Awareness of Disorder and Suicide Risk in the Treatment of Schizophrenia: Results of the International Suicide Prevention Trial
Abstract
OBJECTIVE: Schizophrenia is characterized by high suicide risk and low awareness of disorder. Although awareness has benefits for medication compliance and clinical outcome, it is unclear how it may relate to suicide risk in this population. METHOD: This multicenter investigation assessed awareness and suicide-related behavior in 980 patients with schizophrenia or schizoaffective disorder. Patients were followed over 2 years and assessed by blinded raters for suicide-related events. RESULTS: Awareness of psychiatric condition at baseline was associated with increased risk of suicide events over the follow-up. This effect was mediated by depression and hopelessness levels. By contrast, changes in awareness associated with treatment decreased the risk of suicide. CONCLUSIONS: Although some patients may become depressed after acknowledging the clinical handicaps of their disorder, treatment-related changes in awareness are generally associated with a positive outcome relative to suicide risk. The complex interactions and mediation effects of these clinical variables require careful monitoring.
It is now well established that individuals with schizophrenia or schizoaffective disorder are at high risk for suicide (1–3) and that awareness of disorder in these patients is among the lowest of all major psychiatric conditions (4, 5). While greater awareness has typically been associated with better treatment compliance and improved long-term outcomes in this population (6, 7), its relationship to suicide risk may be unfavorable. Recent investigations indicate that awareness of schizophrenia is positively correlated with suicide risk (8) and, moreover, that this association may become increasingly evident over the course of treatment (9). The mechanisms by which patient awareness may exert both protective and aversive effects on the clinical manifestations of schizophrenia therefore appear inconsistent with simple main-effect models.
An alternative but more complex explanation for the role of awareness in schizophrenia suggests that patient acknowledgment of clinical symptoms or functional handicaps induces feelings of hopelessness and depression, which in turn increase suicide risk (10). The present investigation examines this question based on data collected through the International Suicide Prevention Trial (InterSePT). We hypothesized that greater awareness of disorder would be associated with the occurrence of suicidal behavior over the observation period but that this relationship would be mediated by depression or hopelessness levels.
Method
The methods of this study and the main findings concerning predictors of suicide events have been previously described in detail (11, 12). In summary, InterSePT is a 2-year randomized, open-label, blinded-rater trial that included 980 patients with schizophrenia (N=609) or schizoaffective disorder (N=371) who were recruited from 67 centers in 11 countries. Of the total group, 477 subjects received olanzapine, 479 received clozapine, 21 received no treatment, and three dropped out of the study before medication compliance could be verified. All patients were evaluated as being at high risk for suicide because of a suicide attempt or hospitalization to prevent suicide in the 3 years before inclusion or because of severe suicidal ideation with depressive symptoms or command hallucinations for self-harm in the week before inclusion. After providing informed written consent, the patients received weekly clinical monitoring and assessments for suicide-related events over 6 months and then at biweekly intervals for 1.5 years. Suicide events in both patient groups were defined as a suicide attempt or a hospitalization to prevent suicide but not ideation alone, and these judgments were made by blinded, independent evaluators of a suicide-monitoring board. Depression and awareness were assessed at baseline and weeks 24, 52, and 104 (or at endpoint, which was defined as a suicide event). Depression was assessed by using the total score (range=0–25) of the Calgary Depression Scale (13), and one item of this instrument was used to specifically assess hopelessness. Awareness of disorder was examined by using the Scale of Functioning (item 12, range=1–4), which assesses the level of awareness that the patient has concerning his or her psychiatric illness over the preceding 7 days (14). Statistical analyses of suicide monitoring with board-determined endpoints were conducted by using Cox’s proportional hazards regression models. Covariates included treatment medication, pooled country, sex, and age.
Results
For the clozapine treatment group, mean awareness levels were 2.33 (SD=0.87) for schizophrenia and 2.69 (SD=0.87) for schizoaffective disorder. For the olanzapine group, mean scores were 2.53 (SD=0.88) and 2.67 (SD=0.84), respectively. Both treatment groups demonstrated improvement over the follow-up concerning awareness of disorder and depression, and the patients who made a suicide attempt had less improvement in depression (2.49 [SD=5.54] versus 5.58 [SD=6.02]; z=7.373, p<0.0001).
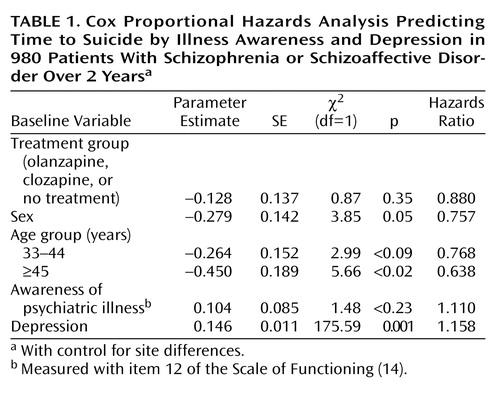
The results of a Cox proportional hazards analysis for main effects of baseline variables demonstrated that greater awareness significantly predicted time to suicide events (hazards ratio=1.17; χ2=4.38, df=1, p<0.04). As demonstrated by Table 1, the inclusion of depression at baseline in the model rendered awareness nonsignificant as a predictor of suicide behavior. However, along with male gender and younger age, depression remained a highly significant predictor of suicide events in the model (hazards ratio=1.16; χ2=175.59, df=1, p<0.0001). Parallel results were found when these analyses were limited to the hopelessness component of depression. No differences were observed by medication group concerning the relationships of depression or insight with suicidal behavior, and no differential effects were observed by diagnosis type. However, although baseline awareness was an absolute risk factor for suicide events, increases in awareness as a function of treatment (over the follow-up) were associated with a decreased risk of suicide events (hazards ratio=0.75; χ2=21.9, df=1, p<0.0001).
Conclusions
The present findings are consistent with past research indicating that baseline awareness levels are positively related to suicide risk (8, 9) but suggest that such effects are mediated by depression or hopelessness levels. Furthermore, important differences were found for the role of baseline awareness compared to treatment-related changes in awareness. Specifically, this latter variable was found to reduce the risk of suicide events over the 2-year observation period.
While the consequences of acknowledging one’s disorder may increase feelings of hopelessness or depression for many patients, increases in awareness related to treatment itself may be an important indicator of positive medication response. In this way, the present findings underscore the complexity of awareness in schizophrenia and schizoaffective disorder and indicate the need for careful clinical monitoring of both baseline and treatment-related changes in patient insight concerning his or her condition.
 |
Received May 1, 2003; revision received Dec. 30, 2003; accepted Jan. 12, 2004. From the Psychopathology Research Laboratory, University of Bordeaux. Address reprint requests to Dr. Swendsen, Psychopathology Research Laboratory, University of Bordeaux, 3 ter, Place de la Victoire, 33076 Bordeaux, France; [email protected] (e-mail).
1. Cohen LJ, Test MA, Brown RL: Suicide and schizophrenia: data from a prospective community treatment study. Am J Psychiatry 1990; 147:602–607; correction, 147:1110Link, Google Scholar
2. Meltzer HY, Fatemi H: Suicide in schizophrenia: the effect of clozapine. Clin Neuropharmacol 1995; 18:S18-S24Google Scholar
3. Gupta S, Black DW, Arndt S, Hubbard WC, Andreasen NC: Factors associated with suicide attempts among patients with schizophrenia. Psychiatr Serv 1998; 49:1353–1355Link, Google Scholar
4. Masson M, Azorin JM, Bourgeois ML: Awareness of illness in schizophrenic, schizo-affective, bipolar and unipolar mood disorders: results of a comparative study of 90 hospitalized patients. Ann Med Psychol (Paris) 2001; 159:369–374Crossref, Google Scholar
5. Pini S, Cassano GB, Dell’Osso L, Amador XF: Insight into illness in schizophrenia, schizoaffective disorder, and mood disorders with psychotic features. Am J Psychiatry 2001; 158:122–125Link, Google Scholar
6. Schwartz RC, Cohen BN, Grubaugh A: Does insight affect long-term inpatient treatment outcome in chronic schizophrenia? Compr Psychiatry 1997; 38:283–288Crossref, Medline, Google Scholar
7. Smith TE, Hull JW, Goodman M, Hedayat-Harris A, Willson DF, Israel LM, Munich RL: The relative influence of symptoms, insight, and neurocognition on social adjustment in schizophrenia and schizoaffective disorder. J Nerv Ment Dis 1999; 187:102–108Crossref, Medline, Google Scholar
8. Siris SG: Suicide and schizophrenia. J Psychopharmacol 2001; 15:127–135Crossref, Medline, Google Scholar
9. Cunningham-Owens DG, Carroll A, Fattah S, Clyde Z, Coffey I, Johnstone EC: A randomized, controlled trial of a brief interventional package for schizophrenia out-patients. Acta Psychiatr Scand 2001; 103:362–369Crossref, Medline, Google Scholar
10. Meltzer HY: Treatment of suicidality in schizophrenia. Ann NY Acad Sci 2001; 932:44–58Crossref, Medline, Google Scholar
11. Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, Bourgeois ML, Chouinard G, Islam MZ, Kane J, Krishnan KRR, Lindenmayer JP, Potkin S (InterSePT Study Group): Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry 2003; 60:82–91Crossref, Medline, Google Scholar
12. Potkin S, Alphs L, Hsu C, Krishnan KRR, Anand R, Young FK, Meltzer HY, Green A: Predicting suicidal risk in schizophrenic and schizoaffective patients in a prospective two-year trial. Biol Psychiatry 2003; 54:444–452Crossref, Medline, Google Scholar
13. Addington D, Addington J, Maticka-Tindale E, Joyce J: Reliability and validity of a depression rating scale for schizophrenics. Schizophr Res 1992; 6:201–208Crossref, Medline, Google Scholar
14. Rapaport MH, Bazzetta J, McAdams LA, Patterson T, Jeste CV: Validation of the Scale of Functioning in older outpatients with schizophrenia. Am J Geriatr Psychiatry 1996; 4:218–228Crossref, Medline, Google Scholar



