Prevalence and Characteristics of Trauma and Posttraumatic Stress Disorder in a Southwestern American Indian Community
Abstract
OBJECTIVE: High rates of violence and trauma in many American Indian communities have been reported. The authors investigated the relationship between both the frequency and type of traumatic events and the prevalence of posttraumatic stress disorder (PTSD) in a Southwestern American Indian tribe. METHOD: A structured psychiatric interview and the Traumatic Events Booklet were administered to a subset of 247 tribal members from an overall study population of 582. Subjects were recruited from the community on the basis of membership in pedigrees, and not by convenience. DSM-III-R diagnoses were assigned by consensus after the interviews were evaluated blindly by independent raters. RESULTS: The prevalence of lifetime PTSD was 21.9% (N=54), and 81.4% of the subjects (N=201) had experienced at least one traumatic event apiece. The most predictive factor for lifetime PTSD among women was the experience of physical assault, and for men the most predictive factors were a history of combat and having experienced more than 10 traumatic events. CONCLUSIONS: In this Southwestern American Indian community, the prevalences of lifetime PTSD and of exposure to a traumatic event were higher than in the general U.S. population. However, the nearly 4:1 ratio of subjects who reported at least one traumatic event to those with PTSD diagnoses is similar to findings from studies of non-Indians. Individuals with a history of multiple traumatic events (66.0%, N=163) had a significantly higher risk of developing PTSD. Chronic and multiple trauma did not preclude the identification of acute and discrete traumatic events that resulted in PTSD. (Am J Psychiatry 1997; 154:1582–1588)
American Indians are at high risk for early death, exposure to violence, and other traumatic events. The homicide rate is 70% higher for American Indians than for Caucasians in the U.S. population (1). The suicide rate for American Indians is two to four times as high as that for non-Indian populations (2). Early death is more common among American Indians than among other ethnic groups, and many of the leading causes of death are “lifestyle-related” diseases and events, such as suicide, accidents, and alcoholism (3). Despite these high exposure rates, nearly all data on violence and trauma among American Indians have been compiled from mortality and morbidity statistics. Little is known about the effects of nonfatal traumatic events on the lives of American Indians (4).
Information on traumatic events in the U.S. non-Indian civilian population is abundant. National surveys indicate that exposure to violence and attendant trauma is common. An estimated 36%–70% of people have experienced at least one traumatic event apiece in their lifetimes (5, 6). Posttraumatic stress disorder (PTSD), one organized response to trauma, occurs in almost one-fourth of those exposed to traumatic events (7). To more fully evaluate the impact of violence on American Indians, both trauma exposure and subsequent responses, including PTSD, need to be examined.
This current study, part of a larger investigation of alcoholism and psychiatric disorders, evaluated the relationship between traumatic life events and PTSD in a Southwestern American Indian tribal community. PTSD was also examined in terms of its relationship to trauma exposure. High rates of trauma exposure increased our ability to relate PTSD to trauma and other factors in this tribal community. The community is geographically situated in a state where American Indians have much higher rates of death from homicide, accidents, and suicide than do other ethnic groups (8; analysis of 1992–1994 death records conducted by J.K. Rasmussen, 1996). Furthermore, lifestyle-related diseases have been identified by the tribe as among its top 10 health concerns (9). Finally, high rates of alcoholism, drug use disorders, and child sexual abuse, all indices of trauma, have been reported for this tribe (10, 11). We hypothesized that given the likely high rate of exposure to multiple and severe traumatic events in this community, its members would correspondingly exhibit high rates of PTSD.
METHOD
Subjects
The total study group comprised 582 adult subjects in a study of genetic and environmental factors in vulnerability to alcoholism in three large and interrelated multigenerational pedigrees. We used the genealogical information to address the extent to which this family-derived study group is genetically representative of the tribe. The links between the three large pedigrees were identified, and the fraction of genes shared by common descent was calculated for all 169,071 pairs of the 582 participants. A randomly drawn pair of individuals shared only 1.2% of their genes by descent, equivalent to a degree of relationship that is between second cousins once removed and third cousins. This indicates that most pairs of individuals have a low degree of relationship. The average degree of relationship for the whole tribe has not been measured, but the average sharing by descent of 1.2% is compatible with the tribal population's size and history.
All subjects were required to be 21 years of age or older and to be eligible for enrollment in the Southwestern tribe (≥¼ tribal ancestry); all 582 subjects were enrolled tribal members. Because of the high prevalence of alcoholism in this population, there was no need to ascertain subjects through alcoholic probands. Therefore, the subjects were selected on the basis of pedigree structure and accessibility only and without knowledge of or reference to their clinical histories or the clinical histories of relatives. Detailed genetic, demographic, and social data were collected, allowing systematic description of the representativeness of the study group and comparisons to the larger population of the tribe, best estimates for which were derived by using U.S. census data. A more detailed description of the study population and the Southwestern tribe is provided elsewhere (12).
Data on sociodemographic characteristics and psychiatric disorders were collected from all 582 subjects over a 4-year period (1991–1995). Although the research was designed initially as a genetics study, the investigators recognized that environmental factors could also influence outcomes. Therefore, the PTSD section of the Structured Clinical Interview for DSM-III-R (SCID) (13) and the Traumatic Events Booklet (14) were introduced midway through the study and applied consecutively to the final 247 participating subjects (117 men and 130 women). No additional inclusion or exclusion criteria or other selection bias were applied to this subgroup. All 582 participants were recruited in accordance with the study protocol.
Community support was instrumental in attaining a level of completeness that would have otherwise been unlikely. The study participants were recruited by local interviewers who were themselves members of the Southwestern tribe. Focus groups consisting of tribal staff and community members also assisted in the review of testing instruments, participant recruitment, and data collection. Considerable emphasis was placed on developing rapport with potential subjects. The participation rate was 93.7% of the eligible persons contacted. After complete description of the study, all subjects gave written informed consent under a human research protocol approved by the Institutional Review Board of the National Institute on Alcohol Abuse and Alcoholism and the tribal council. Each subject received a stipend of $40 for participation.
Clinical Measures
DSM-III-R diagnoses were made by using a modified version of the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (SADS-L), following operationally defined criteria, and using the instructions of Spitzer, Endicott, and Robins (15, 16). The validity of the SADS-L has been well established in population and clinical studies (17), and the SADS-L has been found to be reliable when administered by clinicians experienced in psychiatric assessment of American Indians (18–20). The diagnosis of PTSD was based on the PTSD component of the SCID (13).
Both the SADS-L interview and SCID PTSD component were administered by a psychologist (R.W.R.) with extensive experience in working with American Indian people. The written SADS-L semistructured clinical interview was blindly rated for DSM-III-R lifetime and current diagnoses for all disorders except PTSD, yielding acceptable rates of agreement between two independent blind raters—a clinical psychologist (B.C.) and a clinical social worker (kappa coefficients ranged from 0.63 to 0.96). The SCID PTSD component was also blindly rated, resulting in a kappa coefficient for PTSD of 1.00, attributed largely to the highly structured composition of the SCID, from which PTSD was diagnosed. Only after the psychiatric interviews were evaluated blindly by independent raters was a consensus conference held to resolve diagnostic differences among the interviewer and blind raters and to assign final diagnoses.
Provisions were made to limit diagnostic errors due to culture-specific phenomena. For example, depression is overdiagnosed in some American Indian societies in which it is normative to mourn for the death of secondary relatives for more than 3 months (21, 22). Schizophrenia can also be overdiagnosed in American Indian populations (23) when culture-specific hallucinatory experiences during religious ceremonies or mourning are perceived as psychosis (24, 25). In addition, high base rates of unemployment and lack of transportation can lead to overdiagnosis of antisocial personality and other disorders. Thus, the participants were questioned in detail about the specific circumstances that may have contributed to their unemployment.
Psychiatric disorders were evaluated typologically for lifetime (ever) and point (current) prevalences as defined by Spitzer et al. (15). To facilitate comparative analysis, DSM-III-R diagnoses were grouped into the following six categories:
Mood disorders: bipolar disorder (296.4x, 296.5x, 296.6x), bipolar disorder not otherwise specified (296.70), major depression (296.2x, 296.3x), dysthymia (300.40), depressive disorder not otherwise specified (311.00).
Alcohol disorders: alcohol dependence (303.90), alcohol abuse (305.00).
Antisocial personality disorder (301.70).
Anxiety disorders: anxiety disorder not otherwise specified (300.00), generalized anxiety disorder (300.02), obsessive-compulsive disorder (300.30), panic disorder without agoraphobia (300.01), phobia (300.22, 300.23, 300.29).
Drug disorders: drug dependence (304.00–304.60), drug abuse (305.20–305.90).
Posttraumatic stress disorder (309.89).
To test for the specific relationship between episodes of trauma and PTSD, PTSD was analyzed independently from other anxiety-related diagnoses.
The Traumatic Events Booklet (14) was administered consecutively to the last 247 enrolled subjects. This is a simple measure of potential events meeting DSM-III-R criterion A for PTSD and is currently being used in large-scale studies of Southwestern and Plains Indian communities. The booklet presents to the respondent yes-or-no questions about whether he or she has directly experienced or witnessed any of 10 traumatic events during his or her lifetime: combat, accident or crash, fire or explosion, industrial trauma, natural disaster, physical assault, witnessing extreme violence, dangerous situation, receiving news of the mutilation, serious injury, or violent or unexpected death of a loved one (not war related), or other traumatic event. Criterion A traumatic events are described as ones that are unusual, are extremely stressful or disturbing, and do not happen to most people. If several events are recorded, the respondent is asked to cite one event that is perceived as the “most upsetting,” and this event is assessed to determine whether criterion A is met by presenting the first section of the SCID PTSD component. If criterion A is met, the remaining sections of the SCID PTSD component are administered. Combat was treated as a discrete event and was not recorded for other event categories (e.g., dangerous situation, witnessing extreme violence). The temporal occurrence of events was evaluated in the recording of specific incidents of trauma.
Statistical Analyses
The mean ages at onset of PTSD for men and women were compared by using the t test for unpaired data with unequal variances. The two-sample Wilcoxon rank-sum test was used to test the equality of the median numbers of traumatic events for individuals with and without a PTSD diagnosis. The numbers of traumatic events experienced were categorized into quintiles of approximately equal size—0, 1 or 2, 3–5, 6–10, and >10—to facilitate further analysis. Pearson chi-square tests were used to determine associations between categorical number of traumatic events and presence or absence of PTSD diagnosis. Odds ratios were calculated for the prevalences of PTSD among men and women and for the occurrence of PTSD and other psychiatric disorders. Corresponding 95% confidence intervals were determined. Critical values were adjusted by using the Bonferroni adjustment for multiple comparisons. To evaluate sex, stratum-specific odds ratios were tested by using the Mantel-Haenszel test for heterogeneity. Sex was determined to be an effect modifier for PTSD, and so analyses were performed separately for men and women. Logistic regression was performed by using demographic variables, number of traumatic events, and type of traumatic event. Appropriate models were tested with log likelihoods.
Advantages and Limitations
A potential limitation of the genealogically based sampling strategy for estimating prevalence or collecting subjects with representative typology is that nonrepresentativeness could result from nonexhaustive sampling within families, ascertainment bias, or collection of a sample of families insufficient to describe the target population. The genealogical strategy used here involved comprehensive investigation of a unique population involving large and relatively homogeneous pedigrees. This method resulted in the collection of a large and genetically well-defined study group from a tribal population that is itself well circumscribed genetically, geographically, and culturally. However, our study group was not a randomly selected community-based sample and therefore has inherent limitations and biases. In subsequent analyses, the potential biases enumerated here were kept in mind; for example, data were separately analyzed by sex, and age was covaried. An additional limiting factor is the likelihood that a number of potential subjects were not included in our study population because of early death, including violent death. For this reason, individuals surviving to an older age would reflect an artificially low rate of traumatic events.
RESULTS
Our total study group consisted of 253 male and 329 female members of the Southwestern tribe. In general, the group's demographic characteristics were comparable with those from the largest Southwestern tribal reservation-based population (26). Substantial differences largely can be attributed to definitional variations. For example, the study group included common-law relationships—a common occurrence in many American Indian communities—in the married and divorced categories; the U.S. census data do not take these relationships into account. Other differences in definition that impeded comparison with U.S. census data involved education and household income.
The gender distribution of the PTSD subset examined in this investigation parallels the greater number of Southwestern tribal women aged 21 years or older in U.S. census figures (PTSD: 52.6%, N=130; U.S.: 52.2%, 2,706). Equal numbers of men and women refused to participate in the study. The demographic characteristics of the overall study group of 582 subjects did not differ substantially from the data subset for the 247 subjects who were assessed with the PTSD component of the SCID.
The overall lifetime prevalence of PTSD was 21.9% (N=54)—17.9% for the men (N=21) and 25.4% for the women (N=33). The overall point prevalence was 5.7% (N=14)—5.1% for the men (N=6) and 6.2% for the women (N=8). The women had slightly higher lifetime and point prevalences of PTSD than did the men, but there were no statistically significant gender differences (lifetime prevalence: odds ratio=1.56, 95% confidence interval=0.84–2.86; point prevalence: odds ratio=1.21, 95% confidence interval=0.43–3.46). The mean age at onset of PTSD did not differ significantly by gender (women: 16.4 years, SD=7.4; men: 20.3 years, SD=7.4) (t=1.81, df=49, p<0.08).
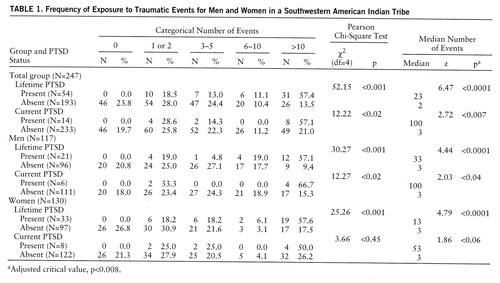
Table 1 presents the frequency of exposure to traumatic events by both lifetime and current PTSD diagnoses. The categorical number of traumatic events differed significantly between those with and without lifetime PTSD for both men and women. The median number of traumatic events was 23 for those with lifetime PTSD and only two for those without lifetime PTSD. When the subjects were classified according to current PTSD, the median number of events was 100 for those with current PTSD and only three for those without current PTSD. The differences for both lifetime and current diagnoses were significant.
The women had been exposed to more lifetime traumatic events than had the men (Pearson χ2=14.93, df=4, p<0.005). The likelihood of receiving a lifetime diagnosis of PTSD increased as a function of the number of reported traumatic events. Individuals who had experienced more than 10 traumatic events were more than eight times as likely to receive a diagnosis of lifetime PTSD than those who had experienced 10 or fewer events (odds ratio=8.66, 95% confidence interval=4.41–17.01).
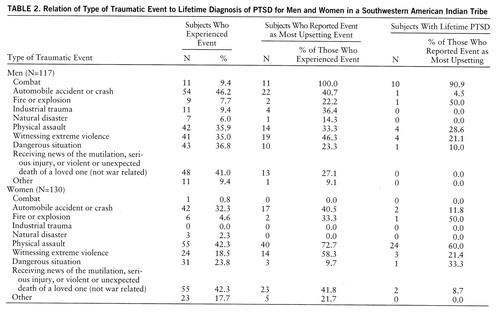
Table 2 lists the specific types of traumatic events and 1) the frequency with which each had been experienced by men and women, 2) the frequency with which they were reported as being the “most upsetting” (if experienced), and 3) the frequency of PTSD diagnosis (if the event was reported as the most upsetting). For both the men and women, the most frequently reported traumatic events were automobile accidents and receiving news of the mutilation, serious injury, or violent or unexpected death of a loved one (not war related). Additionally, physical assault (including physical sexual abuse) was reported by 42.3% of the women. Combat, witnessing violence, and automobile accidents were reported as the most upsetting by the men who had experienced these events. For the women, physical assault, witnessing violence, receiving news of the mutilation, serious injury, or violent or unexpected death of a loved one, and automobile accidents were described as the most upsetting events by the women who had experienced these events. Nearly every man who had been in combat developed PTSD. Over one-half of the women who reported physical assault as the most upsetting event were diagnosed with PTSD.
We examined the relationship of lifetime PTSD to other lifetime psychiatric disorders. Women with PTSD were more likely to be diagnosed with a mood disorder (odds ratio=3.29, 95% confidence interval=1.38–7.86), to have had a drug use disorder (odds ratio=2.84, 95% confidence interval=1.25–6.49), and to be diagnosed with antisocial personality disorder (odds ratio=2.81, 95% confidence interval=1.11–7.12) than women who were not diagnosed with PTSD. After an adjustment for multiple comparisons, these results were no longer statistically significant. No significant comorbid relationships were detected for men with PTSD, most likely because the frequency of psychiatric disorders among the men was so high and the number of men diagnosed with PTSD (N=21) was too low to reach statistical significance. Overall, the power to detect significant differences was reduced by the small number of individuals.
We performed logistic regressions separately by sex, relating the type and number of lifetime traumatic events to the diagnosis of lifetime PTSD. Potential confounders—age, income, education, and marital status—were not statistically significant. Interactions between type and number of events were also not significant.
Men who reported more than 10 traumatic events, after adjustment for the type of event, were more than six times as likely to develop PTSD than those reporting 10 or fewer traumatic events (odds ratio=6.48, 95% confidence interval=1.71–24.54, p<0.006). The only significant type of event predictive of PTSD in men was combat (odds ratio=45.58, 95% confidence interval=4.86–427.39, p<0.001). For women, there was no significant relationship between number of traumatic events and PTSD, after adjustment for type of event, and only physical assault was predictive of lifetime PTSD (odds ratio=46.50, 95% confidence interval=10.35–208.96, p<0.001).
DISCUSSION
This Southwestern American Indian study group, unselected for clinical or trauma history, had a prevalence of PTSD comparable to rates for groups selected for severe and extreme events, such as survivors of mass shootings, major burns, and combat (27). In comparison, the prevalence of PTSD in nonclinical non-Indian populations generally ranges from 1% to 9% (28).
Of the subjects who reported at least one traumatic event (81.4%, N=201), approximately one in four was diagnosed with lifetime PTSD (21.9%, N=54). This nearly 4:1 ratio has been found in other studies of PTSD (7). Also consistent with other findings (27, 29), the risk of developing PTSD was significantly greater for individuals with a history of multiple traumatic events. The high prevalence of PTSD in this community is, therefore, more likely due to a high rate of exposure to trauma and the types of traumatic events than to any specific vulnerability to PTSD.
Findings from national studies that indicate strong relationships between PTSD and other psychiatric disorders, including depression and substance abuse and dependence, were similarly demonstrated in our study group. Of our subjects who were diagnosed with lifetime PTSD, 83.3% (N=45) were each also diagnosed with at least one other lifetime psychiatric disorder. This rate is comparable to the 62%–80% range reported in studies from the Epidemiologic Catchment Area program (30). The rates of comorbid conditions in the men and women were not significantly different, possibly because of low statistical power.
While there were no statistically significant gender differences in the prevalences of PTSD, there were differences in the impact of specific events on men and women. The logistic regression demonstrated that type of event was more predictive than number of events. Physical assault was the most predictive variable for PTSD in the women. Twice as many female as male subjects perceived physical assault as the most upsetting experienced traumatic event (72.7% versus 33.3%) and developed PTSD as a result of physical assault (60.0% versus 28.6%). The strength of physical assault as a predictor of PTSD in women is most likely due to characteristics of the assault and victimization, such as sexual assault and abuse and domestic violence. The reports of the physical assaults experienced by the men are more indicative of mutual engagement in violence, often occurring in social contexts involving drinking.
For this community, analysis demonstrated that women who had been sexually abused as children (at age 15 or younger) were more likely to receive a lifetime diagnosis (odds ratio=5.27, 95% confidence interval=2.17–12.71) or current diagnosis (odds ratio=8.71, 95% confidence interval=1.34–56.11) of PTSD than were women who had not been sexually abused as children (10). However, only 45 of the 129 male and female subjects who reported histories of childhood sexual abuse responded affirmatively to the Traumatic Events Booklet question “Have you ever seen or experienced physical assault, torture, rape, abuse, mugging, or similar assault (not war-related)?” This question, therefore, was ineffective in recording childhood sexual abuse as either a physical assault or a rape. Possibly, people in this community view assault and rape as primarily adult phenomena. If incidents of childhood sexual abuse were considered, physical assault would likely be a more powerful predictor of PTSD in women. This finding suggests that trauma lists, such as the Trauma Events Booklet, need to be more specific in questions involving assault as a criterion A event.
Combat was the most powerful predictor of PTSD in men. The 10 combat veterans who developed PTSD participated in the Vietnam war (N=4), the Korean conflict (N=3), secret missions in other regions (N=2), and World War II (N=1). Four of these subjects served in high-risk reconnaissance units; the other six subjects were situated in artillery divisions and/or on the front lines. Preliminary data from the American Indian Vietnam Veterans Project (31) indicate that American Indian war theater veterans have a higher rate of PTSD than any other racial group. This high rate of PTSD has been attributed primarily to extremely stressful and vulnerable assignments as scouts or point men and a higher frequency of being wounded in action than has been found for non-Indians (31, 32). It is also possible that prewar exposure to multiple traumatic events may have increased the vulnerability of American Indian combat veterans to PTSD.
The PTSD diagnosis is a categorical classification of a set of behaviors. It should not be presumed that diagnostic categories are cross-culturally valid, but the question can be empirically addressed. The relationship of PTSD prevalence to exposure to traumatic events and the greater likelihood of PTSD after specific trauma lend credibility to the use of PTSD as a meaningful diagnostic entity in this Southwest American Indian community. After reviewing four ongoing studies covering different stages of the developmental cycle, Manson et al. (31) concluded that PTSD is an important part of the large and complex picture of trauma within American Indian communities.
The impact of discrete and acute traumatic events occurring within the context of cumulative, long-term, and intergenerational trauma is an important factor to consider (33). Efforts have been made to determine the effects of specific extreme stressors for other indigenous populations characterized by their extensive histories of trauma (34, 35), as well as for refugees (36) and victims of political torture (37).
In this Southwestern American Indian community, the chronic nature of extreme stress does not preclude identification of acute events that result in PTSD. While demonstrating high rates of exposure to multiple traumatic events, this study underscores the importance of examining individual events that may be potent predictors of PTSD. In a context of considerable community trauma, these discrete events may challenge a threshold beyond which PTSD emerges as a response.
 |
 |
Received Aug. 5, 1996; revision received April 4, 1997; accepted June 6, 1997. From the Laboratory of Neurogenetics, National Institute on Alcohol Abuse and Alcoholism, Rockville, Md. Address reprint requests to Dr. Robin, LNG/NIAAA/NIH, P.O. Box 617, Sitka, AK 99835; [email protected] (e-mail). Funded by the Intramural Program of the National Institute on Alcohol Abuse and Alcoholism.
1. Kettl PA: Homicide in Alaska Natives. Alaska Med 1993; 35:168–172Medline, Google Scholar
2. Blum RW, Harmon B, Harris L, Bergeisen L, Resnick MD: American Indian—Alaska Native youth health. JAMA 1992; 267:1637–1644Google Scholar
3. Dinges NG, Joos SK: Stress, coping, and health: models of interaction of Indian and Native populations. Am Indian Alask Native Ment Health Res 1993; 1:8–64Google Scholar
4. Chester B, Robin RW, Koss MK, Lopez J, Goldman D: Grandmother dishonored: violence against women by male partners in American Indian communities. Violence Vict 1994; 9:249–258Crossref, Medline, Google Scholar
5. Resnick HS, Kilpatrick DG: Crime-related PTSD: emphasis on adult general population samples. PTSD Res Q 1994; 5:1–7Google Scholar
6. Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL: Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol 1993; 61:984–991Crossref, Medline, Google Scholar
7. Breslau N, Davis GC, Andreski P, Peterson E: Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry 1991; 48:216–222Crossref, Medline, Google Scholar
8. Population Estimates 1992–1994. Phoenix, Arizona Department of Economic Security, 1996Google Scholar
9. Chester B: Evaluation for the Southwestern Indian Community, Department of Health Services, Concerning Possible Integration of the Alcohol and Drug Abuse Program With the Behavioral Health Clinic: Desirability and Feasibility: Report Presented to the Southwestern Indian Tribal Council and Department of Health Services. Phoenix, Arizona Department of Health Services, April 23, 1993Google Scholar
10. Robin RW, Chester B, Rasmussen JK, Jaranson JM, Goldman D: Childhood sexual abuse and associated psychiatric disorders in a southwestern American Indian tribal community (abstract). Am J Epidemiol 1996; 143(suppl 11):S56Google Scholar
11. Robin RW, Long JC, Rasmussen JK, Chester B, Jaranson JM, Goldman D: Comorbidity of alcoholism and other psychiatric disorders in a Southwestern American Indian community (abstract). Alcohol Clin Exp Res 1995; 19(April suppl):92AGoogle Scholar
12. Robin RW, Chester B, Rasmussen JK, Jaranson JM, Goldman D: Prevalence, characteristics, and impact of childhood sexual abuse in a Southwestern American Indian tribe. Child Abuse Negl (in press)Google Scholar
13. Spitzer RL, Williams JBW, Gibbon M, First MB: User's Guide for the Structured Clinical Interview for DSM-III-R (SCID). Washington, DC, American Psychiatric Press, 1990Google Scholar
14. Davidson JRT, Smith RD: Traumatic experiences in a psychiatric outpatient population. J Trauma Stress 1990; 3:459–474Crossref, Google Scholar
15. Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria (RDC) for a Selected Group of Functional Disorders, 3rd ed, updated. New York, New York State Psychiatric Institute, Biometrics Research, 1989Google Scholar
16. Endicott J, Spitzer RL: A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry 1978; 35:837–844Crossref, Medline, Google Scholar
17. Hesselbrock B, Stabenau J, Hesselbrock M, Mirkin P, Meyer R: A comparison of two interview schedules: the Schedule for Affective Disorders and Schizophrenia—Lifetime Version and the National Institute of Mental Health Diagnostic Interview Schedule. Arch Gen Psychiatry 1982; 39:674–677Crossref, Medline, Google Scholar
18. Shore JH, Manson SM, Bloom JD, Keepers G, Neligh G: A pilot study of depression among American Indian patients with research diagnostic criteria. Am Indian Alask Native Ment Health Res 1987; 1:4–15Crossref, Medline, Google Scholar
19. Boehnlein JK, Kinzie JD, Leung PK, Matsunaga D, Johnson R, Shore JH: The natural history of medical and psychiatric disorders in an American Indian community. Cult Med Psychiatry 1993; 16:543–554Google Scholar
20. Somervell PD, Beals J, Kinzie JD, Boehnlein J, Leung P, Manson SM: Use of the CES-D in an American Indian village. Cult Med Psychiatry 1993; 16:503–517Google Scholar
21. Manson SM, Shore JH, Bloom JD: The depression experience in American Indian communities: a challenge for psychiatric theory and diagnosis, in Culture and Depression. Edited by Kleinman A, Good B. Berkeley, University of California, 1985, pp 331–368Google Scholar
22. Shore JH, Manson SM: Cross-cultural studies of depression among American Indians and Alaska Natives. White Cloud J 1981; 2:5–12Google Scholar
23. Pelz M, Merskey H, Brant C, Patterson PGR, Heseltine GFD: Clinical data from a psychiatric service to a group of Native people. Can J Psychiatry 1981; 26:345–348Crossref, Medline, Google Scholar
24. Shen W: The Hopi Indians' mourning hallucinations. J Nerv Ment Dis 1986; 74:365–367Crossref, Google Scholar
25. Matchett WF: Repeated hallucinatory experiences as part of the mourning process among Indian women. Psychiatry 1972; 35:185–194Crossref, Medline, Google Scholar
26. United States Bureau of the Census: Census of Population and Housing. Phoenix, Arizona Data Center, Population Statistics Unit, Department of Economic Security, 1990Google Scholar
27. de Girolamo G, McFarlane AC: The epidemiology of PTSD: a comprehensive review of the international literature, in International Handbook of Traumatic Stress Syndromes. Edited by Wilson JP, Raphael B. New York, Plenum, 1993, pp 33–86Google Scholar
28. Norris FH: Epidemiology of trauma: frequency and impact of different potentially traumatic events on different demographic groups. J Consult Clin Psychol 1992; 60:409–418Crossref, Medline, Google Scholar
29. Yehuda R, Kahana B, Schmeidler J, Southwick SM, Wilson S, Giller EL: Impact of cumulative lifetime trauma and recent stress on current posttraumatic stress disorder symptoms in Holocaust survivors. Am J Psychiatry 1995; 152:1815–1818Google Scholar
30. Davidson RT, Fairbank JA: The epidemiology of posttraumatic stress disorder, in Posttraumatic Stress Disorder: DSM-IV and Beyond. Edited by Davidson JRT, Foa EB. Washington, DC, American Psychiatric Press, 1993, pp 147–172Google Scholar
31. Manson SM, Beals J, O'Nell T, Piasecki J, Bechtold D, Keane E, Jones M: Wounded spirits, ailing hearts: PTSD and related disorders among American Indians, in Ethnocultural Aspects of Posttraumatic Stress Disorder: Issues, Research, and Clinical Applications. Edited by Marsella AJ, Friedman MJ, Gerrity ET, Scurfield RM. Washington, DC, American Psychological Association, 1996, pp 255–283Google Scholar
32. Holm T: The national survey of Indian Vietnam veterans. Am Indian Alask Native Ment Health Res 1994; 6:18–28Crossref, Medline, Google Scholar
33. Robin RW, Chester B, Goldman D: Cumulative trauma and PTSD in American Indian communities, in Ethnocultural Aspects of Posttraumatic Stress Disorder. Edited by Marsella AJ, Friedman MJ, Gerrity ET, Scurfield RM. Washington, DC, American Psychological Association, 1996, pp 239–253Google Scholar
34. Duran E, Duran B: Native American Postcolonial Psychology. New York, State University of New York Press, 1995Google Scholar
35. Macedo H: Community trauma and community interventions. Arctic Med Res 1988; 47(suppl 1):94–96Google Scholar
36. Mollica R: The trauma story: the psychiatric care of refugee survivors of violence and torture, in Post-Traumatic Therapy and Victims of Violence. Edited by Ochberg F. New York, Brunner/Mazel, 1988, pp 295–314Google Scholar
37. Chester B, Jaranson JM: The context of survival and destruction: conducting psychotherapy with survivors of torture. Clin Q 1994; 4:17–20Google Scholar



