Predictors of 2-Year Outcome for Patients With Borderline Personality Disorder
Abstract
Objective: The primary purpose of this report was to investigate whether characteristics of subjects with borderline personality disorder observed at baseline can predict variations in outcome at the 2-year follow-up. Method: Hypothesized predictor variables were selected from prior studies. The patients (N=160) were recruited from the four clinical sites of the Collaborative Longitudinal Personality Disorders Study. Patients were assessed at baseline and at 6, 12, and 24 months with the Structured Clinical Interview for DSM-IV Axis I Disorders; the Diagnostic Interview for DSM-IV Personality Disorders, a modified version of that instrument; the Longitudinal Interval Follow-Up Evaluation; and the Childhood Experiences Questionnaire–Revised. Univariate Pearson’s correlation coefficients were calculated on the primary predictor variables, and with two forward stepwise regression models, outcome was assessed with global functioning and number of borderline personality disorder criteria. Results: The authors’ most significant results confirm prior findings that more severe baseline psychopathology (i.e., higher levels of borderline personality disorder criteria and functional disability) and a history of childhood trauma predict a poor outcome. A new finding suggests that the quality of current relationships of patients with borderline personality disorder have prognostic significance. Conclusions: Clinicians can estimate 2-year prognosis for patients with borderline personality disorder by evaluating level of severity of psychopathology, childhood trauma, and current relationships.
This report investigates baseline characteristics of subjects with borderline personality disorder to determine whether they can predict variations in outcome 2 years later. It takes place within the context of a series of prior studies characterized by use of widely divergent predictor variables, often assessed retrospectively, and, if prospectively, without established reliability. This study uses data from the Collaborative Longitudinal Personality Disorders Study (1) . Its data set provides a sizable group of carefully diagnosed subjects with borderline personality disorder from a wide range of clinical settings from whom data were prospectively collected and analyzed with a repeated-measures design.
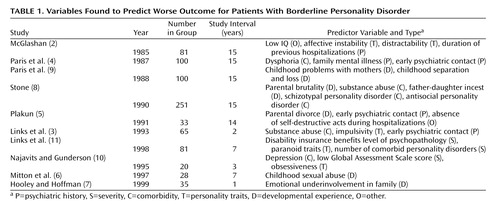
Predictive variables identified in prior studies of patients with borderline personality disorder are summarized in Table 1 . Psychiatric history variables found to be predictive are length of previous hospitalizations (2) and early age of psychiatric contact (3 – 5) . Developmental experiences predictive of poor outcome include childhood abuse (6) , parental underinvolvement (7) , father-daughter incest (8) , parental divorce (5) , parental brutality (8), childhood separations or losses (9) , and disturbed maternal relationships (9) . Predictor variables within presenting phenomenology traits are of three subtypes: severity, comorbidity, and personality. Severity variables previously reported to predict poor outcome include low Global Assessment Scale (GAS) scores (10) , a greater number of bipolar disorder criteria met, and a greater number of axis II diagnoses present at follow-up (11) . Comorbidity variables found to be predictive of poor outcome include substance abuse (3 , 8) and depression (10) or “dysphoria” (4) . Comorbid personality predictor variables of poor outcome include those related to personality disorders—i.e., schizotypal (8) , antisocial (8) , and paranoid (11) —and of better outcome, such as obsessive-compulsive personality disorder (10) . Personality trait variables that predict outcome are impulsivity (3) and affective instability (2) .
When our assessment battery permitted, we tested whether the variables found to predict outcome in prior studies were replicated. We also tested four variables not represented by prior research. We added posttraumatic stress disorder (PTSD) to our comorbidity variables because of its connection to childhood abuse or neglect (12) . The three other additions were personality trait variables that represent probable phenotypic traits of borderline personality disorder—affective, impulsive, and interpersonal—that have been identified by factor analytic studies (13 – 16) with support from family history (17 , 18) and attachment (19) studies.
Method
Subjects
The overall Collaborative Longitudinal Personality Disorders Study aims, background, design, methods, and group characteristics are detailed elsewhere (1 , 20) . In brief, this was a repeated-measures prospective study in which treatment-seeking subjects who met criteria for one of the four personality disorders were compared to subjects with major depressive disorder without personality disorder to examine stability, interactions with axis I disorders, alternative classification systems, and prognostic factors. This report focuses on the predictors for 160 subjects with borderline personality disorder (from our baseline group of 175 subjects) for whom 2-year outcome data were available. This subgroup of subjects with borderline personality disorder, derived from a wide range of psychiatric services, was 75% female and 71% Caucasian and was distributed evenly by socioeconomic status and was between ages 18 and 45 (1) .
Procedures
All participants signed written informed consent. Clinically experienced research assistants interviewed subjects who screened positive for borderline personality disorder (or the other study diagnostic groups) with the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P) (21) and the Diagnostic Interview for DSM-IV Personality Disorders (22) . Convergent support of the Diagnostic Interview for DSM-IV Personality Disorders diagnosis of borderline personality disorder was required by either the self-reported Schedule for Nonadaptive and Adaptive Personality (23) or an independent clinician-rated Personality Assessment Form (24) . The participants were interviewed at 6, 12, and 24 months after the baseline assessment. The course of the group was assessed with 1) a modified version of the Diagnostic Interview for DSM-IV Personality Disorders (the Diagnostic Interview for DSM-IV Personality Disorders Follow-Along Version), which provided monthly ratings of the borderline personality disorder criteria, and 2) the Longitudinal Interval Follow-Up Evaluation (25) for assessment of axis I disorders, social relationships, and other domains of functioning.
Assessment Instruments
The Diagnostic Interview for DSM-IV Personality Disorders is a semistructured diagnostic interview for the assessment of all DSM-IV personality disorders (22) . Each of the criteria for all disorders is assessed with one or more questions, which are then rated on a 3-point scale (0=not present, 1=present but of uncertain clinical significance, and 2=present and clinically significant). The Diagnostic Interview for DSM-IV Personality Disorders requires that the criteria be present and pervasive for at least 2 years and that it be characteristic of the person for most of his or her adult life to be counted toward a diagnosis. In the present study, the interrater reliability for borderline personality disorder, based on 84 pairs of raters, was kappa=0.68. The test-retest reliability, based on 52 cases, was kappa=0.69 (26) .
The Diagnostic Interview for DSM-IV Personality Disorders was used to assess the following predictor variables measuring baseline severity: 1) the number of borderline personality disorder criteria, and 2) the number of other personality disorder criteria. It was also used to assess the three component personality traits as defined by combining criteria whose groupings have been shown to be familial (18) , i.e., affect dysregulation (affective instability, emptiness, and anger), behavioral dyscontrol (impulsivity and self-injurious behavior), and interpersonal instability (intense unstable relationships and efforts to avoid abandonment).
The Diagnostic Interview for DSM-IV Personality Disorders Follow-Along Version was used to determine criteria-based outcome. It provided a record of the presence of borderline personality disorder criteria for each month of the follow-up period. Reliability for retrospective reporting on the Diagnostic Interview for DSM-IV Personality Disorders Follow-Along Version was found to be good, with kappa scores ranging from 0.68 to 0.78 for individual personality disorders.
The SCID-P is a diagnostic interview that assesses current and lifetime axis I psychiatric disorders (21) . In the current study, kappa coefficients for interrater reliability for axis I disorders ranged from 0.57 to 1.00, with a median kappa of 0.76. Test-retest reliability ranged from 0.35 to 0.78, with a median kappa of 0.64 (26) . The SCID-P was used at study intake to measure severity variables (Global Assessment of Functioning [GAF] Scale score and the number of axis I disorders) and axis I comorbidity variables (PTSD and alcohol or substance abuse and dependence).
The Longitudinal Interval Follow-Up Evaluation is a semistructured interview rating system with demonstrated reliability for assessing the longitudinal course of axis I mental disorders (25) . In addition, the Longitudinal Interval Follow-Up Evaluation assesses the nature and quantity of all forms of treatment received and provides specific scales for rating impairment in relationships with parents, spouse, siblings, and children. These monthly ratings are combined to give an overall scale score on the quality of the patients’ relationships to all others in their family during the follow-up period.
The Childhood Experiences Questionnaire–Revised is a semistructured interview that assesses a variety of developmental adversities, including experiences of neglect and abuse (27) . It has excellent interrater reliability, with kappas that range from 0.64 to 1.00 and a median kappa of 0.88 (27) . The Childhood Experiences Questionnaire–Revised was included to measure the historical predictor variables of childhood abuse and neglect.
Data Analysis
For the purposes of this report, outcome was defined by two different methods. One method involved the level of borderline personality disorder psychopathology, and the other involved the level of functional impairment. The first method used a definition of outcome based on the mean number of borderline personality disorder criteria in the 6 months before the 2-year assessment (number of criteria for months 19–24: mean=3.97, SD=2.47). The second method used the average GAF Scale score during the 6 months before the 2-year assessment (GAF Scale score for months 19–24: mean=53.72, SD=11.29). These two outcome measures were negatively correlated (r=–0.48, p<0.0001). Although correlated, these measures of outcome have significant independent variances as demonstrated by other analyses from the Collaborative Longitudinal Personality Disorders Study data set (28 , 29) .
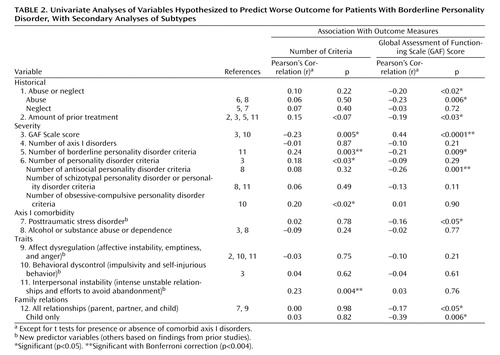
Univariate Pearson’s correlation coefficients were calculated on 12 primary predictor variables ( Table 2 ). Because these variables are hypothesis driven, the need for a multiple test adjustment (i.e., Bonferroni correction) was arguable (30 , 31) . Nonetheless, to distinguish findings from our analyses that would bear stern statistical critique, we identified the variables remaining significant with Bonferroni correction (p<0.004). For the variables that proved to be significant predictors of outcome, we then decomposed the variables into their components (i.e., rather than simply looking at the overall number of personality disorder criteria, we looked at the more specific types of personality disorder criteria, such as antisocial, schizotypal, and obsessive-compulsive personality disorder). This allowed us to examine whether more discrete features could account for the variance in outcome; however, the p values for these tests could be inflated because of the risk of capitalization on chance.
Finally, two forward stepwise regression models were tested. These included all of the variables in our univariate correlations that were predictive of either of our two outcome measures (number of borderline personality disorder criteria or the GAF Scale score). These analyses were conducted to select the best subset of predictor variables with control for redundant variance. These analyses did not, however, override the results from the univariate analyses because some of our predictor variables were correlated with each other, and minor differences in apparent strength of association could substantially alter which variables were included in the final regression model.
Results
As shown in Table 2 , the results of our univariate analyses demonstrated that five of the hypothesized predictor variables were significantly related to criteria-based outcomes at the p<0.05 level, and nine were significantly related to outcomes based on the GAF Scale score at the p<0.05 level. The variables that predicted poorer criteria-based outcomes were the GAF Scale score at baseline, the number of borderline personality disorder criteria, the total number of personality disorder criteria, and the unstable interpersonal relationship trait. In secondary analyses of personality disorder criteria, a negative effect of more obsessive-compulsive criteria was found to be significant but not the expected negative effect of antisocial, schizotypal, or paranoid criteria. The variables that predicted poorer outcomes based on the GAF Scale score were childhood abuse or neglect, the amount of treatment received before baseline, the GAF Scale score at baseline, poor family relationships, the number of schizotypal personality disorder or personality disorder criteria, and the comorbidity of PTSD. In secondary analyses, the abuse component of abuse and neglect, the number of antisocial personality disorder criteria component of the total number of personality disorder criteria, and the relationship to children component of family relationships were significant predictors.
For the two stepwise regression models, the predictor variables from univariate analyses were joined by gender, race, age, and site as covariates. In our first model, which predicted psychopathology (i.e., criteria-based) outcome, we found that the low GAF Scale score (beta=–0.05, p<0.03) and more obsessive-compulsive personality disorder criteria (beta=0.25, p<0.04) were the only two significant variables that predicted poor outcome. In the second model, which predicted functional outcome (i.e., GAF Scale score), greater total number of personality disorder criteria was the only significant variable (beta=–0.41, p<0.005).
Discussion
The clearest and strongest finding from this study was that the greater the severity of the level of dysfunction and psychopathology at baseline of the subjects with borderline personality disorder, the worse their outcome. Measures of severity also emerged in both of the multiple regression analyses, which, although they confirmed the importance of severity, did not diminish the significance of the variables found through univariate analyses. The overriding importance of severity as a predictor found here replicates a finding reported by Links et al. (3 , 11) .
Our finding that an early history of abuse and neglect is associated with a poor prognosis echoes prior reports. Of note, abuse emerged as the more important component. This finding expands on the study by Stone (8) that identified specific types of abuse as predictors of borderline personality disorder, i.e., father-daughter incest and parental brutality.
Perhaps the most interesting but difficult findings to interpret are that the three variables reflecting the quality of the borderline patients’ relationships—i.e., the trait of interpersonal instability, current family relationships, and relationship with children—were each predictive of outcome. However, because our measure of the borderline personality disorder interpersonal trait is composed of two of the nine DSM-IV borderline personality disorder criteria, its correlation with the number of borderline personality disorder criteria at outcome is partly circular. Similarly, because functioning within family relationships is a component of the GAF Scale scoring, this finding, too, is partially circular. The third relationship variable that emerged from a secondary analyses is that for the borderline patients who are parents, the quality of their relationships with their children (i.e., whether good or poor) are prognostically significant. This is consistent with clinical reports that some patients with borderline personality disorder find motherhood a source of self-esteem and security, whereas others can be immobilized by the conflicts related to nurturing or disciplining their children (32 , 33) . Overall, although the predictive strength of our interpersonal relationship findings is unclear, they do suggest that assessing the quality of relationships can help in estimating a prognosis for patients with borderline personality disorder. This suggestion is consistent with treatment strategies that try to effect changes in troubling relationships with an expectation that this can improve the prognosis.
Some predictor variables found in prior reports were not assessed in the present report. Most notably, our data set did not include assessments of age of first psychiatric contact or number of prior hospitalizations. We could look at a related variable, i.e., amount of prior treatment, and by finding that it predicted functional outcome, we did indirectly confirm those predictors. One prior predictor variable that we evaluated, i.e., impulsivity, found surprisingly modest support whether measured by comorbid antisocial personality disorder or alcohol or substance abuse or as a borderline personality disorder behavioral component trait. On the other hand, the number of antisocial personality disorder criteria did predict functional outcome. The relative weakness of impulsivity as a predictor in this study may be due to our use of improved methodology, i.e., reliable and prospective assessments, or, conversely, it may be because prior studies that supported the prognostic significance of impulsivity had much longer periods of follow-up (3 , 8) . Examination with subsequent longer-term data from the Collaborative Longitudinal Personality Disorders Study will help clarify this.
In conclusion, our findings indicate that in developing a 2-year prognosis for patients with borderline personality disorder, assessments of severity, both symptomatic (i.e., criterion) and functional (i.e., the GAF Scale score), are most important. Our findings also suggest that a thorough examination of the present relationships and past relational history of patients with borderline personality disorder, specifically a history of early childhood maltreatment, may add to estimates of the expected prognosis. Implications for future research include the need for replications of studies of borderline personality disorder—a point underscored by our inconsistent replication of findings from prior studies—and the need to test the significance of these 2-year findings with follow-ups that assess a longer-term course.
1. Gunderson JG, Shea MT, Skodol AE, McGlashan TH, Morey LC, Stout RL, Zanarini MC, Grilo CM, Oldham JM, Keller MB: The Collaborative Longitudinal Personality Disorders Study: development, aims, design, and sample characteristics. J Personal Disord 2000; 14:300–315Google Scholar
2. McGlashan TH: Prediction of outcome in borderline personality disorder, in The Borderline: Current Empirical Research. Edited by McGlashan TH. Washington, DC, Psychiatric Press, 1985, pp 61–98Google Scholar
3. Links PS, Mitton JE, Steiner M: Stability of borderline personality disorder. Can J Psychiatry 1993; 38:255–259Google Scholar
4. Paris J, Brown R, Nowlis D: Long-term follow-up of borderline patients in a general hospital. Compr Psychiatry 1987; 28:530–535Google Scholar
5. Plakun EM: Prediction of outcome in borderline personality disorder. J Personal Disord 1991; 5:93–101Google Scholar
6. Mitton MJE, Links PS, Durocher G: A history of childhood sexual abuse and the course of borderline personality disorder, in Role of Sexual Abuse in the Etiology of Borderline Personality Disorder. Edited by Zanarini MC. Washington, DC, American Psychiatric Press, 1997, pp 181–202Google Scholar
7. Hooley JM, Hoffman PD: Expressed emotion and clinical outcome in borderline personality disorder. Am J Psychiatry 1999; 156:1557–1562Google Scholar
8. Stone MH: The Fate of Borderline Patients. New York, Guilford, 1990Google Scholar
9. Paris J, Nowlis D, Brown R: Developmental factors in the outcome of borderline personality disorder. Compr Psychiatry 1988; 29:147–150Google Scholar
10. Najavits LM, Gunderson JG: Better than expected: improvements in borderline personality disorder in a 3-year prospective outcome study. Compr Psychiatry 1995; 36:296–302Google Scholar
11. Links PS, Heslegrave R, Vanreekum R: Prospective follow-up study of borderline personality disorder: prognosis, prediction of outcome, and axis II comorbidity. Can J Psychiatry 1998; 43:365–270Google Scholar
12. Gunderson JG, Chu JA: Treatment implications of past trauma in borderline personality disorder. Harv Rev Psychiatry 1993; 1:75–81Google Scholar
13. Clarkin JF, Hull JW, Hurt SW: Factor structure of borderline personality disorder criteria. J Personal Disord 1993; 7:137–143Google Scholar
14. Sanislow CA, Grilo CM, McGlashan TH: Factor analysis of DSM-III-R borderline personality disorder criteria in psychiatric inpatients. Am J Psychiatry 2000; 157:1629–1633Google Scholar
15. Sanislow CA, Grilo CM, Morey LC, Bender DS, Skodol AE, Gunderson JG, Shea MT, Stout RL, Zanarini MC, McGlashan TH: Confirmatory factor analysis of DSM-IV criteria for borderline personality disorder: findings from the Collaborative Longitudinal Personality Disorders Study. Am J Psychiatry 2002; 159:284–290Google Scholar
16. Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ: The borderline diagnosis I: psychopathology, comorbidity, and personality structure. Biol Psychiatry 2002; 51:936–950Google Scholar
17. White CN, Gunderson JG, Zanarini MC, Hudson JI: Family studies of borderline personality disorder: a review. Harv Rev Psychiatry 2003; 11:8–19Google Scholar
18. Zanarini MC, Frankenburg FR, Yong L, Raviola G, Reich DB, Hennen J, Hudson JI, Gunderson JG: Borderline psychopathology in the first-degree relatives of borderline and axis II comparison probands. J Personal Disord 2004; 18:439–447Google Scholar
19. Agrawal HR, Gunderson J, Holmes BM, Lyons-Ruth K: Attachment studies with borderline patients: a review. Harv Rev Psychiatry 2004; 12:94–104Google Scholar
20. McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, Zanarini MC, Stout RL: The Collaborative Longitudinal Personality Disorders Study: baseline patterns of DSM-IV axis I/II and II/II diagnostic co-occurrence. Acta Psychiatr Scand 2000; 102:256–264Google Scholar
21. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P). New York, New York State Psychiatric Institute, Biometrics Research, 1996Google Scholar
22. Zanarini MC, Frankenburg FR, Sickel AE, Yong L: The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV). Belmont, Mass, McLean Hospital, 1996Google Scholar
23. Clark LA: Schedule for Nonadaptive and Adaptive Personality (SNAP). Minneapolis, Minn, University of Minnesota Press, 1993Google Scholar
24. Shea MT, Glass DR, Pilkonis PA, Watkins J, Docherty JP: Frequency and implications of personality disorders in a sample of depressed inpatients. J Personal Disord 1987; 1:27–42Google Scholar
25. Keller MB, Lavori PW, Friedman B, Nielson E, Endicott J, McDonald-Scott P, Andreasen NC: The Longitudinal Interval Follow-up Evaluation. Arch Gen Psychiatry 1987; 44:540–548Google Scholar
26. Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaeffer E, Morey LC, Grilo CM, Shea MT, McGlashan TH, Gunderson JG: The Collaborative Longitudinal Personality Disorders Study: reliability of axis I and II diagnoses. J Personal Disord 2000; 14:291–299Google Scholar
27. Zanarini MC, Gunderson JG, Marino MF, Schwartz EO, Frankenburg FR: Childhood experiences of borderline patients. Compr Psychiatry 1989; 30:18–25Google Scholar
28. Grilo CM, Sanislow CA, Gunderson JG, Pagano ME, Yen S, Zanarini MC, Shea MT, Skodol AE, Stout RL, Morey LC, McGlashan TH: Two-year stability and change of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. J Consult Clin Psychol 2004; 72:767–775Google Scholar
29. Skodol AE, Pagano ME, Bender DS, Shea TM, Gunderson JG, Yen S, Stout RL, Morey LC, Sanislow CA, Grilo CM, Zanarini MC, McGlashan TH: Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder over two years. Psychol Med 2005; 35:443–451Google Scholar
30. Moye LA: Alpha calculus in clinical trials: considerations and commentary for the new millennium. Stat Med 2000; 19:767–779Google Scholar
31. Bender R, Lange S: Adjusting for multiple testing—when and how? J Clin Epidemiol 2001; 54:343–349Google Scholar
32. Gunderson JG: Borderline Personality Disorder: A Clinical Guide. Washington, DC, American Psychiatric Press, 2001Google Scholar
33. Feldman RB, Guttman HA: Families of borderline patients: literal-minded parents, borderline parents, and parental protectiveness. Am J Psychiatry 1984; 141:1392–1396Google Scholar