Cannabis, Inhibitory Neurons, and the Progressive Course of Schizophrenia
The neurons of individuals with schizophrenia appear to be under stress. Unlike the neurons of healthier brains, these neurons have smaller cell bodies and stunted dendritic branches. The connections between them appear to be diminished and they have stopped making many of the special substances, such as neurotransmitters, that distinguish them and their functions from other cells in the body. It is a stunning feat of cell biology for a nerve cell to amass the enormous amounts of energy required to synthesize the protein machinery that enables it to receive and transmit information and to then elaborate its large branched axons and dendrites to connect with other neurons (the dendrites and axon of a single inhibitory neuron of the cerebral cortex are shown on the cover of this month’s issue). But when a neuron is stressed, it preserves its own cellular life first. It gradually stops making the many proteins that it needs to carry out its functions. It begins to retract its dendrites and axon branches to function as a simpler cell. Diminished brain size has long been recognized as a common feature of schizophrenia. The number of neurons appears to be intact, but there is loss of the axons and dendrites that connect the neurons with each other. If the pathophysiology of this loss of neuron structure and function in schizophrenia were better understood and could be arrested, individuals with schizophrenia might be spared the cognitive and social decline that occurs over the course of the illness.
Two articles in this issue of the Journal provide further evidence about the loss of neuron function and structure in schizophrenia. In the first article, Hashimoto et al. present data that increase the evidence for loss of inhibitory function in interneurons throughout the neocortex in schizophrenia. Hashimoto et al. studied the expression of genes that synthesize gamma-aminobutyric acid (GABA), the inhibitory neurotransmitter of interneurons, GABA transporters, and GABA receptor subunits, as well as genes for somatostatin and parvalbumin, proteins that are found in inhibitory interneurons. They found that the expression of these genes was diminished in the dorsolateral prefrontal cortex, the anterior cingulate, and the primary motor and visual cortices in brain tissue obtained postmortem from 12 subjects who had schizophrenia in life, compared to tissue from 12 unaffected individuals. The only gene studied whose expression did not change was the gene for calretinin, a protein found only in a subclass of interneurons that primarily inhibit other inhibitory interneurons and thereby diminish inhibition for the brain as a whole. Thus, Hashimoto et al.’s findings suggest that the cerebral cortex of individuals with schizophrenia lacks normal inhibitory neuronal machinery. This neuronal machinery is thought to be essential to the brain’s cognitive functions. Deficits in inhibitory neurons in schizophrenia have been found by a number of investigators in various brain regions. Hashimoto et al.’s study is the first to present evidence that the deficit is widespread throughout the neocortex.
In the second article, Rais et al. used MRI to document that the brains of individuals with schizophrenia, including the neocortex, are progressively diminished. They compared 51 patients with recent onset of schizophrenia to 31 healthy comparison subjects. Each subject’s brain was imaged twice at 5-year intervals. Gray matter loss over the 5-year period was greater in patients with schizophrenia, as has been previously observed. The new finding was that the 19 patients with schizophrenia who used cannabis during the 5-year interval lost tissue at nearly twice the rate of the 32 patients with schizophrenia who did not use cannabis during this interval. None of the patients reported other drug abuse. While we do not know for sure if cannabis abuse is the causative agent in the loss of brain tissue or if the loss of brain tissue due to the course of illness causes patients to abuse cannabis, the fact that both cannabis abusers and non-cannabis abusers did not differ in brain size or psychopathology at the initial examination suggests that cannabis is the causal agent.
David Lewis, the senior author of the Hashimoto et al. article, and Stephen Eggan have examined human brain tissue for the expression of the cannabinoid CB 1 receptor, the receptor activated by cannabis (1) . Figure 1 shows CB 1 immunocytochemical labeling of these receptors in the human cortex. Eggan and Lewis presented electron microscopic evidence that many of these CB 1 receptors are located on inhibitory interneurons. Neurobiological studies in laboratory animals suggest that activation of these receptors decreases the release of GABA, essentially decreasing inhibition of the cerebral cortex.
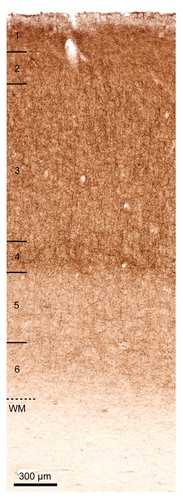
Figure by Stephen Eggan, Leonid Krimer, and David Lewis. (Figure adapted from S. Eggan and D. Lewis, “Immunocytochemical Distribution of the Cannabinoid CB1 Receptor in the Primate Neocortex: A Regional and Laminar Analysis” [Cereb Cortex 2007; 17:175–191] with permission from Oxford University Press.)
Why would individuals with schizophrenia want to use cannabis, which further decreases inhibition of the cerebral cortex, when they are already losing inhibitory interneuron function? Functional MRI of brain activity demonstrates that neuronal activity is decreased in the frontal lobe of many patients with schizophrenia. When they are asked to complete a task, these patients often respond with increased activity over a wider area of the frontal lobe than that of normal subjects asked to perform the same task (2) . Patients with schizophrenia appear to need to increase their brain’s excitatory activity to compensate for other deficits in brain function. If cannabis blocks the release of GABA, the result is that their brains are more readily excited. Cannabis may therefore help individuals with schizophrenia achieve the more widespread levels of excitation in the frontal lobe that are required to match the performance of other individuals.
Unfortunately, there are problems caused by the loss of inhibition. Inhibition normally supports cognitive function by helping neurons to attune themselves to only respond to target stimuli of interest and to inhibit their response to extraneous or distracting material. Individuals with schizophrenia already have hyperactive sensory and limbic areas (3) . Further loss of inhibition in these areas may contribute to distractibility and the inability to distinguish between internal and external stimuli in individuals with schizophrenia, a failure that may underlie the occurrence of hallucinations and other forms of thought disorder. Thus, cannabis use has been associated with exacerbation of psychotic symptoms (4) .
There are further long-term consequences of prolonged cannabis use. Excitatory neurotransmission between neurons is the mechanism by which one neuron changes the activity of another in the service of conveying and processing information. However, excitatory neurotransmission works by admitting sodium and calcium ions into the neuron. In large amounts, these ions are toxic and can stress the neuron, resulting in loss of neuronal functions (such as the ability to synthesize inhibitory neurotransmitters), loss of dendrites, and ultimately cell death, a process called excitotoxicity (5 , 6) . The mechanism of neuronal stress in schizophrenia is unknown, but excitotoxicity is one possible mechanism because of the hyperactivity and loss of inhibition that has already been described. Activation of cannabinoid CB 1 receptors generally has a neuroprotective effect, but chronic exposure to cannabinoids, as occurs in severe cannabis addiction, desensitizes cannabinoid CB 1 receptors (7 , 8) . The desensitized receptors then can no longer help protect neurons against the stress of increased excitation. These neuronal effects of chronic cannabis exposure may mediate the accelerated loss of brain tissue observed by Rais et al. in patients with schizophrenia who abuse cannabis.
What should psychiatrists advise patients with schizophrenia about cannabis use? Many treatment programs have given up trying to prohibit cannabis use, for much the same reasons they used to not prohibit smoking tobacco. Both substances are avidly abused by individuals with schizophrenia and both may have some transitory effects that seem positive. It is therefore difficult to prevent their abuse. Alcohol is less avidly abused but also increases brain tissue loss in schizophrenia. The new data suggest that cannabis should now join nicotine and alcohol as a substance that has significant long-term negative consequences that patients and their families need to understand. Information about these negative effects and treatment for cannabis abuse seem warranted as one of the few things that psychiatrists can do to help patients with schizophrenia prevent further decline in cognitive function.
1. Eggan SM, Lewis DA: Immunocytochemical distribution of the cannabinoid CB1 receptor in the primate neocortex: a regional and laminar analysis. Cereb Cortex 2007; 17:175–191Google Scholar
2. Callicott JH, Mattay VS, Verchinski BA, Marenco S, Egan MF, Weinberger DR: Complexity of prefrontal cortical dysfunction in schizophrenia: more than up or down. Am J Psychiatry 2003; 160:2209–2215Google Scholar
3. Tregellas JR, Davalos DB, Rojas DC, Waldo MC, Gibson L, Wylie K, Du YP, Freedman R: Increased hemodynamic response in the hippocampus, thalamus and prefrontal cortex during abnormal sensory gating in schizophrenia. Schizophr Res 2007; 92:262–272Google Scholar
4. Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, Lewis G: Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet 2007; 370:319–328Google Scholar
5. Marsicano G, Goodenough S, Monory K, Hermann H, Eder M, Cannich A, Azad SC, Cascio MG, Gutiérrez SO, van der Stelt M, López-Rodriguez ML, Casanova E, Schütz G, Zieglgänsberger W, Di Marzo V, Behl C, Lutz B: CB1 cannabinoid receptors and on-demand defense against excitotoxicity. Science 2003; 302:84–88Google Scholar
6. Kim SH, Won SJ, Mao XO, Jin K, Greenberg DA: Molecular mechanisms of cannabinoid protection from neuronal excitotoxicity. Mol Pharmacol 2006; 69:691–696Google Scholar
7. Greenwood SM, Mizielinska SM, Frenguelli BG, Harvey J, Connolly CN: Mitochondrial dysfunction and dendritic beading during neuronal toxicity. J Biol Chem 2007; 282:26235–26244Google Scholar
8. Monnerie H, Le Roux PD: Reduced dendrite growth and altered glutamic acid decarboxylase (GAD) 65- and 67-kDa isoform protein expression from mouse cortical GABAergic neurons following excitotoxic injury in vitro. Exp Neurol 2007; 205:367–382Google Scholar



