The Human Genome: Susceptibility Loci
Many psychiatric illnesses, such as bipolar disorder and schizophrenia, are complex genetic disorders, in which genetic heterogeneity is assumed. However, identifying chromosomal regions linked to these syndromes (susceptibility loci) has its challenges. In family linkage analysis, failure of subsequent studies to confirm previously nominated susceptibility loci is commonplace. Several methodological issues are at play in this failure to confirm, including the power of the individual studies, the inherent limitations of linkage analysis, and variation among population samples. Despite this, multiple susceptibility loci have been identified for several psychiatric diagnoses, including schizophrenia and bipolar disorder. Most probably, these susceptibility loci interact with each other and the environment to produce the clinical syndromes. Susceptibility loci are identifiable regions of a chromosome that are inherited with the illness in families, and they are assumed to include the illness vulnerability allele that partially explains illness risk in these families.
Geneticists now see that some of these susceptibility loci for schizophrenia overlap with loci for bipolar disorder. The figure identifies the loci for bipolar disease alone (B), for schizophrenia alone (S), and for bipolar and schizophrenia (*). While bipolar disorder and schizophrenia are two distinct psychiatric diagnostic categories, each with its own characteristic symptoms, course of illness, and pharmacology, they have several similarities: age at onset, lifetime risk, suicide risk, gender distribution, and heritability estimates. Family studies indicate that the first-degree relatives of bipolar probands and the first-degree relatives of schizophrenia probands are at higher than normal risk for schizoaffective and recurrent unipolar disorders, suggesting some shared familial risk. The molecular data represented here support the idea of shared genetic risk. The family study and molecular data suggest that these two groups of disorders may be more closely related than previously considered. Novel genes corresponding to the loci will be identified over the next decade. Characterization of these susceptibility alleles will allow for correlation between the genetic data and clinical phenotype. Because environmental factors drive gene expression, knowledge of the environmental risk factors will certainly inform data from the molecular level.
Address reprint requests to Dr. Tamminga, Maryland Psychiatric Research Center, University of Maryland, P.O. Box 21247, Baltimore, MD 21228. Image is an updated version of one published in Biological Psychiatry (W.H. Berrettini, 48:531–538; copyright 2000 by the Society of Biological Psychiatry); reprinted by permission of Elsevier Science.
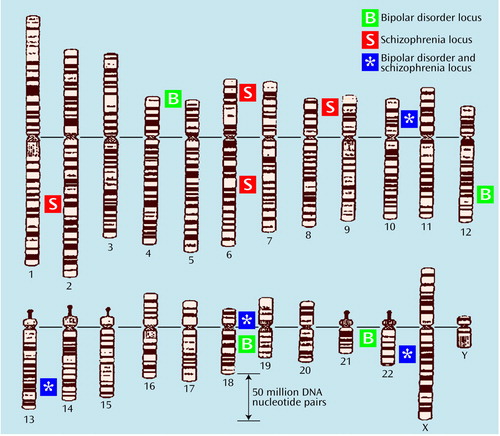
Figure.
Ideograms of human chromosomes showing susceptibility loci for bipolar disorder, schizophrenia, and both disorders. The identifying symbols are placed to the right of the structures to which they refer.



