Memories of Childhood Abuse: Dissociation, Amnesia, and Corroboration
Abstract
OBJECTIVE: This study investigated the relationship between self-reported childhood abuse and dissociative symptoms and amnesia. The presence or absence of corroboration of recovered memories of childhood abuse was also studied. METHOD: Participants were 90 female patients admitted to a unit specializing in the treatment of trauma-related disorders. Participants completed instruments that measured dissociative symptoms and elicited details concerning childhood physical abuse, sexual abuse, and witnessing abuse. Participants also underwent a structured interview that asked about amnesia for traumatic experiences, the circumstances of recovered memory, the role of suggestion in recovered memories, and independent corroboration of the memories. RESULTS: Participants reporting any type of childhood abuse demonstrated elevated levels of dissociative symptoms that were significantly higher than those in subjects not reporting abuse. Higher dissociative symptoms were correlated with early age at onset of physical and sexual abuse and more frequent sexual abuse. A substantial proportion of participants with all types of abuse reported partial or complete amnesia for abuse memories. For physical and sexual abuse, early age at onset was correlated with greater levels of amnesia. Participants who reported recovering memories of abuse generally recalled these experiences while at home, alone, or with family or friends. Although some participants were in treatment at the time, very few were in therapy sessions during their first memory recovery. Suggestion was generally denied as a factor in memory recovery. A majority of participants were able to find strong corroboration of their recovered memories. CONCLUSIONS: Childhood abuse, particularly chronic abuse beginning at early ages, is related to the development of high levels of dissociative symptoms including amnesia for abuse memories. This study strongly suggests that psychotherapy usually is not associated with memory recovery and that independent corroboration of recovered memories of abuse is often present.
In recent years, the explosion of reports of childhood abuse has raised questions about the nature of memory for traumatic events, the occurrence of amnesia for childhood abuse, and the validity and accuracy of recovered memories. Many clinicians accept recovered memories of childhood abuse as essentially valid reports of early experiences, and clinical work with recovered memories has proved to be useful in some patients. Recently, however, a number of investigators have questioned the validity of recovered memory of childhood abuse, arguing that many clinicians may be colluding in the creation of pseudomemories. A heated debate has emerged regarding therapists’ role in the retrieval of previously unremembered memories of childhood abuse.
Recent studies in cognitive psychology have shown that memories can be inaccurate. For example, investigators studying the impact of stressful experiences on memory have tested college students under demanding conditions (1–3) or exposed study participants to shocking photographic material (4, 5). Study participants are often remarkably inaccurate in recounting details of their experience (4–7). The role of suggestion in the malleability of memory also has been well established in laboratory studies (8–11). In some protocols, participants are shown pictures, slides, or videotapes of an event and then are asked to recall the event. When given cues or suggestions, they often make errors concerning peripheral details of the events. However, despite evidence that memory content can be influenced by suggestion, emotional arousal, and personal meaning, the bulk of memory research actually supports the accuracy of memory for the central components of significant events (12).
There also is evidence of memory for events that did not occur. One well-known personal pseudomemory was described by Piaget, the well-known Swiss theorist of childhood cognitive development (13). For many years during his childhood, Piaget had a clear visual memory of someone trying to kidnap him from his pram when he was 2 years old. The memory also involved his nanny chasing away the potential kidnapper and then going home and telling the family about the incident. Years later, when Piaget was 15, the nanny returned to the Piaget family and confessed that the incident had never occurred. Her motive had been to enhance her position in the household, but she subsequently suffered guilt about the fabrication and about the watch she had received as a reward.
Piaget’s experience suggests that persons may create pseudomemories of events that never actually occurred, especially after being told of such “events” by trusted individuals. The memories may seem valid, and persons may not recall the true source of the information (so-called source amnesia). In experimental protocols with college students, researchers have given cues about both real events (from information supplied by parents) and false childhood events and have asked participants to describe these events (14). Over three interviews, approximately 6% of participants developed vivid pseudomemories of false events. In a similar protocol, up to 25% of participants developed vivid pseudomemories if they were asked to imagine the false events in detail (15). These studies support the contention that pseudomemories can be induced, particularly with repeated suggestion, rehearsal, and the use of imagery. It should be noted, however, that only a minority of participants responded to the cues to remember false events, suggesting that certain individuals may have more vulnerability than others to creating pseudomemories. Or, from the reverse perspective, 75% to 94% of participants appeared to be resistant to the development of pseudomemories.
In contrast to the malleability of memory demonstrated in experimental protocols, some investigators have hypothesized that memory of actual traumatic events is different from memory of ordinary or laboratory experiences. For example, investigators (16–19) have suggested that traumatic memories are segregated and stored apart from ordinary narrative memory and thereby are less subject to ongoing modification in response to new experiences. In contrast to narrative memories that are integrative, malleable, and fitted into the individual’s personal cognitive schemas, traumatic memories are said to be inflexible, nonnarrative, automatic, triggered, and disconnected from ordinary experience. This nonintegration is considered the basis for remembering through behavioral reenactment, somatic sensation, or intrusive images that are disconnected from conscious verbal memory. Because the memories are unassimilated, they retain their original force—“unremembered and therefore unforgettable” (19). While ordinary narrative memory is dynamic and both changes and degrades over time, traumatic memory has been described as “indelible” (20).
Clinical research generally has supported the concepts of dissociative amnesia and recovered memory in relation to traumatic events. Clinical investigators have found relatively high rates of self-reported amnesia for childhood sexual abuse (19%–62%) in clinical populations being treated for trauma-related conditions (21–24). Moreover, these studies suggest that the incidence of amnesia is highly correlated with early onset of abuse, chronicity of abuse, and severity of abuse (e.g., violence, multiple perpetrators, physical injury, fear of death). Terr’s investigations with traumatized children also have demonstrated that there are differential effects depending on the chronicity of abuse (25–27). Children who have experienced limited, circumscribed trauma have hypermnesia—“clear, detailed accounts of their experiences [that] makes one conclude that these memories stay alive in a very special way” (27, p. 14). In contrast, chronically traumatized children demonstrate extensive amnesia. Terr notes that this kind of chronic traumatization results in a variety of symptoms—“massive denial, repression, dissociation, self-anesthesia, self-hypnosis, identification with the aggressor, and aggression turned against the self” (27, p. 15)—that may significantly alter subsequent recall. Thus, chronically traumatized patients are most likely to suffer amnesia, but, given their levels of denial and dissociative defenses, these patients may also be most vulnerable to distortions and errors in recall.
The present study investigated both the nature and the validity of traumatic memory of childhood abuse. Self-reported physical abuse, sexual abuse, and witnessing violence and the parameters of abuse experiences were examined in relation to dissociative symptoms and amnesia. We sought to replicate the findings that childhood physical and sexual abuse would be related to high levels of dissociative symptoms (28–30) and hypothesized that early age at onset and higher frequency of abuse would be correlated with higher levels of dissociative symptoms, including amnesia. We examined recovered memory following amnesia for abuse, particularly in relation to the circumstances of memory recovery, the role of suggestion in recall, and the existence of physical evidence or verbal confirmation to validate the accuracy of the memories.
METHOD
The participants for this study were recruited from female inpatients, 18–60 years old, in a psychiatric teaching hospital. All patients consecutively admitted to a unit specializing in the treatment of posttraumatic and dissociative disorders were considered for participation. Reasons for admission were varied; although some patients were admitted with high levels of posttraumatic or dissociative symptoms, others had nonspecific difficulties such as suicidal impulses or inability to function. Patients with the diagnosis of a psychotic illness (e.g., schizophrenia or mood disorder with psychotic features) or an organic brain syndrome were excluded from this study. Of 179 patients meeting inclusion criteria, 31 were discharged before being approached for the study. Of the remaining 148, 109 (74%) agreed to participate, 21 (14%) refused, and 18 (12%) were felt by their treating clinicians to have symptoms that would have made it clinically inappropriate for them to participate. Patients who refused to participate typically indicated that they would find the subject matter of the study upsetting. The clinicians treating those deemed inappropriate generally cited unstable symptoms, such as severe posttraumatic or dissociative symptoms, or tenuous control of impulses. After a complete description of the study procedures to prospective participants, written informed consent was obtained. Of the 109 potential participants, 13 were unable to complete the research protocol and six had very incomplete data and were dropped from the study, leaving 90 participants. Not all participants responded to every research question. Where this was the case, percentages are reported relative to the number of participants who responded to that particular question.
The participants’ mean age was 34.9 years (SD=8.8). Seventy-nine (88%) were Caucasian. Forty-five (50%) had never married, 19 (21%) were married or living with a partner, and 26 (29%) were separated, divorced, or widowed. Most (73%; 51 of 70 responses) had annual household incomes under $20,000. Sixty-six (73%) reported some form of education beyond high school, and nearly all (94%; 84 of 89 responses) listed their usual occupation as work, work in the past, or student. However, a majority (64%) reported that they were currently disabled or unemployed.
Participants completed two self-report instruments: the Dissociative Experiences Scale (31–33), a 28-item questionnaire with established validity and reliability that measures the current prevalence of dissociative symptoms, and a revision of the Life Experiences Questionnaire (28, 29, 34) that gathers detailed information about traumatic experiences in childhood. Responses to the Life Experiences Questionnaire were considered indicative of childhood abuse if participants reported that before age 16 years they had been “hit really hard, kicked, punched, stabbed, or thrown down” (physical abuse); had been “pressured against your will into forced contact with the sexual parts of your body or his/her body” (sexual abuse); or had seen “anyone hurt in a physical conflict or forced sexual activity” (witnessing abuse).
Each participant underwent a structured interview that asked if she experienced amnesia for currently recalled traumatic experiences that occurred in childhood. The interviewer (B.L.G. or L.M.F.) was not involved in the study patients’ clinical care. Participants were considered to have had complete amnesia if there was a period during which they “did not remember that this [traumatic] experience happened” and were considered to have had partial amnesia if there was a period during which they “did not remember significant parts of this [traumatic] experience.” Participants who reported a period of complete amnesia were asked about the circumstances of first recovered memory, including where (e.g., home, work, therapy), with whom (e.g., alone or with others), in what state of consciousness (e.g., awake, dreaming, hypnotized), and whether they were in psychotherapy or counseling during that period of their lives. Participants were asked whether the possibility of abuse had been suggested to them before the first recovered memory (“Prior to recalling being hurt/seeing others hurt, did anyone suggest to you that this may have occurred?”). Participants also were asked whether they had sought or obtained verbal information (“Have you had anyone confirm these events?”) or had physical evidence (e.g., scars from injuries, medical records, or other documentation such as photos, diaries, letters) that validated the occurrence of abuse that was previously “forgotten” and subsequently recalled.
Participants’ self-report responses to the Life Experiences Questionnaire were analyzed for the rates of each type of abuse, the age at onset, and frequency of abuse. For most analyses of data, nonparametric statistics were used, given the type of data and the nonnormal distribution of Dissociative Experiences Scale scores. Kruskal-Wallis analyses were used to compare Dissociative Experiences Scale scores across levels of amnesia for each type of abuse. Further, the Mann-Whitney U Wilcoxon rank sum W test was used to test differences in Dissociative Experiences Scale scores (across types of abuse) between levels of frequency of abuse and levels of amnesia. Spearman correlation coefficients (two-tailed) were used to evaluate whether age at onset of abuse was correlated with the degree of amnesia and to examine the relationship between onset of abuse and Dissociative Experiences Scale scores.
RESULTS
Self-Reported Childhood Abuse in Relation to Dissociative Symptoms and Amnesia
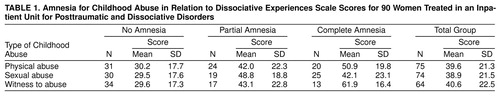
Because this participant group (N=90) was drawn from a posttraumatic stress and dissociative disorders treatment unit, the majority of participants reported a high level of childhood abuse experiences. Seventy-five (83%) reported physical abuse, 74 (82%) reported sexual abuse, and 64 (71%) reported witnessing violence. Participants reporting any kind of abuse also reported a substantial rate of both partial and complete amnesia and elevated Dissociative Experiences Scale scores in a range consistent with PTSD (median scores above 31.3 found for PTSD patients by Bernstein and Putnam [31]) (table 1). Among participants reporting physical abuse, analysis showed significant differences in Dissociative Experiences Scale scores across levels of amnesia for the traumatic events (χ2=11.50, df=2, p=0.003). Significant differences were also obtained for the groups reporting sexual abuse (χ2=9.18, df=2, p=0.01) and witnessing abuse (χ2=19.15, df=2, p=0.0001).
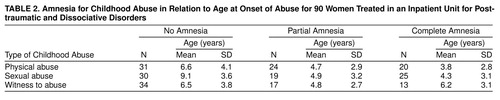
The mean age at onset of physical abuse, sexual abuse, and witnessing violence was generally early in childhood, before adolescence (table 2). Earlier age at onset was correlated with a higher degree of amnesia for physical abuse (Spearman r=–0.39, N=73, p=0.001) and sexual abuse (Spearman r=–0.55, N=73, p<0.001) but showed only a trend for witnessing abuse (Spearman r=–0.08, N=62, p=0.55, n.s.). Early age at onset was also correlated with higher Dissociative Experiences Scale scores for physical abuse (Spearman r=–0.27, N=68, p=0.03) and sexual abuse (Spearman r=–0.48, N=67, p<0.001) but was only weakly associated with witnessing abuse (Spearman r=–0.09, N=56, p=0.53, n.s.).
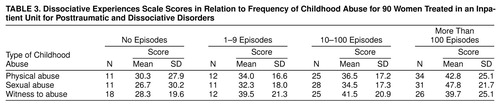
Analysis of mean Dissociative Experiences Scale scores in relation to frequency of childhood abuse showed a clear trend of higher scores with more frequent episodes of abuse (table 3), although not all differences were statistically significant. Only participants with very frequent sexual abuse (more than 100 episodes) had significantly higher levels of dissociation than participants with infrequent or no abuse (fewer than 10 episodes) (Mann-Whitney z=–2.13, N=42, p=0.03).
Circumstances Concerning Recovered Memory, Suggestion, and Corroboration of Childhood Abuse
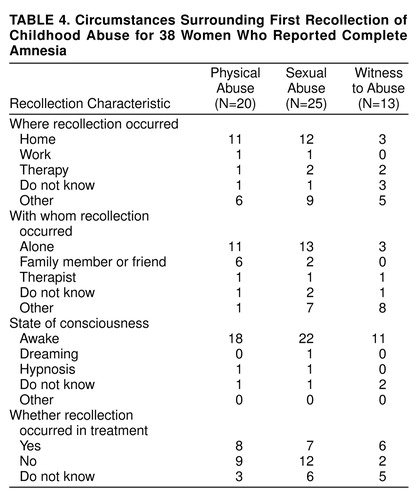
Most of the participants reporting complete amnesia for physical abuse and sexual abuse had their first recollection of the abuse while at home and alone (table 4). Few participants (only one or two for each type of abuse) reported being in a therapy session when they first remembered the abuse. Nearly all were awake, and hypnosis was a factor for only one participant. Many of the participants (at least 45% for sexual abuse, 48% for physical abuse, and 15% for witnessing abuse) were not involved in any kind of psychological treatment or counseling when they first recovered memories of traumatic experiences.
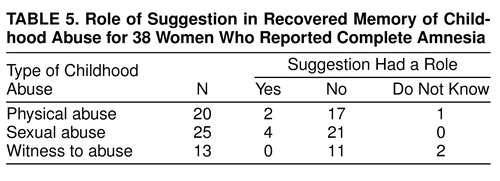
Participants who reported a period of complete amnesia for episodes of childhood abuse were asked about the role of suggestion in memory recovery. As shown in table 5, the vast majority of participants with all types of abuse did not recall any overt suggestion before the first recovered memory.
A majority of participants who reported a period of complete amnesia for episodes of childhood abuse made some attempt to corroborate their recovered memories. As shown in table 6, of those who attempted corroboration, more than half found physical evidence of the abuse (e.g., scars from physical injury, medical records). The rates of verbal confirmation for the group of participants with complete amnesia who attempted corroboration were strikingly high for physical abuse (93%) and for sexual abuse (89%). Half of the participants with complete amnesia who sought confirmation of witnessing abuse were able to find corroboration.
DISCUSSION AND CONCLUSIONS
The high rates of physical and sexual abuse in this study are similar to other reports of clinical populations with posttraumatic and dissociative disorders (21, 22, 29). Childhood abuse experiences were related to higher levels of dissociation. Early age at onset was correlated with higher dissociative symptoms and greater levels of amnesia for physical and sexual abuse. More frequent sexual abuse was correlated with higher levels of dissociation. These findings have considerable face validity as dissociative capacity is thought to be greater in younger children (35, 36), and chronic abuse may result in the persistent utilization of dissociative defenses—including amnesia—into adulthood. Many of the findings from this study are consistent with other studies concerning dissociation related to physical and sexual abuse (28, 30), dissociation related to parameters of sexual abuse (29), and amnesia in persons with childhood sexual abuse (21, 22).
There appears to be a particular subset of severely and chronically abused patients with high rates of amnesia. Of note are the anecdotal descriptions of amnestic experiences reported by many of our participants. For the most part, these participants lost memory for whole periods of their lives—recollecting neither traumatic events nor neutral or positive experiences. These descriptions are strikingly similar to Terr’s observation that chronically traumatized children “may forget whole segments of childhood—from birth to age 9, for instance” (27, p. 17). These reports also suggest that the underlying mechanism for this kind of amnesia may not be repression of overwhelming experiences or selective inattention to noxious events. The massive failure to integrate entire periods of childhood is consistent with the hypothesis that intense and chronic traumatic experiences may lead to pervasive changes in the mechanisms for processing and storing information. Thus, traumatic memory may be different from ordinary memory. This model is also consistent with the concept of dissociation in which various mental contents exist in different states held separately from each other.
There were a number of participants who reported childhood abuse—including multiple kinds of abuse, frequent abuse, and abuse with early age at onset—yet had relatively low levels of dissociative experiences and little amnesia. It is possible that this group of participants actually had amnesia but had yet to recover memories of more abuse. However, a recent analysis by Putnam et al. (37) suggests that in traumatized clinical populations there are subsets of high dissociators and low dissociators. Thus, the subset of participants with significant abuse, relatively little dissociative symptoms, and no amnesia may represent a group with low dissociative capacity. The differential susceptibility toward the development of dissociative symptoms may also explain the large standard deviations on the Dissociative Experiences Scale that we found in many categories. Further research is needed to help determine factors associated with dissociative capacity, such as innate characteristics or environmental circumstances.
Our findings concerning the recollection of abuse experiences suggest that memory recovery usually is not directly related to participation in psychotherapy. A substantial number of our participants were in some kind of treatment during the period that they began recalling their abuse—as would be expected by their high levels of symptoms. If the therapy was a primary causal factor in production of these memories, it would be expected that many would have actually been in therapy sessions during their first recollections. However, most participants reported that they first began to remember at home when alone or with family or friends, and not in therapy sessions. Most participants also denied that abuse had been suggested, although subtle suggestion (e.g., emphasis on certain subjects, tone of voice, nods, etc.) might not have been perceived as such.
Many of the participants who had complete amnesia had made attempts to corroborate their recovered memories. Nearly all participants who reported physical and sexual abuse and who attempted corroboration were able to find some kind of verification. Our corroboration rate (89%) of participants with complete amnesia for sexual abuse and who attempted to confirm the abuse is similar to that reported by Herman and Schatzhow (83%) (22) in a clinical population of patients being treated for abuse-related difficulties. It should be noted, however, that although participants in this study were asked about corroboration of recovered memory, some may have reported about their attempts to validate experiences that they had always remembered. Nonetheless, this level of corroboration is strikingly high given that much abuse leaves no physical scars and that child abuse almost always occurs in great secrecy. At a minimum, our data support the validity of some reports of recovered memory for childhood abuse. In particular, our criteria for confirmation were relatively stringent, asking for actual independent confirmation rather than just that someone else believed that the abuse might have happened.
The findings of this study argue against the notion that many or most reports of childhood abuse are pseudomemories. Moreover, abuse memories that are recovered in therapy are not necessarily suspect. In Kluft’s study of 34 dissociative identity disorder patients (38), 68% of the 19 patients who were able to confirm abuse memories first recalled these experiences in therapy. Moreover, many of these patients recovered memories in therapy using hypnotic techniques. Three patients were also able to disconfirm memories, and two patients had both validated memories of abuse and pseudomemories. These findings suggest that neither psychotherapy nor hypnosis, per se, are treatments that encourage pseudomemories and that all memories should be viewed critically in the therapeutic setting and subject to clinical evaluation as to their validity. However, our findings do not rule out the possibility of wholesale creation of pseudomemories resulting from grossly improper therapeutic practices. Of interest are a very small number of participants in our study who recalled abuse while in therapy sessions, who had used hypnosis, who had been recipients of suggestion, and/or who could not find any corroboration of their memories of abuse. Some of the participants in this group might be patients who developed pseudomemories of their trauma. Unfortunately, in this study, this group was too small to analyze. However, similar populations should be further investigated as to whether they differ in any other ways from those with apparently valid recovered memories of abuse.
There are limitations to this study worth noting. The major methodological limitation is the use of retrospective self-report for memories of childhood abuse, episodes of amnesia, and the circumstances of recovered memory. These self-reports were potentially subject to distortion and inaccuracies (e.g., difficulties in distinguishing between different levels of amnesia, inability to accurately recall the number of episodes of abuse, errors in recalling when and how memories were recovered). The results are also limited by the participant pool of primarily Caucasian women. In addition, the use of a participant pool of predominantly disabled patients being treated for trauma-related difficulties limits the applicability of our findings to other less traumatized and more functional clinical and general population groups. In our analyses, the multiple types of abuse reported by many participants makes it difficult to draw conclusions concerning the effects of any particular type of abuse in comparison to another. Similarly, this study did not examine the role of severe neglect—which is known to be ubiquitous among maltreated children (39)—in the development of dissociative symptoms.
The results of this study should be interpreted somewhat narrowly, as it investigates only the relationship between early trauma and subsequent dissociative symptoms and amnesia. In the clinical arena, patients with childhood abuse may present with other primary difficulties—some may have abuse-related difficulties such as poor ego functioning or substance abuse, and others may have difficulties that are entirely independent of childhood experiences. In addition, this study recruited participation from psychiatric inpatients and hence does not elucidate the mechanisms whereby persons who have been traumatized in childhood have been able to overcome or compensate for those experiences and have fewer or no dissociative or posttraumatic difficulties. Given the limitations of this study, the conclusions cannot be considered definitive. Nonetheless, in the context of continuing controversy concerning amnesia and recovered memory, this study does provide further evidence supporting the occurrence of amnesia for childhood traumatic experiences and the subsequent recovery of memory.
The participants in this study reported high levels of amnesia, and many of their subsequently recovered memories could be independently corroborated. Nonetheless, our results do not obviate the possible role of psychotherapy and suggestion in the creation of pseudomemory in some patients. Although there is little evidence that direct questioning about abuse, per se, results in false memories, clinicians must be careful not to inquire about possible abuse in a way that is suggestive of any particular responses. Especially when memories are fragmentary, clinicians must support the psychological validity of the memories but avoid coming to premature conclusions about the occurrence of trauma without sufficient evidence. When recovered memory begins to replace amnesia, clinicians must be open to the possibility of real abuse but must allow patients to reconstruct—without suggestion—a credible personal history that is consistent with past and current symptoms.
Presented in part at Trauma and Memory: An International Research Conference, Durham, N.H., July 28, 1996. Received Jan. 5, 1998; revision received Sept. 14, 1998; accepted Nov. 19, 1998. From the Dissociative Disorders and Trauma Program, McLean Hospital, and the Department of Psychiatry, Harvard Medical School, Boston. Address reprint requests to Dr. Chu, McLean Hospital, 115 Mill St., Belmont, MA 02478
 |
 |
 |
 |
 |
1. Eriksen C: Defense against ego threat in memory and perception. J Abnorm Soc Psychol 1952; 3:253–256Google Scholar
2. Eriksen C: Individual differences in defensive forgetting. J Exp Psychol 1953; 44:442–443Crossref, Google Scholar
3. Tudor TG, Holmes DS: Differential recall of successes and failures. J Res Personality 1973; 7:208–224Crossref, Google Scholar
4. Christianson S-Å, Loftus EF: Memory for traumatic events. Applied Cognitive Psychol 1987; 1:225–239Crossref, Google Scholar
5. Kramer TH, Buckhout R, Fox P, Widman E, Tusche B: Effects of stress on recall. Applied Cognitive Psychol 1991; 5:483–488Crossref, Google Scholar
6. Christianson S-Å, Loftus EF: Remembering emotional events: the fate of detailed information. Mem Cognit 1991; 5:81–108Google Scholar
7. Holmes DS: Evidence for repression: an examination of 60 years of research, in Repression and Dissociation: Implications for Personality Theory, Psychopathology, and Health. Edited by Singer J. Chicago, University of Chicago Press, 1990, pp 85–102Google Scholar
8. Loftus EF, Korf NL, Schooler JW: Misguided memories: sincere distortions of reality, in Credibility Assessment. Edited by Yuille JC. Norwell, Mass, Kluwer Academic, 1989, pp 155–173Google Scholar
9. Loftus E: Reacting to blatantly contradictory information. Mem Cognit 1979; 7:368–374Crossref, Google Scholar
10. Schooler J, Gerhard E, Loftus E: Qualities of the unreal. J Exp Psychol 1986; 12:171–181Google Scholar
11. Schumaker JF (ed): Human Suggestibility: Advances in Theory, Research, and Application. New York, Routledge, 1991Google Scholar
12. Chu JA, Matthews JA, Frey LM, Ganzel B: The nature of traumatic memories of childhood abuse. Dissociation 1996; 9:2–17Google Scholar
13. Piaget J: Plays, Dreams and Imitation in Childhood. New York, WW Norton, 1962Google Scholar
14. Hyman IE, Pentland J: The role of mental imagery in the creation of false childhood memories. J Memory and Language 1992; 35:101–117Crossref, Google Scholar
15. Hyman IE, Troy TH, Billings FJ: False memories of childhood experiences. Applied Cognitive Psychol 1995; 9:181–197Crossref, Google Scholar
16. Crabtree A: Dissociation and memory: a two hundred year perspective. Dissociation 1992; 5:150–154Google Scholar
17. Kolb LC: A neuropsychological hypothesis explaining posttraumatic stress disorders. Am J Psychiatry 1987; 144:989–995Link, Google Scholar
18. van der Kolk BA, Ducey CP: The psychological processing of traumatic experience: Rorschach patterns in PTSD. J Trauma Stress 1989; 2:259–274Crossref, Google Scholar
19. van der Kolk BA, van der Hart O: The intrusive past: the flexibility of memory and the engraving of trauma. Am Imago 1991; 48:425–454Google Scholar
20. LeDoux JE: Emotion as memory: anatomical systems underlying indelible neural traces, in The Handbook of Emotion and Memory. Edited by Christianson S-Å. Hillsdale, NJ, Lawrence Erlbaum Associates, 1992, pp 289–297Google Scholar
21. Briere J, Conte J: Self-reported amnesia in adults molested as children. J Trauma Stress 1993; 6:21–31Crossref, Google Scholar
22. Herman JL, Schatzhow E: Recovery and verification of memories of childhood sexual trauma. Psychoanal Psychol 1987; 4:1–4Crossref, Google Scholar
23. Loftus EF, Polonsky S, Fullilove MT: Memories of childhood sexual abuse. Psychol Women Q 1994; 18:64–84Crossref, Google Scholar
24. Williams LM: Recall of childhood trauma: a prospective study of women’s memories of child sexual abuse. J Consult Clin Psychol 1994; 62:1167–1176Google Scholar
25. Terr L: Remembered images of psychic trauma. Psychoanal Study Child 1985; 40:493–533Crossref, Medline, Google Scholar
26. Terr L: What happens to memories of early childhood trauma? J Am Acad Child Adolesc Psychiatry 1988; 27:96–104Google Scholar
27. Terr LC: Childhood traumas: an outline and overview. Am J Psychiatry 1991; 148:10–20Link, Google Scholar
28. Chu JA, Dill DL: Dissociative symptoms in relation to childhood physical and sexual abuse. Am J Psychiatry 1990; 147:887–892Link, Google Scholar
29. Kirby JS, Chu JA, Dill DL: Correlates of dissociative symptomatology in patients with physical and sexual abuse histories. Compr Psychiatry 1993; 34:250–263Crossref, Google Scholar
30. Saxe GN, van der Kolk BA, Berkowitz R, Chinman G, Hall K, Lieberg G, Schwartz J: Dissociative disorders in psychiatric inpatients. Am J Psychiatry 1993; 150:1037–1042Google Scholar
31. Bernstein EM, Putnam FW: Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727–735Crossref, Medline, Google Scholar
32. Loewenstein RJ, Putnam FW: A comparison study of dissociative symptoms in patients with complex partial seizures, MPD, and post-traumatic stress disorder. Dissociation 1988; 1:17–23Google Scholar
33. Ross CA, Norton GR, Anderson G: The Dissociative Experiences Scale: a replication study. Dissociation 1988; 1:21–32Google Scholar
34. Bryer JB, Nelson BA, Miller JB, Krol PA: Childhood sexual and physical abuse as factors in adult psychiatric illness. Am J Psychiatry 1987; 144:1426–1430Google Scholar
35. Ross CA, Ryan L, Anderson G, Ross D, Hardy L: Dissociative experiences in adolescents and college students. Dissociation 1989; 2:239–242Google Scholar
36. Ross CA, Joshi S, Currie R: Dissociative experiences in the general population. Am J Psychiatry 1990; 147:1547–1552Google Scholar
37. Putnam FW, Carlson EB, Ross CA, Anderson G, Clark P, Torem M, Bowman ES, Coons P, Chu JA, Dill DL, Loewenstein RJ, Braun BG: Patterns of dissociation in clinical and nonclinical samples. J Nerv Ment Dis 1996; 184:673–679Crossref, Medline, Google Scholar
38. Kluft RP: The confirmation and disconfirmation of memories of abuse in dissociative identity disorder patients: a naturalistic study. Dissociation 1995; 4:253–258Google Scholar
39. US Department of Public Health, Administration for Children and Families, National Center on Child Abuse and Neglect: The Third National Incidence Study of Child Abuse and Neglect. Washington, DC, US Government Printing Office, 1996Google Scholar



