Job Performance Deficits Due to Depression
Abstract
Objective: This study assessed the relationship between depression severity and job performance among employed primary care patients. Method: In a 2001–2004 longitudinal observational study of depression’s affect on work productivity, 286 patients with DSM-IV major depressive disorder and/or dysthymia were compared to 93 individuals with rheumatoid arthritis, a condition associated with work disability, and 193 depression-free healthy control subjects. Participants were employed at least 15 hours per week, did not plan to stop working, and had no major medical comorbidities. Measures at baseline, six, 12, and 18 months included the Work Limitations Questionnaire for work outcomes, and the Patient Health Questionnaire-9 for depression. Results: At baseline and each follow-up, the depression group had significantly greater deficits in managing mental-interpersonal, time, and output tasks, as measured by the Work Limitations Questionnaire: The rheumatoid arthritis group’s deficits in managing physical job demands surpassed those of either the depression or comparison groups. Improvements in job performance were predicted by symptom severity. However, the job performance of even the “clinically improved” subset of depressed patients remained consistently worse than the control groups. Conclusions: Multiple dimensions of job performance are impaired by depression. This impact persisted after symptoms have improved. Efforts to reduce work-impairment secondary to depression are needed.
Research in community-based and primary care populations documents that depression has an adverse affect on employment, resulting in job loss, absenteeism, and “presenteeism” (reduced at-work job performance and productivity) (1 – 18) and generally an estimated national productivity cost of $44–$51 billion in U.S. dollars annually (19 , 20) . Despite these large human and economic costs, research on the work impact of depression is a topic in a nascent stage. Most available studies have included work outcomes as secondary endpoints, using samples chosen without regard to employment characteristics (e.g., baseline employment status) and omitting appropriate comparison groups. Research conducted before 2000 frequently measured work outcomes using role disability scales not specifically addressing paid employment (21) . Generally, the results of such treatment suggest that treatment can reduce the disorder’s adverse work impact and that functioning improves relatively soon after treatment is initiated (9 , 13) . Furthermore, high-quality depression detection and treatment has been shown to be superior to usual care, thus, increasing the number of days employed (9 , 10 , 12 , 13 , 17) . However, no study has used nondepressed comparison groups to judge the impact of depression on work performance.
This prospective study builds on prior research by considering job performance as its primary endpoint, including two employed comparison groups. Specifically, we 1) enrolled individuals who were working at baseline with no plans to stop working, 2) calibrated the impact of depression on work and job performance by including a group of healthy employees and one with a primarily chronic physical condition (rheumatoid arthritis, and 3) employed serial measurement of a validated multidimensional survey of health-related deficits in job performance (presenteeism).
The following questions were addressed:
What is depression’s effect on job performance within an employed population?
How do job performance deficits compare to those observed for employees with rheumatoid arthritis?
To what degree is symptom severity predictive of job performance?
Method
Study Setting and Patients
The 572 members of the study group consisted of 72 patients with DSM-IV dysthymia, 105 with DSM-IV major depressive disorder, 109 with double depression (DSM-IV major depressive disorder and dysthymia, a group of 193 healthy control subjects without major medical or psychiatric illnesses, and 93 individuals with a diagnosis of rheumatoid arthritis, including eight with comorbid depressive diagnoses. The comparison subjects were expected to have minimal job performance deficits, and the rheumatoid arthritis group was expected to have some deficits.
Between February 2001 and March 2003, the patients were recruited from the offices of primary care physicians of the Tufts Health Plan, the Fallon Clinic, and Harvard Pilgrim Health Care. Insurance from one of the health plans was not a study requirement. Eligibility criteria were being 18 to 62 years old, working for pay at least 15 hours per week, and for the depression group, a positive in-office screening result using the Primary Care Screener for Affective Disorders. Used in our prior studies, the Primary Care Screener for Affective Disorders is 87% sensitive and 95% specific (22) and has comparable diagnostic accuracy to the Prime-MD Patient Health Questionnaire-9 (23 , 24) .
Exclusions were planning to retire within 2 years, receiving disability benefits, actively alcoholic or drug-abusing, pregnant or 6 months postpartum, diagnosed with bipolar disorder, non-English speaking and/or reading, and/or diagnosed with one or more of 12 potentially disabling medical conditions (e.g., angina, congestive heart failure, stroke, diabetes, chronic obstructive lung disease). A history of alcoholism, long-term/chronic depression (those with more than four major depressive disorder episodes in their lifetime plus their diagnosis >10 years ago), anxiety, or other nonexcluded comorbid conditions were not exclusions.
The institutional review boards of all participating sites approved this study’s protocols. After complete description of the study to eligible individuals, written informed consent was obtained.
Recruitment Procedures
A multistep recruitment process was instituted. During routine office visits, patients were approached by a study representative and invited to complete self-administered prescreener forms that were electronically scanned and scored on-site. Daily, each primary care physician received a report indicating if a patient screened positive for depression. If suicidal risk was detected, the primary care physician was notified immediately. For potentially eligible patients, the primary care physician completed a brief history, noting medical contraindications to participation. Confirmation of rheumatoid arthritis was obtained from the patient’s primary care physician or rheumatologist. For the control group, a random sample of 10% of the prescreened patients was considered eligible.
Next, any remaining potentially eligible patients were mailed a baseline questionnaire, a consent form, explanatory materials, and an opt-out postcard. To assess eligibility further, an interviewer attempted to contact patients by phone and performed an in-depth screening survey. The patients declining the phone interview or who were unreachable after 10 tries were invited to complete the baseline questionnaire and consent form. An investigator then reviewed the baseline responses to assess eligibility. The telephone and/or baseline surveys included the Patient Health Questionnaire-9 (23) , which is a brief validated questionnaire for assessing current major depressive disorder and bereavement items (24) . The Patient Health Questionnaire-9 generates a DSM-IV symptom count and a depression severity score (25) .
Once eligibility was confirmed, patients were asked to complete mail surveys every 6 months for 18 months. A $20 cash incentive was provided with the baseline survey, and $10 was offered for each follow-up. A modified Dillman technique (26) encouraged responses consisting of timed phone and postcard reminders.
Outcome Indicators
Job performance deficits were measured by the Work Limitations Questionnaire, a validated self-report survey for patient and employee populations, including groups with depression (8 , 27 , 28) . In an employee sample, the relationship of Work Limitations Questionnaire scales to objectively measured work output was statistically significant for employees with and without depressive symptoms (28) . Work Limitations Questionnaire scale scores reflect the percentage of time in the prior 2 weeks the respondent had job performance deficits because of emotional and/or physical health problems. The Work Limitations Questionnaire provides information on the performance of mental-interpersonal tasks, time management, output (e.g., handling the workload and finishing work on time), and physical tasks. Its 25 items are scored on a 0% (limited none of the time) to 100% (limited all of the time) scale.
Major Independent Variables
The major independent variables were condition group (dysthymia, major depressive disorder, double depression, control, and rheumatoid arthritis), depression severity, and change in severity. Condition group was the initial assignment made at prescreening. Depressive symptom severity was based on the weighted sum of Patient Health Questionnaire-9 symptoms, according to published methodology (25) . Change in severity was defined by comparing baseline and 6-month follow-up Patient Health Questionnaire-9 scores. The first 6-month interval was used because clinical improvement is greatest during this period (29 , 30) .
Three “change” groups were defined. The “clinically improved” patients had a >50% decrease in Patient Health Questionnaire-9 severity scores (range=–4 to –19, N=48, including eight who remitted with 0–1 symptoms). Patients were the “same” if there was <50% improvement or worsening or an increase or decrease of <5 points (range –10 to 5; N=176). Patients were considered “worse” if symptom severity increased at least five points (range=6–21, N=62). Two in the “improved” group had 4-point decreases as a result of baseline scores of 7 or less. Thirty-three in the “same” group had –5 to –10 point decreases, but all had <50% improvement. In defining improvement, we chose a 50% decrease rather than an absolute reduction of –5 to be consistent with the literature (30) and so that at high scores improvement would be clinically meaningful (31) .
Patient Characteristics
Demographic characteristics included age, gender, race/ethnicity, marital status, education, and median annual income (adjusted for age, gender, and number of chronic medical conditions).
Mental health and physical health status were measured using the Short Form-12 Mental and Physical Summary Scales scores (32) ; these range from 10 (worst health) to 70 (best health). Also measured was the presence of various chronic medical conditions, a history of taking psychoactive medications, including antidepressants, number and duration of hospital visits in the past year, and number of health care visits in the past 3 months for emotional problems.
The number of jobs held since age 18, current occupation, weekly work hours, and self-employment were reported. Occupation was coded according to the six-digit 1990 Standard Occupational Classification procedure (33) , grouped into one of 23 major occupational groups with three composite categories representing 1) managers, professionals, and technicians; 2) sales, service, and support; and 3) construction, production, repairs, and transportation.
Statistical Analysis
The statistical analysis consisted of the following:
Assessing sampling bias and creating simple linear and logistic regression models comparing the characteristics of patients who enrolled with those who declined participation.
Determining the baseline comparability of enrollees, the five condition groups (dysthymia versus major depressive disorder versus double depression versus control versus rheumatoid arthritis) were compared. Regression models assessed demographic, work, and health characteristics. Baseline differences were also tested by comparing the combined depression group (dysthymia, major depressive disorder, or double depression) versus control subjects versus rheumatoid arthritis.
In a series of analyses, we measured associations with each of the dependent variables (e.g., Work Limitations Questionnaire and Patient Health Questionnaire-9 severity scores) using linear regression models with control for the independent variables of baseline age, gender, and number of chronic medical conditions. To account for multiple measurements of individuals, each model included indicator variables that represented each combination of a time point or interval and a condition group (depression, control, or rheumatoid arthritis). Models jointly estimated baseline scores and changes from baseline to later time points. These statistical models account for the serial correlations among the observations contributed by the same individual in different time points (34) . We constructed scores for follow-up surveys by adding the predicted baseline score and change from baseline. This technique avoids bias in serial changes because of the departure from the work force of individuals with poor performance. Study hypotheses were expressed in terms of linear combinations (“contrasts”) of the regression coefficients. For each test, we reported the p value, the F value across comparison groups in an omnibus test, and degrees of freedom for the associated F values. For results that were significant, we also compared the depression group with each nondepressed comparison group in a pairwise test.
Using the multivariate linear regression techniques and forming the appropriate group contrasts, we tested whether there were cross-sectional differences among the condition groups in depression severity at each study time point.
The prior models were also used to test the significance of changes in depression severity within each condition group between time points. Change scores were defined by averaging the adjusted patient changes within each group from baseline to the specific time point. To reduce the number of tests conducted, we compared the within-group change between the baseline and 6-month follow-up and performed an overall test for the trend after 6 months.
We tested the relationship between work outcomes, defined by the Work Limitations Questionnaire scales, and the type of condition. As before, each of the plotted change values involved a sum of baseline values and changes. Thus, with four outcomes and multiple condition groups, the statistical tests were carried out using an F value based on Seemingly Unrelated Regression methods because baseline scores and changes, as well as the four outcome measures, were statistically correlated (34) .
To assess whether the effect of depression on work outcomes differed among certain depression subgroups, we tested whether Work Limitations Questionnaire scales (cross-sectionally and longitudinally) were predicted by clinical improvement from depression. In these models, we included an indicator variable to contrast the “clinically improved” depression subgroup to the control subjects (again limiting the number of tests). The testing methods used were the same as for the prior step. Stata 7.0 (35) was used for all analyses.
Results
A total of 14,268 patients completed the prescreener questionnaire, and 1,909 (13%) were eligible for further screening ( Figure 1 ). Of these, 646 (34%) declined to participate in the screening or had inaccurate contact information (supplied by the primary care physician’s office), 437 (23%) were ineligible based on physician reports, and 826 (43%) were fully screened. Of these, 681 (82%) were confirmed eligible and 145 (18%) were ineligible. Of the 681 confirmed eligible patients, 109 (16%) declined to participate, and 572 (84%) enrolled (depression group=286, rheumatoid arthritis group=93, control group=193). Most follow-up administrations were completed (1,454 of 1,716 or 84.7%). The attrition rate was 9%.
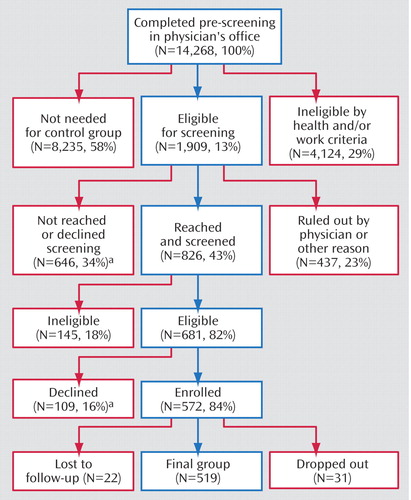
a Effective refusal rate=(646+109)/1,909 or 39.4%.
There were no statistically significant differences between enrolled patients and patients who declined to participate with regard to prescreener employment status, Mental and Physical Component Summary scores, number of dysthymia or major depressive disorder symptoms, or comorbid diagnoses (p>0.05). The latter group was younger (39.0 versus 41.5 years; F=7.33, df=1, 604, p<0.01) and contained more men than women (38% versus 21%, F=21.33, df=1, 607, p<0.01).
Baseline Characteristics
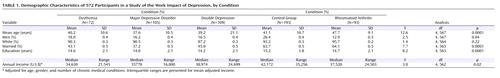
Of the 572 enrolled participants, 81% were women (N=461); 92% were white (N=521); 51% held professional, technical, and managerial occupations (N=292); 42% were in sales, support, and service occupations (N=237); and 7% were in production, construction, repairs, and transportation occupations (N=40). (Data not shown and were missing for three participants) ( Table 1 ). Mean weekly work hours were 38.6 (SD=–0.5). Few participants (N=40, 9.3%) were self-employed.
When we compared the combined depression group versus the control subjects versus the rheumatoid arthritis group, there were differences in age (F=23.7, df=2, 569, p<0.0001), marital status (F=14.7, df=2, 565, p<0.0001), education (F=14.2, df=2, 565, p<0.0001), and annual median income (F=3.2, df=2, 564, p=0.04). The depression group ( Table 1 ) was youngest, included fewer married individuals, was less educated, earned less, and held more jobs since age 18 (7.0 versus 5.9 versus 6.1).
The three groups differed on Mental Component Summary 12 (F=318.0, df=2, 569, p<0.0001) and Physical Component Summary 12 scores (F=30.3, df=2, 569, p<0.0001), with the depressed group having the poorest health and with regard to the number of visits for emotional problems (F=17.1, df=2, 520, p<0.0001). The depression group had three times as many health care visits. Few patients reported that their primary care physicians had ever asked about work issues (dysthymia, 28%; major depressive disorder, 32%; double depression, 23%; rheumatoid arthritis, 26%, versus control subjects, 10%; F=6.4, df=4, 559, p<0.0001), or advised them to change their work (20%/19%/17%/20% versus 7%; F=3.5, df=4, 560, p=0.008).
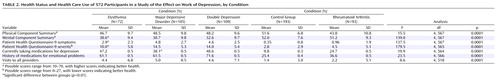
Depression-Specific Baseline Characteristics
At the time of screening, 25% of the depression group met the screening criteria for dysthymia (N=72), and 75% met criteria for major depressive disorder (major depressive disorder (N=105) and double depression (N=109) ( Table 2 ). By baseline, the mean number of symptoms was 2.9 for the dysthymia group, 4.8 for major depressive disorder, and 4.6 for double depression. Also, baseline Patient Health Questionnaire-9 severity scores were 10.0, 14.5, and 14.0, respectively, for the three depression groups (F=18.1, df=1, 282, p<0.0001 for dysthymia versus major depressive disorder and double depression). Two-thirds of all depressed patients had previously taken medication for an emotional problem (N=187), and 44% (N=127) were taking antidepressants at baseline. The use of health care providers was similar whether patients were currently taking an antidepressant or not (data not shown).
Cross-Sectional and Longitudinal Depression Severity
In cross-sectional pairwise comparisons of Patient Health Questionnaire-9 depression severity scores, the combined depression group was worse than the control group: baseline difference (F=606.6, df=1, 569, p<0.0001); 6 month difference (F=262.3, df=1, 569, p<0.0001); 12-month difference (F=233.3, df=1, 569, p<0.0001); and 18-month difference (F=167.2, df=1, 569, p<0.0001). Cross-sectional comparisons contrasting the depression and rheumatoid arthritis groups demonstrated significant differences in Patient Health Questionnaire-9 severity scores (F=169.0, df=1, 569, p<0.0001); 6-month difference (F=73.9, df=1, 569, p<0.0001); 12-month difference (F=109.8, df=1, 569, p<0.0001); and 18-month difference (F=67.5, df=1, 569, p<0.0001) ( Figure 2 ).
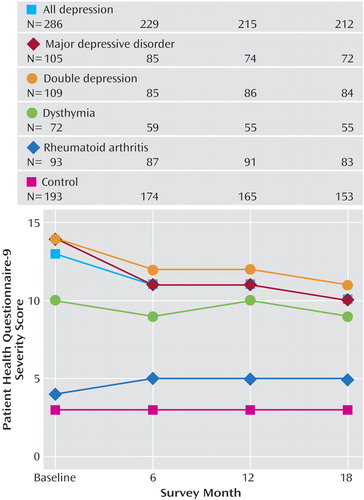
a Adjusted for age, gender, and number of chronic conditions.
Between baseline and 6-month follow-up, the combined depression group experienced a significant decline in severity (F=7.7, df=1, 569, p<0.01). Severity declined further between the 6-month and 18-month follow-up (F=4.2, df=1, 569, p=0.02). Between baseline and 6 months, 17% of the depression group (N=48, Patient Health Questionnaire-9 severity: mean=3.9) was clinically improved, 61% (N=176, Patient Health Questionnaire: mean=11.2) was the same, and 22% (N=62, Patient Health Questionnaire-9=18.4) worsened. By 18 months, of the 212 subjects with completed Patient Health Questionnaire-9 scores at all time points, 45 (21%) had remitted (0–1 symptoms).
Job Performance Deficits
According to Work Limitations Questionnaire scores, the depression group had significantly greater job performance deficits at each time point than the control or the rheumatoid arthritis groups ( Figure 3 ). There were significant differences with regard to performing mental-interpersonal tasks (baseline: F=141.7; 6 months: F=39.0; 12 months: F=34.8; 18 months: F=39.0; all df=2, 560, p<0.0001), time management (baseline: F=94.7; 6 months: F=35.6; 12 months: F=23.4; 18 months: F=26.4, all df=2, 556, p<0.0001), output tasks (baseline: F=99.0; 6 months: F=27.7; 12 months: F=25.0; 18 months: F=20.9, all df=2, 558, p<0.0001), and physical tasks (baseline: F=25.4, 6 months: F=13.1; 12 months: F=18.5; 18 months: F=21.6, all df=2, 556, p<0.0001). In pairwise comparisons of the combined depression versus control groups, job performance was more impaired (mental-interpersonal baseline: F=238.5; 6 months: F=77.9; 12 months: F=65.6; 18 months: F=76.8; all=df 1, 560, p<0.0001; time management baseline: F=189.4; 6 months: F=62.9; 12 months: F=46.1; 18 months: F=51.1, all df=1, 556, p<0.0001; output baseline: F=194.8; 6 months: F=52.3; 12 months: F=45.0; 18 months: F=41.8, all df=1, 558, p<0.0001; and physical tasks baseline: F=17.5; 6 months: F=7.3; 12 months: F=19.6; 18 months: F=16.7, all df=1, 556, p<0.0001). However, in a pairwise comparison of the combined depression group and rheumatoid arthritis, performance of physical tasks was worse in the latter group at 6 and 18 months (6 months: F=6.8; 18 months: F=6.7, both df=1, 556, p=0.01; baseline: F=1.8; 12 months: F=1.7, both df=1, 556, p=0.20).
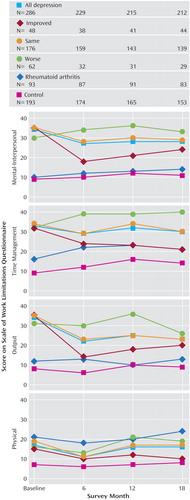
a Adjusted for age, gender, and number of chronic conditions.
We assessed temporal changes in job performance among depression group subjects defined as clinically improved, the same, or worse. Between baseline and 6 months, job performance deficits declined significantly in the “clinically improved” group according to three of the four Work Limitations Questionnaire scales (mental-interpersonal: F=19.7, df=1, 560, p<0.0001; time: F=4.1, df=1, 556, p=0.04; output: F=21.3, df 1, 558, p<0.0001). Patients in the “same” severity group had significantly improved job performance (between baseline and 6 months) on each of the four Work Limitations Questionnaire scales (mental-interpersonal: F=11.6, df=1, 560, p<0.001; time management: F=5.0, df=1, 556, p=0.03; output: F=19.2, df=1, 558, p<0.0001; and physical: F=0.8.7, df=1, 556, p<0.01). Within this time period, patients in the “worse” severity subgroup had no significant changes in any scale scores.
Between the 6-month and 18-month follow-up intervals, job performance did not change significantly for any of the three severity depression groups, except in one instance. Deficits in performing physical job tasks increased significantly in the “same” severity group (F=4.3, df=1, 556, p=0.01) ( Figure 3 ).
Changes in depression severity and job performance were significantly positively correlated. For example, a 1.0-point decrease in depression severity was associated with a 1.2-point improvement in performing mental-interpersonal tasks (t=12, df=989, p<0.0001). However, comparisons of the combined depression group versus the control groups indicated that clinical improvement does not result in full recovery of job performance. Although the control group experienced an increase in deficits in performing mental-interpersonal tasks and time management, the job performance deficits even in the clinically improved group were greater at baseline and 18 months. These deficits affected performance of mental-interpersonal job tasks (baseline: F=77.4 and 18 months:: F=24.3, df=1, 560, p<0.001) and output tasks (baseline: F=51.6 and 18 months: F=6.9, df=1, 558, p<0.001).
Discussion
This is the first study to our knowledge to longitudinally assess the impact of depression on job performance among employed primary care patients relative to two comparison groups. The control group provided a benchmark for relatively healthy employees; the rheumatoid arthritis group was the benchmark for a group vulnerable to work disabilities. Compared to the other two groups, the depression group had persistent, multidimensional deficits. Moreover, while symptom improvement correlates with better job performance, depressed patients meeting the criteria for clinical improvement still perform worse than healthy control subjects.
These results have several intervention implications. First, guideline-concordant pharmacological and psychotherapeutic treatment of depression should be pursued as a strategy to maximize remission rates. In this usual care study, few (21%) of the depressed patients achieved Patient Health Questionnaire-9 symptom remission scores by the end of the study. That 44% of the depressed group was taking antidepressants at baseline yet met criteria for clinical depression indicates how important it is to ensure close monitoring of treatment. The literature on guideline-concordant depression care indicates that many individuals with depression do not have a remitted illness or a relapse within the first year of treatment, and those that improve frequently experience a lag time to treatment response (29 , 30) .
Second, physicians need to inquire about the impact of depression on work and monitor the impact of symptom reduction on recovery of work function. Although it is possible that ideal depression treatment may have led to a larger number of employees whose illness remitted, it is unclear whether work outcomes would approximate those of the healthy control subjects.
Third, the results suggest that patients with depression may benefit from work-focused interventions. These interventions may help patients address barriers to effective functioning. The Work Limitations Questionnaire scores provide insight into interventions that may help. Specifically, we found that there were deficits on performance of mental-interpersonal, time management, output, and physical tasks. Thus, depressed patients may benefit from learning new approaches to managing job demands, and identifying workplace supports such as Employee Assistance Programs or worksite occupational health clinics. It may also be worthwhile to adapt job retention techniques currently used within employment programs for severely and chronically mentally ill individuals (36 – 38) .
This study had limitations. First, by defining entrance into the study by a high level of depression symptoms (75% met criteria for current major depressive disorder), there could be selection or ascertainment bias. Thus, symptom improvement in the initial period may be overstated, and we may have selected individuals with higher initial work impairment. Despite informing patients that this was an observational study, participants had poorer social role functioning on the prescreener than those declining or excluded. Results may also not generalize beyond a primary care population to a community-based population (e.g., worksite-based samples) who use less health care in general. Third, because more depressed respondents became unemployed and/or dropped-out of the study (7% versus 4% for the control groups), study results may underestimate job performance limitations. Finally, this study did not measure the work impact of antidepressants. Participants were considered to have depression treatment if they reported using an antidepressant or a recent visit to a health care provider for an emotional problem.
The reality of impaired job performance suggests that, in addition to quality medical care for their persistent depressive symptoms, employees with depression may benefit from other services. There is more research to be performed. Testing of interventions focusing on supporting depressed employees’ on-the-job performance is urgently needed.
1. Berndt ER, Finkelstein SN, Greenberg PE, Howland RH, Keith A, Rush AJ, Russell J, Keller MB: Workplace performance effects from chronic depression and its treatment. J Health Econ 1998; 17:511–535Google Scholar
2. Broadhead WE, Blazer DG, George LK, Tse CK: Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA 1990; 264:2524–2528Google Scholar
3. Goetzel RZ, Hawkins K, Ozminkowski RJ, Wang S: The health and productivity cost burden of the “top 10” physical and mental health conditions affecting six large U.S. employers in 1999. J Occup Environ Med 2003; 45:5–14Google Scholar
4. Kessler RC, Barber C, Birnbaum HG, Frank RG, Greenberg PE, Rose RM, Simon GE, Wang P: Depression in the workplace: effects on short-term disability. Health Aff 1999; 18:163–171Google Scholar
5. Kessler RC, Greenberg P, Mickelson K, Meneades LM, Wang PS: The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med 2001; 43:218–225Google Scholar
6. Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS: The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 2003; 289:3095–3105Google Scholar
7. Kroenke K, West SL, Swindle R, Gilsenan A, Eckert GJ, Dolor R, Stang P, Zhou XH, Hays R, Weinberger M: Similar effectiveness of paroxetine, fluoxetine, and sertraline in primary care: a randomized trial. JAMA 2001; 286:2947–2955Google Scholar
8. Lerner D, Amick BC III, Lee JC, Rooney T, Rogers WH, Chang H, Berndt ER: Relationship of employee-reported work limitations to work productivity. Med Care 2003; 41:649–659Google Scholar
9. Mintz J, Mintz L, Aruda M, Hwang S: Treatments of depression and the functional capacity to work. Arch Gen Psychiatry 1992; 49:761–768Google Scholar
10. Rost K, Smith JL, Dickinson M: The effect of improving primary care depression management on employee absenteeism and productivity: a randomized trial. Med Care 2004; 42:1202–1210Google Scholar
11. Schoenbaum M, Unutzer J, Sherbourne C, Duan N, Rubenstein LV, Miranda J, Meredith LS, Carney MF, Wells K: Cost-effectiveness of practice-initiated quality improvement for depression: results of a randomized controlled trial. JAMA 2001; 286:1325–1330Google Scholar
12. Schoenbaum M, Unutzer J, McCaffrey D, Duan N, Sherbourne C, Wells KB: The effects of primary care depression treatment on patients’ clinical status and employment. Health Serv Res 2002; 37:1145–1158Google Scholar
13. Simon GE, Revicki D, Heiligenstein J, Grothaus L, Von Korff M, Katon WJ, Hylan TR: Recovery from depression, work productivity, and health care costs among primary care patients. Gen Hosp Psychiatry 2000; 22:153–162Google Scholar
14. Spitzer R, Kroenke K, Linzer M, Hahn S, Williams J, de Gruy F, Brody D, Davies M: Health-related quality of life in primary care patients with mental disorders: results from the PRIME-MD 1000 study. JAMA 1995; 274:1511–1517Google Scholar
15. Von Korff M, Ormel J, Katon W, Lin EHB: Disability and depression among high utilizers of health care. Arch Gen Psychiatry 1992; 49:91–100Google Scholar
16. Wang PS, Beck AL, Berglund P, McKenas DK, Pronk NP, Simon GE, Kessler RC: Effects of major depression on moment-in-time work performance. Am J Psychiatry 2004; 161:1885–1891Google Scholar
17. Wells KB, Sherbourne C, Schoenbaum M, Duan N, Meredith L, Unutzer J, Miranda J, Carney MF, Rubenstein LV: Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA 2000; 283:212–220Google Scholar
18. Zhang M, Rost KM, Fortney JC, Smith GR: A community study of depression treatment and employment earnings. Psychiatr Serv 1999; 50:1209–1213Google Scholar
19. Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, Corey-Lisle PK: The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry 2003; 64:1465–1475Google Scholar
20. Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D: Cost of lost productive work time among US workers with depression. JAMA 2003; 289:3135–3144Google Scholar
21. Wells KB, Stewart A, Hays RD, Burnam A, Rogers W, Daniels M, Berry S, Greenfield S, Ware J: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 1989; 262:914–919Google Scholar
22. Rogers WH, Wilson IB, Bungay KM, Cynn DJ, Adler DA: Assessing the performance of a new depression screener for primary care (PC-SAD). J Clin Epidemiol 2002; 55:164–175Google Scholar
23. Spitzer RL, Williams JB, Kroenke K, Linzer M, de Gruy FV III, Hahn SR, Brody D, Johnson JG: Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA 1994; 272:1749–1756Google Scholar
24. Spitzer RL, Kroenke K, Williams JB: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study: primary care evaluation of mental disorders: Patient Health Questionnaire. JAMA 1999; 282:1737–1744Google Scholar
25. Kroenke K, Spitzer RL, Williams JB: The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613Google Scholar
26. Dillman DA: Mail and Telephone Surveys: The Total Design Method. New York, John Wiley, 1978Google Scholar
27. Lerner D, Adler DA, Chang H, Lapitsky L, Hood MY, Perissinotto C, Reed J, McLaughlin TJ, Berndt ER, Rogers WH: Unemployment, job retention, and productivity loss among employees with depression. Psychiatr Serv 2004; 55:1371–1378Google Scholar
28. Lerner D, Amick BC III, Rogers WH, Malspeis S, Bungay K, Cynn D: The work limitations questionnaire. Med Care 2001; 39:72–85Google Scholar
29. American Psychiatric Association: Practice Guideline for the Treatment of Patients With Major Depressive Disorder. Am J Psychiatry 2000; 157:1–45Google Scholar
30. Depression Guidelines Panel: Depression in Primary Care: Volume 2: Treatment of Major Depression: Clinical Practice Guidelines Number 5. Rockville, Md, Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, 1993Google Scholar
31. Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K: Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Med Care 2004; 42:1194–1201Google Scholar
32. Ware JE Jr, Kosinski M, Keller SD: SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales, 2nd Ed. Boston, the Health Institute, New England Medical Center, 1995Google Scholar
33. US Department of Labor: Standard Occupational Classification. http://www.bls.gov/oes/2001/oes_nat.htmGoogle Scholar
34. Greene WH: Systems of Regression Equations in Econometric Analysis. New York, MacMillan, 1993Google Scholar
35. Stata Reference Manual, Volume 1 A–G, 7th Ed. College Station, Tex, Stata Press, 2001Google Scholar
36. Handler J, Doel K, Henry A, Lucca A: Implementing supportive employment services in a real world setting. Psychiatr Serv 2003; 54:960–962Google Scholar
37. Kopelowicz A, Liberman RP: Integrating treatment with rehabilitation for persons with major mental illnesses. Psychiatr Serv 2003; 54:1491–1498Google Scholar
38. Lehman AF, Goldberg R, Dixon LB, McNary S, Postrado L, Hackman A, McDonnell K: Improving employment outcomes for persons with severe mental illnesses. Arch Gen Psychiatry 2002; 59:165–172Google Scholar