Trauma, Resilience, and Recovery in a High-Risk African-American Population
Abstract
Objective: Despite increased risk for psychiatric disorders after trauma exposure, many people are able to adapt with minimal life disruption, and others eventually recover after a symptomatic period. This study examined psychosocial factors associated with resilience and recovery from psychiatric disorders in a high-risk sample of African American adults exposed to a range of severe traumas, who participated in structured diagnostic interviews. Method: The sample included 259 patients exposed to at least one severe traumatic event, recruited from primary care offices at Howard University and administered the Structured Clinical Interview for DSM-IV Axis I disorders. Multinomial logistic regression was used to identify potential psychosocial factors associated with resilience and recovery, including purpose in life, mastery, and coping strategies. Results: Forty-seven patients had no lifetime psychiatric disorders (resilient), 85 met criteria for at least one past DSM-IV disorder but no current disorders (recovered), and 127 met criteria for at least one current DSM-IV disorder (currently ill). The resilient group was characterized by a significantly lower lifetime trauma load. Female gender was predictive of currently ill status. In the final model, purpose in life emerged as a key factor associated with both resilience and recovery, and mastery was also significantly associated with recovery. Conclusions: The identification of psychosocial factors associated with resistance to severe trauma can inform future studies of preventive and treatment interventions for high-risk populations. Further study is needed to determine which psychosocial factors are consistently associated with resilience and to what extent they can be modified through clinical intervention.
Most people are exposed to at least one traumatic event during their lifetime (1 – 3) . Although trauma can increase the risk for a range of psychiatric disorders, studies have consistently shown that many people are able to adapt with minimal disruption to their lives and others are eventually able to recover their baseline level of functioning after a symptomatic period (1 , 4) . Improving our understanding of psychological characteristics associated with resistance to severe stress can inform preventive and treatment interventions for trauma-exposed individuals.
A large body of research on resilience has come from studies in children and adolescents exposed to a variety of stressors (5 , 6) . Fewer studies have been conducted with adult populations (7) . Although detailed information is available on risk factors for posttraumatic stress disorder (PTSD) (2 , 3) , resilience in adults has often been misunderstood because much of what we know about coping in trauma-exposed adults comes from studies of treatment-seeking or distressed individuals recruited from psychiatric treatment settings (1) . Definitions of resilience have also varied across studies. Studies in children have defined resilience as good adjustment across different domains despite significant adversity (5 , 6) . Comparatively few studies have examined resilience in adults exposed to severe traumas, defined as the absence of psychopathology by DSM-IV criteria (8 – 10) . Initial findings suggest that it is important to distinguish resilience from recovery after a symptomatic period (1) .
Results from hallmark epidemiologic studies indicate that severe traumas, and in particular assaultive trauma, carry the highest risk for PTSD (2 , 11) . The study of populations at high risk for trauma provides a unique opportunity to examine psychosocial characteristics associated with resilience. Studies have shown that African American individuals living in central-city areas have high rates of exposure to trauma and in particular to assaultive trauma (11) . The few published studies examining individual characteristics associated with better adjustment in African American adults have focused on specific types of trauma or coping strategies and have assessed mental health outcomes exclusively with self-report questionnaires (12 – 14) , with the exception of one study using the Clinician-Administered PTSD Scale (CAPS) (15) .
The present study was conducted in an urban sample of African American adults exposed to a range of severe traumas, often on a repeated basis, who participated in structured diagnostic interviews administered by trained experienced clinicians. We were interested in studying individual factors found to be associated with positive adjustment in prior studies, such as optimism and adaptive coping strategies, as well as exploring less-studied factors such as religious involvement and religious coping, known to be of central importance in African American cultures (16) . Based on previous research, we expected that higher use of adaptive coping strategies (e.g., active coping, emotional expression, and the ability to elicit social support), higher levels of optimism, mastery, and purpose in life, and lower use of avoidant coping strategies (e.g., denial, behavioral disengagement, substance use) would be associated with resilience and recovery. Based on epidemiological research findings, we expected that female gender (17) and more severe trauma exposure (17 , 18) would predict psychiatric illness. Finally, we set out to examine similarities and differences in psychosocial factors associated with resilient versus recovered status.
Method
The study participants were recruited from primary care offices at Howard University Hospital. The staff members approached the patients in the waiting areas as they came in to wait for their doctors. The primary care setting was used to develop a cohort of trauma-exposed individuals to study with detailed interviews. This study was not designed to determine the prevalence of psychiatric disorders in this setting. After complete description of the study to the subjects, written informed consent was obtained. Forty-one percent of patients attending the clinics consented to complete the self-report questionnaire. Reasons for nonparticipation included ineligibility because of not speaking English, medical acuity, pain and discomfort, or refusals in some cases owing to concerns about research participation. The self-report questionnaire included demographic information and the Life Events Checklist from the CAPS inquiring about the lifetime occurrence of traumatic events in 17 trauma categories (e.g., natural disasters, physical assault, sexual assault) (19) . A significant traumatic event was defined as an unambiguously high-impact trauma (e.g., sexual or physical assault, assault with a weapon, serious accident). The participants who only endorsed events that are not uniformly severely traumatic (e.g., motor vehicle accident) were screened further by telephone to determine trauma severity. All patients who identified at least one significant traumatic event meeting criterion A1 in DSM-IV-TR were invited to participate in an in-person assessment of lifetime psychiatric disorders with the Structured Clinical Interview for DSM-IV Axis I Disorders, Nonpatient Edition (SCID-I/NP) (20) , and the current and lifetime CAPS, conducted by trained clinical interviewers (see reference 21 for a more detailed description).
Of a total of 738 patients surveyed, 472 (64.0%) met criteria for trauma exposure, 351 of 472 (74.4%) participated in diagnostic interviews, and 323 of 472 (68.4%) had complete data. We compared trauma-exposed participants and nonparticipants on demographics and severity of trauma exposure using t tests for continuous variables and chi-square tests for categorical variables. The two groups did not differ significantly in gender or age. The study participants were significantly more likely to be single than the nonparticipants (76.2% versus 63.3%, p=0.006) and reported higher education at a level approaching significance (mean=12.7 years [SD=3.1] versus mean=12.0 years [SD=4.1]; p=0.06). They also reported a significantly higher mean number of lifetime trauma categories (mean=4.6 years [SD=2.4] versus mean=3.9 years [SD=2.2]; p=0.003) and significantly higher exposure to assaultive trauma (79.4% versus 69.2%, p=0.02).
After exclusion of patients with bipolar or psychotic disorders, as these disorders are least likely to be related to trauma exposure, the final sample included 259 patients who were exposed to at least one event meeting DSM-IV-TR criterion A1 for trauma exposure. We then grouped participants into three diagnostic groups: 1) patients in the resilient group (N=47) were characterized by the absence of any lifetime DSM-IV psychiatric disorders, 2) those in the recovered group (N=85) met criteria for at least one past DSM-IV disorder but had no current disorders, and those in the currently ill group (N=127) met criteria for at least one current DSM-IV disorder. Of note, some studies have distinguished individuals who develop symptoms but do not meet criteria for any axis I disorder from those who develop few or no symptoms after trauma (10 , 17) . In the present study, both are included in the resilient group. During face-to-face interviews, only 9% of participants in the currently ill group (12 of 127) reported that they were currently receiving specialized mental health treatment. Of a subset of 123 participants from all three diagnostic groups, only 37% reported having discussed their trauma or any mental health problems with their primary care provider.
Measures
The participants completed the following self-report measures (see data supplement available at http://ajp.psychiatryonline.org for references and further information). The Life Orientation Test–Revised (LOT-R) measures dispositional optimism, the tendency to expect positive outcomes. The Purpose in Life Scale assesses a person’s sense of purpose and direction in life. The Pearlin Mastery Scale measures the extent to which an individual feels control over his life. A 7-item version of the RCOPE was used to assess to what extent positive and negative religious coping is involved in the way respondents generally cope with major life problems. The frequency of religious service attendance was assessed with the question “How often do you go to religious services?” Religiosity and spirituality were assessed with the questions “To what extent do you consider yourself a religious person?” and “To what extent do you consider yourself a spiritual person?” respectively. The Posttraumatic Growth Inventory (PTGI) measures positive changes in different areas of life (e.g., beliefs, relationships, attitudes) attributed to “the most traumatic or stressful experience” in the respondent’s life.
A 36-item modified version of the COPE, including additional items measuring emotional processing, expression, and self-distraction, was administered to assess a range of generally used coping strategies. An exploratory factor analysis of the modified COPE yielded five factors, accounting for 50.9% of the variance. These were “active coping” (e.g., positive reinterpretation, active coping, and planning), “avoidant coping” (behavioral disengagement and denial), “emotional expression,” “substance use,” and “use of social supports” (instrumental and emotional).
Data Analysis
All analyses were performed using SPSS 14.0. Lifetime trauma load was estimated in the form of two variables: 1) the total number of trauma categories endorsed (e.g., natural disasters, physical assault, sexual assault) and 2) trauma type, consisting of three exposure levels: a) at least one lifetime sexual assault (“sexual assaultive”), b) at least one lifetime assaultive trauma but no history of sexual assault (“nonsexual assaultive”), and c) at least one lifetime trauma but no history of assaultive trauma (“nonassaultive”). Demographic characteristics and lifetime trauma load were compared across the three diagnostic groups (resilient, recovered and currently ill) with one-way analysis of variance (ANOVA) for continuous variables (age, education, and total number of trauma categories) and chi-square tests for categorical variables (gender, marital status [married/cohabiting versus single/separated/divorced], and trauma type). Correlation coefficients were calculated to examine relationships between psychosocial variables in the whole sample.
To examine which psychosocial variables were associated with resilience or recovery, multinomial logistic regression was used, with diagnostic group as the outcome and the currently ill group as the reference group. For the resilient-recovered comparison, analyses were subsequently repeated with the recovered group as the reference group. In the first step, only demographic characteristics and the two trauma variables were included in the model. In the second step, each psychosocial variable was tested individually, with demographic characteristics and the two trauma variables included in each model as covariates (partially adjusted models). Finally, multinomial logistic regression analysis was conducted using the forward selection method to enter all psychosocial variables in order to identify the most significant ones, after adjustment for the six covariates (fully adjusted model). The forward selection method was chosen because of the likely correlation among psychosocial predictors. All statistical tests were two-tailed.
Results
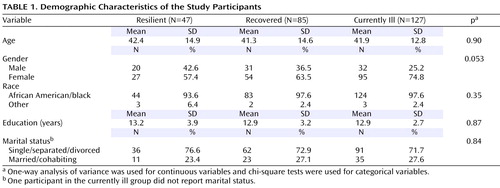
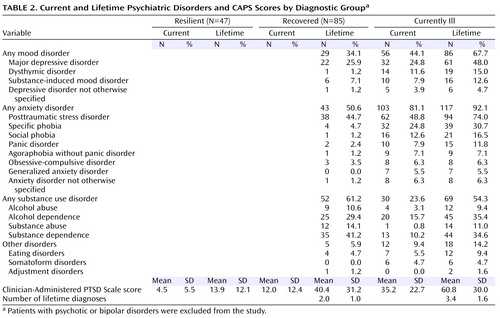
Demographic characteristics are summarized in Table 1 . The three diagnostic groups did not differ significantly on demographic characteristics; they differed on gender composition at the nearly significant level ( Table 1 ). Psychiatric diagnoses in the sample consisted primarily of depressive, anxiety and substance use disorders. PTSD was the most common diagnosis ( Table 2 ). By definition, the resilient group (N=47) had no lifetime history of psychiatric disorders. In the currently ill group (N=127), 75 patients (59.1%) had more than one comorbid current psychiatric disorder. By definition, patients in the recovered group (N=85) only had past psychiatric disorders. In this group, 50 patients (58.8%) had recovered from more than one past psychiatric disorder. Mean current and lifetime CAPS scores for each diagnostic group are listed in Table 2 .
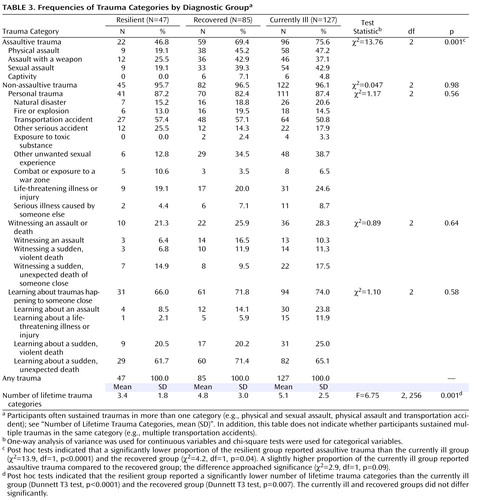
Table 3 lists the frequency of trauma categories by diagnostic group. Lifetime exposure to assaultive trauma and mean total number of lifetime trauma categories were significantly different in the three groups ( Table 3 ). Post hoc comparisons revealed significantly lower exposure to assaultive trauma and a significantly lower mean number of lifetime trauma categories in the resilient compared to the other two groups.
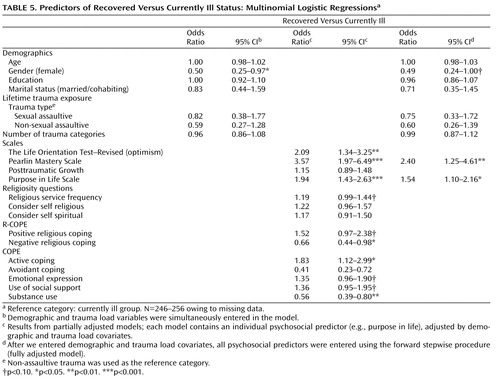
There was a large degree of intercorrelation among several of the psychosocial factors (see Table 5 in data supplement). Table 4 and Table 5 show the results of multinomial logistic regression analyses examining psychosocial factors associated with resilient and recovered status, with the currently ill group as the reference group. Female gender, lifetime exposure to a higher number of trauma categories, and a history of sexual or nonsexual assaultive trauma significantly predicted currently ill versus resilient status in the fully adjusted model. A higher number of trauma categories significantly predicted recovered versus resilient status (see data supplement). In further direct comparisons between sexual and nonsexual assaultive trauma types as predictors of diagnostic status, there were no significant differences in any of the analyses (see data supplement).
In the partially adjusted models, there was considerable overlap in psychosocial factors associated with resilient versus currently ill status ( Table 4 ) and recovered versus currently ill status ( Table 5 ). In the resilient versus recovered group comparison, there were no significant psychosocial factors, and posttraumatic growth was associated with recovered status at a nearly significant level (see data supplement). In the fully adjusted model, purpose in life was significantly associated with both resilient versus currently ill status and recovered versus currently ill status. In addition, mastery was significantly associated with recovered versus currently ill status ( Table 4 , Table 5 , Figure 1 ). The fully adjusted model for the resilient versus recovered group comparison revealed no significant psychosocial factors (see data supplement).
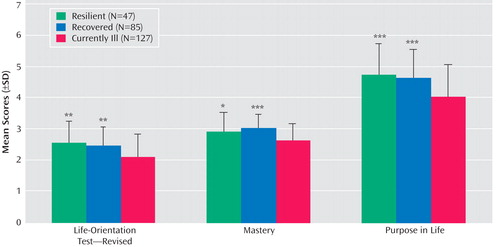
a One-way analyses of variance showed that there were significant group differences on optimism (F=10.74, df=2, 255, p<0.0001), mastery (F=11.28, df=2, 256, p<0.0001), and purpose in life (F=14.71, df=2, 252, p<0.0001).
b In post hoc analyses, both the resilient and recovered groups had significantly higher mean scores than the currently ill group on all three variables. The resilient group did not differ significantly from the recovered group on any of the three variables.
*p<0.01. **p<0.001. ***p<0.0001.
Discussion
To our knowledge, this study is the first to examine psychosocial factors associated with resilience and recovery from psychiatric disorders in a high-risk sample of African American adults exposed to a range of severe traumas assessed with face-to-face diagnostic interviews. Consistent with prior studies (18 , 22) , we found a significantly lower lifetime trauma load in the resilient group, including less exposure to assaultive trauma. Of note, trauma load did not significantly differ between the recovered and currently ill groups, suggesting that other factors are important for recovery. The fact that sexual assaultive trauma was not more strongly associated with currently ill status than nonsexual assaultive trauma in our sample may be due to the severity of nonsexual assaultive trauma in our participants. As expected, female gender was predictive of currently ill status (2 , 11 , 17) . In the final model, purpose in life emerged as a key psychosocial factor associated with both resilience and recovery, and mastery was an additional important factor associated with recovery.
Purpose in Life
The finding that a sense of purpose in life was strongly associated with both resilient and recovered status is in line with the theories of existential writers such as Victor Frankl, who first postulated that a sense of meaning and purpose influence how individuals cope with stress (23) . This finding also agrees with previous reports of associations between a sense of meaning in the face of stress and mental health outcomes (24) . As proposed by Janoff-Bulman (25) , trauma may shatter an individual’s existing schemas, deeply affecting his or her sense of purpose and meaning. A strong sense of purpose predating trauma exposure may promote resilient outcomes, while regaining a sense of purpose may be central to the process of recovery. In cancer patients, counseling sessions focused on enhancing meaning-making have been found to decrease depression and increase life satisfaction (26) .
Another important factor associated with recovered versus currently ill status in this study was mastery. This finding is consistent with previous reports of an inverse relationship between mastery and PSTD symptoms (27) , as well as between mastery and depressive symptoms in both white (28) and African American populations (29) . In African Americans, mastery has also been found to correlate with higher levels of self-efficacy and positive ethnic identity (30) .
Recent studies have found significant associations between religion and spirituality and mental health (31) . In the present study, a higher frequency of religious service attendance was significantly associated with resilient status, while simply considering oneself religious or spiritual was not. Active involvement in a religious community represents a more common, more valued, and less stigmatized source of social support than traditional mental health services for many African Americans (16 , 32) . Of note, while service attendance may be protective in resilient individuals, people who suffer from PTSD may become less religious over time (33) .
Negative religious coping has been linked to higher levels of distress (31) . A recent study of African American women who experienced intimate partner violence suggests that negative religious coping may result from psychiatric illness (12) . In our sample, lower negative religious coping, but not higher positive religious coping, was significantly associated with both resilient and recovered status, paralleling findings in a sample of predominantly African American veterans (15) .
Optimism
Dispositional optimism is the general tendency to hold positive expectations for the future. Optimism has been linked to lower distress and increased psychological well-being (34) . An optimistic outlook may promote resilience and recovery by enabling individuals to experience positive emotions even in the face of adversity. Positive emotions are associated with greater flexibility of thinking and exploration, while negative emotions heighten autonomic activity and narrow one’s focus of attention (35) . Dispositional optimism has also been linked to active coping, use of social supports, and lower avoidant coping (36) . These findings were also supported by our data (see correlation table in data supplement).
Coping strategies can be supported and modified with treatment interventions. In our sample, higher emotional expression was significantly associated with resilient versus currently ill status. Suppression of emotional responses is associated with increased arousal and distress (37) . In contrast, emotional processing and expression have predicted better adjustment in cancer patients (38) and fewer PTSD symptoms in African American female assault victims (39) . Free expression of emotion may facilitate habituation to stressors and harness social support. It is possible to encourage appropriate expression of emotion, with resulting lowered heart rate and negative affect (40) .
Avoidant coping has predicted poorer adjustment (41 , 42) and was associated with currently ill status in our sample. In a study of inner city African American adolescents, negative coping, including avoidance, was found to mediate the relationship between community violence exposure and higher symptom levels (14) . By contrast, studies have shown that active coping, including planning and positively reframing stressors, is associated with fewer psychological symptoms (36) . Our finding that active coping was significantly associated with recovered versus currently ill status, but not resilient versus currently ill status, may indicate that recovery is an effortful process that is distinct from resilience.
Social Support
The relationship between social support and mental health has been widely studied (36) . An individual’s ability to draw on relationships with others as a resource in times of stress is a key component of social support, which has been found to buffer against the development of PTSD (4 , 43) . In this sample, use of social support was associated with both resilience and recovery at the nearly significant level. Religious service attendance may also represent an important source of social support in this population. Studies in African American women exposed to physical and sexual assault have yielded similar findings (39 , 44) .
Posttraumatic Growth
The only factor that differentiated the resilient from the recovered group was posttraumatic growth, with higher reported growth associated with recovered status at the nearly significant level. It may be that recovered individuals are more likely than never-ill individuals to have engaged in a deep search for meaning leading to growth (45) . Of note, the absence of significant differences in psychological factors associated with resilient or recovered status suggests that some of the same mechanisms that protect individuals from developing psychiatric disorders are likely also involved in recovery.
Relationships Among Psychosocial Factors
In the sample as a whole, there were significant moderate positive correlations between psychosocial factors, for example between purpose in life and other factors, such as optimism, mastery, and several adaptive coping strategies (see data supplement). Our data suggest that in resilient individuals, a number of stable characteristics such as optimism, mastery, and purpose in life may foster adaptive coping strategies. Future studies should clarify whether improvements in adaptive coping in currently ill individuals facilitate recovery, resulting in regained feelings of mastery and a sense of purpose.
Limitations
This study has several methodological limitations that need to be addressed in future studies. First, the cross-sectional study design precludes any inferences about causality. Our findings can form the basis for future longitudinal studies. Second, owing to challenges involved in ascertaining lifetime number of traumatic events, trauma load was estimated by adding the number of lifetime trauma categories (and assessing history of assaultive trauma). Third, given the retrospective nature of the interviews, it was not possible to determine the timing of onset of psychiatric disorders with respect to the onset of one or more traumatic events; although we could not always determine if psychiatric disorders predated trauma exposure, a large percentage of currently ill and recovered patients had lifetime PTSD, which by definition is secondary to trauma. Fourth, the study of lifetime traumatic exposures precluded systematic assessment of perceived threat and dissociation (3 , 17) . Fifth, we have run a number of analyses that might have increased the likelihood of type I error, a concern tempered by the fact that psychosocial factors identified in the present study have also been associated with resilience in prior studies. Finally, we cannot determine how representative our findings are of this population.
Implications for Prevention and Treatment
A recent report released by the Institute of Medicine concluded that many treatment modalities for PTSD lack sufficient evidence of efficacy and identified a clear need for further research on treatments for trauma-exposed individuals (46) . It is our hope that further research on psychological factors identified by this and other studies will ultimately lead to the development of new types of preventive and treatment interventions. Future studies need to identify which psychosocial factors are consistently associated with resilience and determine to what extent these factors may be modifiable through clinical intervention. Longitudinal studies are needed to clarify causal pathways between resilience factors and clinical outcomes.
1. Bonanno GA: Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol 2004; 59:20–28Google Scholar
2. Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048–1060Google Scholar
3. Ozer EJ, Best SR, Lipsey TL, Weiss DS: Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull 2003; 129:52–73Google Scholar
4. Rutter M: Resilience in the face of adversity: protective factors and resistance to psychiatric disorder. Br J Psychiatry 1985; 147:598–611Google Scholar
5. Luthar SS, Cicchetti D, Becker B: The construct of resilience: a critical evaluation and guidelines for future work. Child Dev 2000; 71:543–562Google Scholar
6. Masten AS, Coatsworth JD: The development of competence in favorable and unfavorable environments: lessons from research on successful children. Am Psychol 1998; 53:205–220Google Scholar
7. Charney DS: Psychobiological mechanisms of resilience and vulnerability: implications for successful adaptation to extreme stress. Am J Psychiatry 2004; 161:195–216Google Scholar
8. Tiet QQ, Bird HR, Davies M, Hoven C, Cohen P, Jensen PS, Goodman S: Adverse life events and resilience. J Am Acad Child Adolesc Psychiatry 1998; 37:1191–1200Google Scholar
9. DuMont KA, Widom CS, Czaja SJ: Predictors of resilience in abused and neglected children grown-up: the role of individual and neighborhood characteristics. Child Abuse Negl 2007; 31:255–274Google Scholar
10. Bonanno GA, Galea S, Bucciarelli A, Vlahov D: What predicts psychological resilience after disaster? the role of demographics, resources, and life stress. J Consult Clin Psychol 2007; 75:671–682Google Scholar
11. Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P: Trauma and posttraumatic stress disorder in the community: the 1996: Detroit area survey of trauma. Arch Gen Psychiatry 1998; 55:626–632Google Scholar
12. Bradley R, Schwartz AC, Kaslow NJ: Posttraumatic stress disorder symptoms among low-income, African American women with a history of intimate partner violence and suicidal behaviors: self-esteem, social support, and religious coping. J Trauma Stress 2005; 18:685–696Google Scholar
13. Watlington CG, Murphy CM: The roles of religion and spirituality among African American survivors of domestic violence. J Clin Psychol 2006; 62:837–857Google Scholar
14. Dempsey M: Negative coping as mediator in the relation between violence and outcomes: inner-city African American youth. Am J Orthopsychiatry 2002; 72:102–109Google Scholar
15. Witvliet CVO, Phipps KA, Feldman ME, Beckham JC: Posttraumatic mental and physical health correlates of forgiveness and religious coping in military veterans. J Traumatic Stress 2004; 17:269–273Google Scholar
16. Gallup G Jr: The Religion Report: Religion in America. Princeton, NJ, Gallup Report, 1984Google Scholar
17. Brewin CR, Andrews B, Valentine JD: Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 2000; 68:748–766Google Scholar
18. Breslau N, Chilcoat HD, Kessler RC, Davis GC: Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry 1999; 156:902–907Google Scholar
19. Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM: The development of a Clinician-Administered PTSD scale. J Trauma Stress 1995; 8:75–90Google Scholar
20. First MB, Gibbon M, Spitzer RL, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders: Nonpatient Edition (SCID-I/NP). New York, Biometrics Research Department, New York State Psychiatric Institute, 1996Google Scholar
21. Alim TN, Graves E, Mellman TA, Aigbogun N, Gray E, Lawson W, Charney DS: Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. J Natl Med Assoc 2006; 98:1630–1636Google Scholar
22. Breslau N, Anthony JC: Gender differences in the sensitivity to posttraumatic stress disorder: an epidemiological study of urban young adults. J Abnorm Psychol 2007; 116:607–611Google Scholar
23. Frankl VE: Logotherapy. Isr Ann Psychiatr Relat Discip 1967:142–155Google Scholar
24. Harlow LL, Newcomb MD, Bentler PM: Depression, self-derogation, substance use, and suicide ideation: lack of purpose in life as a mediational factor. J Clin Psychol 1986; 42:5–21Google Scholar
25. Janoff-Bulman R: Shattered Assumptions: Towards a New Psychology of Trauma. New York, Free Press, 1992Google Scholar
26. Lee V, Cohen SR, Edgar L, Laizner AM, Gagnon AJ: Clarifying “meaning” in the context of cancer research: a systematic literature review. Palliat Support Care 2004; 2:291–303Google Scholar
27. Heinrichs M, Wagner D, Schoch W, Soravia LM, Hellhammer DH, Ehlert U: Predicting posttraumatic stress symptoms from pretraumatic risk factors: a 2-year prospective follow-up study in firefighters. Am J Psychiatry 2005; 162:2276–2286Google Scholar
28. Pearlin LI, Schooler C: The structure of coping. J Health Soc Behav 1978; 19:2–21Google Scholar
29. Mizell CA: Life course influences on African American men’s depression: adolescent parental composition, self-concept, and adult earnings. J Black Studies 1999; 29:467–490Google Scholar
30. Blash RR, Unger DG: Self-concept of African American male youth: self-esteem and ethnic identity. J Child and Family Studies 1995; 4:359–353Google Scholar
31. Pargament KI, Koenig HG, Perez LM: The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol 2000; 56:519–543Google Scholar
32. Myers L: Stress resolution among middle-aged black Americans, in Violence in the Black Family: Correlates and Consequences. Edited by Hampton RL. Lexington, Mass, Lexington Books, 1987, pp 237–245Google Scholar
33. Falsetti SA, Resick PA, Davis JL: Changes in religious beliefs following trauma. J Trauma Stress 2003; 16:391–398Google Scholar
34. Peterson C, Steen TA: Optimistic explanatory style, in Handbook of Positive Psychology. Edited by Snyder CR, Lopez SJ. New York, Oxford University Press, 2002, pp 244–256Google Scholar
35. Fredrickson BL: The role of positive emotions in positive psychology: the broaden-and-build theory of positive emotions. Am Psychol 2001; 56:218–226Google Scholar
36. Southwick SM, Vythilingam M, Charney DS: The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu Rev Clin Psychol 2005; 1:255–291Google Scholar
37. Mendolia M, Kleck RE: Effects of talking about a stressful event on arousal: does what we talk about make a difference? J Pers Soc Psychol 1993; 64:283–292Google Scholar
38. Stanton AL, Danoff-Burg S, Cameron CL, Bishop M, Collins CA, Kirk SB, Sworowski LA, Twillman R: Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. J Consult Clin Psychol 2000; 68:875–882Google Scholar
39. Gutner CA, Rizvi SL, Monson CM, Resick PA: Changes in coping strategies, relationship to the perpetrator, and posttraumatic distress in female crime victims. J Trauma Stress 2006; 19:813–823Google Scholar
40. Stanton AL, Kirk SB, Cameron CL, Danoff-Burg S: Coping through emotional approach: scale construction and validation. J Pers Soc Psychol 2000; 78:1150–1169Google Scholar
41. Carver CS, Pozo C, Harris SD, Noriega V, Scheier MF, Robinson DS, Ketcham AS, Moffat FL Jr, Clark KC: How coping mediates the effect of optimism on distress: a study of women with early stage breast cancer. J Pers Soc Psychol 1993; 65:375–390Google Scholar
42. Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V: Nationwide longitudinal study of psychological responses to Sept 11. JAMA 2002; 288:1235–1244Google Scholar
43. Charuvastra A, Cloitre M: Social bonds and posttraumatic stress disorder. Annu Rev Psychol 2007;Google Scholar
44. Schumm JA, Briggs-Phillips M, Hobfoll SE: Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. J Trauma Stress 2006; 19:825–836Google Scholar
45. Westphal M, Bonanno GA: Posttraumatic growth and resilience to trauma: different sides of the same coin or different coins? Applied Psychol: An Int Rev 2007; 56:417–427Google Scholar
46. Institute of Medicine: Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence. Washington, DC 2007Google Scholar