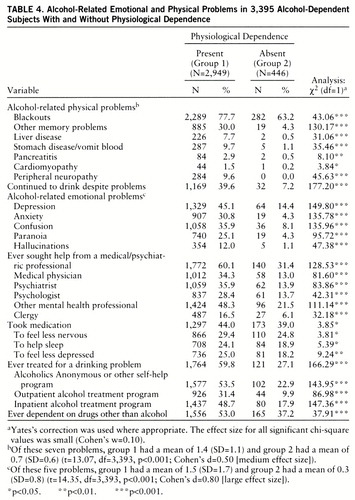
Table 4 shows self-reported alcohol-related physical and emotional problems among the subjects in group 1 and group 2. Group 1 subjects reported higher frequencies of each of the physiological difficulties associated with alcohol use and a higher mean number of the seven items endorsed. The evaluation of psychological problems reported to have occurred during periods of heavy drinking yielded similar conclusions. Consistent with evidence of greater levels of alcohol-related medical and psychological impairment, a higher proportion of group 1 subjects had sought help from professionals, had taken psychiatric medications, and had attended self-help groups or more structured treatment programs for alcohol difficulties. Related to these general data is the higher lifetime prevalence of dependence on one or more drugs other than alcohol for individuals in group 1.
The higher prevalence of alcohol-related (or alcohol-induced) psychiatric symptoms raises the possibility that group 1 members might also evidence a higher rate of axis I major psychiatric disorders or of antisocial personality disorder than group 2 subjects. Table 5 displays the rates of independent psychiatric disorders in the two groups, showing that while the lifetime histories of each major axis I diagnosis were similar for the subjects with and without physiological dependence, group 1 had a significantly higher rate of antisocial personality disorder. The rates of two psychiatric syndromes observed only in the context of substance dependence (induced disorders) were significantly higher in group 1: major depressive disorder and antisocial personality disorder. The latter finding indicates subjects who only met antisocial personality disorder criteria when life events that occurred solely in the context of heavy alcohol use were also counted.
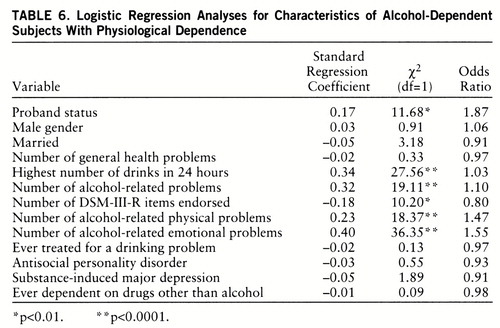
While tables 1–5 demonstrate that a history of physiological dependence on alcohol is associated with several demographic, general medical, alcohol use, alcohol problem, and comorbid psychiatric pictures, the data to this point do not allow an evaluation of the importance of characteristics from each domain if considered in the context of the others. Therefore, we carried out a logistic regression analysis, using characteristics from each domain that were significantly different between groups 1 and 2 and that we felt, a priori, summarized the key findings in a table or were potentially clinically relevant. Items only available for a subset of subjects (e.g., proportion of interviewed relatives of probands who were alcohol-dependent) were not included, nor were items felt to demonstrate small, even though statistically significant, differences. As shown in table 6, the specific items entered into the logistic regression to predict group 1 membership (physiological dependence) included whether the subject was a proband, demographic factors (male gender and currently being married), health problems (number of lifetime general health problems endorsed), and the maximum number of drinks ever consumed in 24 hours. Five additional items relating to the course of alcoholism were also incorporated, including the number of the 26 possible general alcohol-related life problems endorsed, the number out of the six remaining DSM-III-R dependence items that occurred, the number of alcohol-related physical problems, the number of emotion~al problems, and a history of seeking help for alcohol dependence. The final three items entered into the logistic regression were a lifetime history of an independent diagnosis of antisocial personality disorder, ever being dependent on another drug, and a history of a substance-induced major depressive episode.
The regression analysis revealed that six of the 13 predictor items contributed significantly, with the results explaining 17.1% of the variance (the pseudo R2) in group membership. The six predictors included a measure of higher levels of intensity of drinking, all of the measures of alcohol-related life problems, and proband status. The logistic regression analysis revealed that the demographic items, the meas~ure of general health problems, a history of inpatient treatment for alcoholism, and other diagnostic items did not contribute to the prediction of physiological dependence when evaluated in the context of the other items. In this regression analysis, findings for all items were in the predicted direction except for the number of DSM-III-R items endorsed, in which case the sign reflected the impact of a suppressor variable.
Several additional analyses were carried out to evaluate further the applicability of the logistic regression findings to potentially important subgroups. Not surprisingly, when a logistic regression was carried out separately for men and women, similar items predicted physiological dependence in the same direction. The predictors functioned similarly for subjects with and without antisocial personality disorder, and similar results were observed for probands (index cases) and nonindex family members. The ability of the logistic regression analysis to predict group membership among nonindex cases might indicate that the results are relevant to persons who met criteria for alcohol dependence but were not as severely incapacitated as the original probands. The applicability of the results to probands (a sample of unrelated subjects) indicates that the findings are not merely a reflection of having studied genetically related individuals.
The major aim of this study was to evaluate the potential clinical relevance of the DSM-IV distinction between the presence and absence of physiological dependence defined as evidence of tolerance and/or withdrawal. However, as noted earlier, the two phenomena of tolerance and withdrawal might not represent a unitary concept (15, 16). Therefore, the logistic regression was carried out separately for the 1,434 group 1 subjects who evidenced tolerance alone, and then for the 1,515 who reported withdrawal or use of substances to relieve or avoid withdrawal symptoms. Regarding tolerance alone, exactly the same items as those in table 6 significantly predicted group 1 membership. However, the results, while significant, explained only 5.4% of the variance. A separate logistic regression with group 1 defined as showing evidence of withdrawal also revealed items similar to those in table 6, with the exception that a history of treatment for alcoholism became significant, while the number of DSM-III-R items endorsed was not. Here, however, the results explained 52.3% of the variance.
DISCUSSION
This study tested the potential clinical relevance of the DSM-IV approach of subtyping individuals with dependence into subgroups with and without histories of tolerance and/or withdrawal. The data consistently indicate that the physiological characteristics of dependence denote a group with a more severe course of alcoholism, a conclusion that might be especially relevant to subjects with histories of withdrawal.
There are several levels of support for the clinical relevance of the continued distinction between alcohol-dependent individuals with and without a physiological component. First, over 13% of the subjects denied having ever met criteria for physiological dependence, and 48.7% gave no history of withdrawal symptoms. This suggests that the physiological distinction might identify a subgroup of a size that is clinically relevant. Second, the demographic similarity between groups in the logistic regression indicates the possibility that the clinical distinction based on physiological symptoms might have a broad clinical application.
Alcohol-dependent subjects who reported a physiological component demonstrated more alcohol-related problems and more intense alcohol use than subjects without a physiological component. They had higher levels of alcohol intake, noted twice the number of alcohol-related physiological complications, and had five times the rate of alcohol-induced emotional or psychiatric symptoms. These indicators of severity were independent of gender and antisocial personality disorder status and appeared applicable to both index and nonindex cases. These results are consistent with a report by Bucholz et al. (31), who interpreted the data from a latent class analysis as indicating that alcohol dependence is distributed on a spectrum of severity, with physiological dependence representing a relatively distinct group of persons at the more severe extreme.
The group differences reported here are of a greater magnitude than might have been expected from the rather scant available literature. Several studies have reported little evidence of greater severity for alcoholic subjects with tolerance and/or withdrawal, but those subjects were originally chosen because of their involvement with cocaine, not alcohol (9, 10). In addition, the present study used the Semi-Structured Assessment for the Genetics of Alcoholism, a more detailed and intensive evaluation of the alcoholic course than the Addiction Severity Index. The present work also provided a separate evaluation of lifetime general medical problems (which did not differentiate groups 1 and 2 in the regression analysis) versus specific alcohol-related psychiatric or physical problems (which did distinguish between groups). The other studies (9, 10) also reported little evidence that physiological dependence was related to severity of cocaine dependence, although several of the Addiction Severity Index scales indicated that at least some level of enhanced severity might be associated with the diagnostic distinction. In those studies, follow-up of a subset of 94 subjects revealed that the correlation between Addiction Severity Index score for psychiatric symptoms and evidence of physiological dependence was 0.42. These prior generally negative results indicate the need for further study of individuals dependent on drugs other than alcohol, analyses that will be the focus of another paper.
The present data also indicate that more research is needed regarding the definition of physiological dependence. While similar items were associated with group 1 membership when tolerance alone, dependence alone, or their combination was used, the items explained the highest proportion of the variance when withdrawal was the criterion. This might indicate that the most severe clinical course and, thus, the most relevant clinical definition of a physiological component of dependence rests with a definition that includes evidence of withdrawal.
Our results must be considered in the context of the methods used. First, the data test the DSM-IV distinction, and additional analyses will be needed to see whether any other combination of DSM items better identifies a subgroup with a more severe course. Second, the present analyses are cross-sectional and offer no information regarding the implications of tolerance and withdrawal for the future clinical course among alcohol-dependent individuals. However, the Collaborative Study on the Genetics of Alcoholism investigation has recently initiated a 3- to 5-year follow-up of subjects that should help address this issue more directly in the future. The third caveat is the need to recognize relatively unique aspects of the Collaborative Study on the Genetics of Alcoholism sample, including the high frequency of alcohol dependence observed in the probands' families and the procedures used to select convenient comparison subjects and families across the six sites. However, in the present sample, the apparent relationship between group 1 membership and evidence of a more severe alcoholic course appears to be true for both men and women, for index versus nonindex cases, and for individuals with and without antisocial personality disorder, indicating a probability that the findings are generalizable to other clinical and nonclinical samples. An additional methodological consideration is the a priori approach we used to select the items for comparing group 1 and group 2 subjects. However, the items were chosen to have clinical relevance, and the results are internally consistent. Finally, while the logistic regression explained 17.1% of the variance, that figure indicates that many other factors are related to the diagnostic distinction, and there is still a great deal to be learned.
In conclusion, one potentially important attribute of a diagnostic distinction is its ability to identify a population with a relatively unique clinical course (32). Thus, the present findings provide evidence supporting the designation of alcohol dependence with and without a physiological component. Physiological dependence appears to indicate greater levels of involvement with alcohol and more associated problems, supporting the contention that this distinction proposed by DSM-IV might have clinical validity and deserves further study.
ACKNOWLEDGMENTS
The Collaborative Study on the Genetics of Alcoholism (H. Begleiter, State University of New York, Health Sciences Center at Brooklyn, principal investigator, and T. Reich, Washington University, co-principal investigator) includes six different centers where data collection takes place. The six sites and principal investigators and co-investigators are Indiana University (J. Nurnberger, Jr., T.-K. Li, P.M. Conneally, H. Edenberg); University of Iowa (R. Crowe, S. Kuperman); University of California at San Diego and Scripps Institute (M. Schuckit, F. Bloom); University of Connecticut (V. Hesselbrock); State University of New York, Health Sciences Center at Brooklyn (H. Begleiter, B. Porjesz); and Washington University, St. Louis (T. Reich, C.R. Cloninger, J. Rice).
 |
 |
 |
 |
 |
 |
Received July 24, 1997; revision received Nov. 3, 1997; accepted Dec. 4, 1997. From the Collaborative Study on the Genetics of Alcoholism. Address reprint requests to Dr. Schuckit, Department of Psychiatry (116A), VA Medical Center, 3350 La Jolla Village Dr., San Diego, CA 92161-2002. Supported by National Institute on Alcohol Abuse and Alcoholism grants AA-08401, AA-08402, AA-08403, and AA-05526 and by the Veterans Affairs Research Service.
1 Schuckit MA: DSM-IV: was it worth all the fuss? Alcohol Alcohol Suppl 1994; 2:459–469Google Scholar
2 Babor TF, Lauerman RJ: Classification and forms of inebriety, in Recent Developments in Alcoholism, vol 4. Edited by Galanter M. New York, Plenum, 1986, pp 113–144Google Scholar
3 Caetano R: When will we have a standard concept of alcohol dependence? Br J Addict 1987; 82:601–605Google Scholar
4 Babor TF, Dolinsky ZS: Alcohol typologies: historical evolution and empirical evaluation of some common classification schemes, in Alcoholism: Origins and Outcome. Edited by Rose RM, Barrett J. New York, Raven Press, 1988, pp 245–266Google Scholar
5 Babor TF: Substance-related problems in the context of international classificatory systems, in The Nature of Alcohol and Drug-Related Problems. Edited by Lader M, Edwards G, Drummond C. Oxford, England, Oxford University Press, 1992, pp 83–97Google Scholar
6 Jellinek EM: The Disease Concept of Alcoholism. New Brunswick, NJ, Hillhouse, 1960Google Scholar
7 Schuckit MA: Substance-related disorders, in DSM-IV Sourcebook, vol 1. Edited by Widiger TA, Frances AJ, Pincus HA, First MB, Ross R, Davis W. Washington, DC, American Psychiatric Association, 1994, pp 5–19Google Scholar
8 Edwards G, Gross MM: Alcohol dependence: provisional description of a clinical syndrome. BMJ 1976; 1:1058–1061Crossref, Medline, Google Scholar
9 Carroll KM, Rounsaville BJ, Bryant KJ: Should tolerance and withdrawal be required for substance dependence disorders? Drug Alcohol Depend 1994; 36:15–22Google Scholar
10 Rounsaville BJ, Bryant K: Tolerance and withdrawal in the DSM-III-R diagnosis of substance dependence: utility in a cocaine-using population. Am J Addict 1992; 1:50–60Google Scholar
11 Cottler LB, Helzer JE, Mager D, Spitznagel EL, Compton WM: Agreement between DSM-III and III-R substance use disorders. Drug Alcohol Depend 1991; 29:17–25Crossref, Medline, Google Scholar
12 Cottler LB, Schuckit MA, Helzer JE, Crowley T, Woody G, Nathan P, Hughes J: The DSM-IV field trial for substance use disorders: major results. Drug Alcohol Depend 1995; 38:59–69Crossref, Medline, Google Scholar
13 Nathan PE: Psychoactive substance dependence, in DSM-IV Sourcebook, vol 1. Edited by Widiger TA, Frances AJ, Pincus HA, First MB, Ross R, Davis W. Washington, DC, American Psychiatric Press, 1994, pp 33–43Google Scholar
14 Skinner HA: Alcohol dependence: how does it come about? Br J Addict 1986; 81:279–284Google Scholar
15 Kalant H: Nathan B Eddy memorial award lecture: tolerance and its significance for drug and alcohol dependence. NIDA Res Monogr 1987; 76:9–19Medline, Google Scholar
16 Tabakoff B: One man's craving is another man's dependence. Br J Addict 1990; 85:1253–1254Crossref, Medline, Google Scholar
17 Edwards G: Withdrawal symptoms and alcohol dependence: fruitful mysteries. Br J Addict 1990; 85:447–461Crossref, Medline, Google Scholar
18 Cicero TJ: Alcohol self-administration, tolerance and withdrawal in humans and animals: theoretical and methodological issues, in Alcohol Tolerance and Dependence, vol 1. Edited by Rigter H, Rabbe JCC. New York, Elsevier, 1980Google Scholar
19 Langenbucher J, Chung T, Morgenstern J, Labouvie E, Nathan PE, Bavly L: Physiological alcohol dependence as a “specifier” of risk for medical problems and relapse liability in DSM-IV. J Stud Alcohol 1997; 58:341–350Crossref, Medline, Google Scholar
20 Schuckit MA, Daeppen J-B, Tipp JE, Hesselbrock M, Bucholz KK: The clinical course of alcohol-related problems in alcohol dependent and nonalcohol dependent drinking women and men. J Stud Alcohol (in press)Google Scholar
21 Edwards G: The alcohol dependence syndrome: a concept as stimulus to enquiry. Br J Addict 1986; 81:171–183Crossref, Medline, Google Scholar
22 Schuckit MA, Anthenelli RM, Bucholz KK, Hesselbrock VM, Tipp J: The time course of alcohol-related problems in men and women. J Stud Alcohol 1995; 56:218–225Crossref, Medline, Google Scholar
23 Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI Jr, Reich T, Schmidt I, Schuckit MA: A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol 1994; 55:149–158Crossref, Medline, Google Scholar
24 Schuckit MA, Tipp JE, Bergman M, Reich W, Hesselbrock VM, Smith TL: Comparison of induced and independent major depressive disorders in 2,945 alcoholics. Am J Psychiatry 1997; 154:948–957Link, Google Scholar
25 Schuckit MA, Tipp JE, Bucholz KK, Nurnberger JI Jr, Hesselbrock VM, Crowe RR, Kramer J: The life-time rates of three major mood disorders and four major anxiety disorders in alcoholics and controls. Addiction 1997; 92:1289–1304Crossref, Medline, Google Scholar
26 Feighner JP, Robins E, Guze SB, Woodruff RA Jr, Winokur G, Munoz R: Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry 1972; 26:57–63Crossref, Medline, Google Scholar
27 Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria: rationale and reliability. Arch Gen Psychiatry 1978; 35:773–782Crossref, Medline, Google Scholar
28 Schuckit MA, Tipp JE, Anthenelli RM, Bucholz KK, Hesselbrock VM, Nurnberger JI Jr: Anorexia nervosa and bulimia nervosa in alcohol-dependent men and women and their relatives. Am J Psychiatry 1996; 153:74–82Link, Google Scholar
29 Schuckit MA, Hesselbrock VM, Tipp J, Nurnberger JI, Anthen~elli RM, Crowe RR: The prevalence of major anxiety disorders in relatives of alcohol dependent men and women. J Stud Alcohol 1995; 56:309–317Crossref, Medline, Google Scholar
30 Cohen J: Statistical Power Analyses for the Behavioral Sciences, 2nd ed. Hillsdale, NJ, Lawrence Erlbaum Associates, 1988Google Scholar
31 Bucholz KK, Heath AC, Reich T, Hesselbrock VM, Kramer JR, Nurnberger JI Jr, Schuckit MA: Can we subtype alcoholism? a latent class analysis of data from relatives of alcoholics in a multicenter family study of alcoholism. Alcohol Clin Exp Res 1996; 20:1462–1471Crossref, Medline, Google Scholar
32 Goodwin DW, Guze SB: Psychiatric Diagnosis, 5th ed. New York, Oxford University Press, 1996Google Scholar



