Relationship Between Childhood Behavioral Disturbance and Later Schizophrenia in the New York High-Risk Project
Abstract
OBJECTIVE: An association between childhood behavioral disturbance and adulthood schizophrenia has been seen previously in retrospective or follow-back studies and in prospective studies. The authors examined the relationship between childhood behavioral problems and adulthood schizophrenia-related psychoses. Because a high rate of childhood behavioral problems is known to be associated with adult substance abuse, these analyses controlled for substance abuse. METHOD: The subjects of this investigation (N=185) were offspring of parents with schizophrenia or affective disorder and of normal parents from the New York High-Risk Project (sample A). Data on childhood behavioral problems were obtained in a parent interview at initial assessment in 1971–1972. Adulthood outcomes (schizophrenia-related psychoses, affective disorders, anxiety disorders, substance abuse) were based on lifetime axis I diagnoses according to the Research Diagnostic Criteria. RESULTS: Substance abuse had a significant interaction with the clinical outcome groups. In subjects without substance abuse, those with schizophrenia-related psychoses had exhibited significantly more behavioral problems as children than had adult offspring with affective or anxiety disorder or with substance abuse only or no disorder. CONCLUSIONS: These results support the view that schizophrenia-related psychoses can be followed back to early behavioral disturbances. The confounding effects of substance abuse should be statistically controlled in studies of longitudinal associations between childhood behavioral disturbance and axis I outcomes.
One of the major goals of schizophrenia research in the past three decades has been the identification of precursor symptoms and areas of dysfunction before the manifestation of schizophrenia. Psychological and neurodevelopmental abnormalities in preschizophrenic persons have repeatedly been described, and it is now well established (1–3) that early signs of the disorder can be found during infancy. Presumably, these neuropsychological domains influence the individual’s interpersonal functioning and behavior. Consistent with this assumption are results from earlier investigations using retrospective designs (e.g., reference 4) or follow-back designs (e.g., references 5–7) that have shown behavioral deviations in children who later developed schizophrenia, years before the onset of overt psychosis. Prospective studies (8, 9) have confirmed associations between childhood developmental characteristics, including behavioral abnormalities, and adulthood onset of schizophrenia. But still, there is some question with respect to specificity, i.e., whether behavioral disturbances precede only schizophrenia or, rather, indicate general psychiatric difficulty in adulthood. Some investigators have found that schizophrenic individuals can be distinguished from patients with other mental disorders and nonpsychiatric groups by early behavioral abnormalities (8), whereas others have failed to do so (10, 11).
In a 20-year follow-up of school children by Champion et al. (12), behavioral disturbance was shown to be related to a markedly higher rate of severely negative life events in adulthood. Such events, in turn, might put these subjects at greater risk for various psychiatric disorders in adult life. Children who display behavioral problems are also known to be at higher risk for developing externalizing disorders, such as alcohol and drug abuse (13–16). While rates of substance abuse are considerable in schizophrenia and affective disorder (17, 18), the effect of this comorbidity with respect to early behavioral abnormalities is unclear.
The high-risk method was developed to assess early social, psychological, and biological characteristics in individuals with higher than average risk of mental disorders, before the onset of psychopathology, by using a prospective, longitudinal research design. The advantages of the high-risk design have been put forward many times (e.g., reference 19). Children at risk for schizophrenia by virtue of having at least one schizophrenic parent behave differently at school from other children in that they present greater disharmony, less scholastic motivation, and more emotional instability than comparison subjects (20). In the New York High-Risk Project, which began in 1971, offspring of schizophrenic and affectively ill parents have been followed from childhood to midadulthood. The project thus provides a valuable opportunity to prospectively compare behavioral antecedents of a broad range of adulthood psychiatric disorders. The purpose of this analysis was to examine longitudinal associations between childhood behavioral problems reported by the parents at the initial assessment, when the children were on average 9.5 years old, and clinical outcomes after 25 years of follow up, with consideration of patterns of comorbidity with substance abuse.
METHOD
Subjects
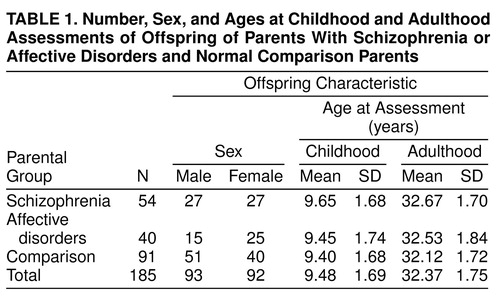
The subjects of this report are members of the initial sample (sample A) of the two-sample longitudinal New York High-Risk Project, which is described fully elsewhere (21, 22). This report is based on data for offspring of schizophrenic, affectively disordered, and normal comparison parents who were available for assessment at two measurement times: 1) in childhood, at a mean age of 9.48 years, and 2) in adulthood, at a mean age of 32.37 years.
The mentally ill parents were ascertained through records of patients consecutively admitted to six hospitals in New York state. Patients who were married, were white, spoke English, passed diagnostic exclusion criteria, and had at least one child between the ages of 7 and 12 were eligible for the study. Subsequent diagnostic assessments of these parents were made by using the Schedule for Affective Disorders and Schizophrenia—Lifetime Version (SADS-L) (23) and the Research Diagnostic Criteria (RDC) (24). Normal comparison families were secured through school systems that were chosen to reflect the characteristics of the community from which the patient parents came. Parents in these families were screened to ensure that they had not received or required treatment for a psychiatric disorder. In all groups, the offspring were free of psychiatric impairment at intake into the study (1971–1972). After complete description of the study to the subjects, written informed consent was obtained. Table 1 displays the numbers, ages, and gender composition of the 185 sample A subjects present for the two measurement times. (Of 188 subjects with adulthood follow-up, three who missed part of the childhood assessment are not included in these analyses.)
Measures
Parents’ report on behavioral problems in childhood
At the first round of testing in 1971–1972, a parent interview, concerned with early life characteristics of the offspring, was administered to the well parent in the groups with mentally ill parents and usually to the mother in the group of normal comparison subjects. The items of this interview were submitted to a principal components analysis, and the factors were rotated to simple structure by using the OBLIMIN oblique rotation (25). Rotation of different numbers of factors was investigated, and a two-factor solution was considered the most interpretable. The first factor reflects the parents’ reports of childhood behavior, while the second indicates when developmental milestones occurred. Behavioral items were scored in the direction of no problems; therefore, high values indicate good childhood behavior. In an earlier investigation (26), the same factor was used as a mediating variable in a path analysis model. For this report, the items of the behavior factor with a loading greater than 0.45 were summed to create a composite variable called “childhood behavior.” The highest-loading items that met this criterion were 1) Are there any behavior or discipline problems at home? 2) Has child always gotten along well with brothers and sisters? 3) Has child fought much with others? 4) Has child had temper tantrums? 5) Has child always gotten along well with others? These items measure presence or absence, and some are based on ordinal scores (0–2). We cannot attach a meaning to a score, but we can compare direction and magnitude on composite variables. Low scores represent more behavioral problems, and high scores represent few behavioral problems.
The mean score for the 185 subjects in this analysis for “childhood behavior” was 6.67 (SD=1.60; minimum=1.00, maximum=8.00). The childhood behavior variable mainly represents externalizing behaviors. Items reflecting other behavioral domains, such as social withdrawal (e.g., Does child usually prefer to play with other children or alone? Does child have any best friends?), did not yield sufficiently high loadings and therefore could not be included in the behavior variable used in this investigation.
Diagnostic assessment of the offspring
Lifetime RDC diagnoses (24) of adulthood axis I disorders were assigned on the basis of SADS-L interviews (23) administered on three separate occasions (for details, see references 22 and 27). For this paper, a hierarchical variable for clinical outcome was defined as follows: 1) schizophrenia-related psychoses, including schizophrenia, mainly schizophrenic schizoaffective disorder, and unspecified psychosis; 2) internalizing disorders, including psychotic and nonpsychotic affective disorders (mainly affective schizoaffective disorder, major depression, bipolar I disorder, bipolar II disorder, hypomania, and intermittent depression), anxiety disorders (generalized anxiety disorder, panic disorder, phobic disorder), or both; or 3) substance abuse only (drug and/or alcohol abuse with no other comorbid disorder) or no psychiatric disorder.
On the basis of findings from earlier studies, we had the following hypotheses:
1. Offspring of schizophrenic parents were expected to have a higher rate of childhood behavioral problems than offspring of normal comparison parents.
2. Subjects who developed schizophrenia-related psychoses were expected to have had more childhood behavioral problems than those with affective and/or anxiety disorders and those with substance abuse only or no disorder.
3. Subjects with substance abuse were expected to have had more childhood behavioral problems than those without substance abuse.
Statistical analysis
For these analyses, we studied 185 subjects who had both complete parental reports of childhood behavior and follow-ups yielding adulthood clinical diagnoses. For comparisons of adulthood clinical outcome by parental diagnostic group and of substance abuse by clinical outcome group, we calculated chi-square statistics, applying Fisher’s exact test when cell sizes were small. We applied simple factorial analysis of variance (ANOVA) (28), using childhood behavior as the dependent variable. Where appropriate, the Tukey honestly significant difference test (28) with adjustment for multiple comparisons was used to examine group differences. A significance level of 0.05 was used for all statistical tests, and two-tailed tests were applied.
RESULTS
Adulthood Clinical Outcome and Parental Diagnosis
Schizophrenia occurred only in the offspring of schizophrenic parents, and the rate of schizophrenia-related psychoses as a whole differed significantly between that group (18.5%, 10 of 54) and the offspring of the normal comparison parents (1.1%, one of 91) (p<0.001). The broad category of schizophrenia-related psychoses did not differ significantly between the offspring of the schizophrenic and affective disorders groups because of the high rate of schizoaffective disorder in the offspring of the affectively disordered parents (10.0%, four of 40). However, it did significantly distinguish the offspring of the affectively disordered parents and the offspring of the normal comparison parents (p=0.03). The other clinical outcome categories did not differ in the three parental diagnostic categories.
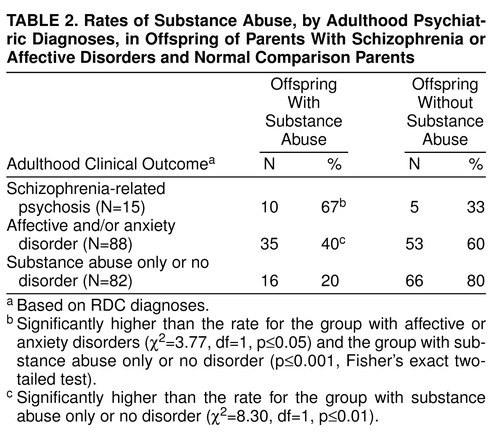
Adulthood Clinical Outcome and Substance Abuse
Table 2 shows the rates of substance abuse in each of the adulthood outcome categories (schizophrenia-related psychoses, affective and/or anxiety disorders, and substance abuse only or no disorder). The rates of substance abuse were significantly higher in both the group with schizophrenia-related psychoses and the group with affective and/or anxiety disorders than in the group with substance abuse only or no disorder. Additionally, the difference between the groups with schizophrenia-related psychoses and with affective and/or anxiety disorders was significant.
Childhood Behavior and Parental Diagnosis
We expected higher rates of childhood behavioral problems in the offspring of schizophrenic parents than in the offspring of parents with affective disorders or offspring of normal comparison subjects. The mean scores for childhood behavior were as follows: offspring of schizophrenic parents, 6.30 (SD=1.63); offspring of parents with affective disorders, 6.68 (SD=1.55); and offspring of normal comparison parents, 6.89 (SD=1.58). Lower scores reflect a greater number of behavioral problems reported by the parents. A one-way ANOVA for the parental diagnostic groups showed no group differences (F=2.38, df=2, 182, p=0.10).
Childhood Behavior and Adulthood Clinical Outcome
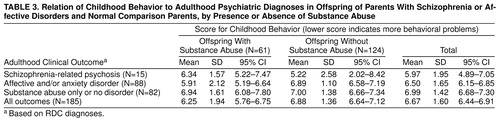
Table 3 shows childhood behavior scores in relation to adulthood clinical outcome, by presence or absence of substance abuse.
A three-way ANOVA using childhood behavior as the dependent variable and clinical outcome, substance abuse, and gender as the independent variables yielded a significant main effect for clinical outcome (F=4.97, df=2, 173, p=0.008), with schizophrenia-related psychosis having the lowest mean score for childhood behavior, and a significant interaction between clinical outcome and substance abuse (F=4.18, df=2, 173, p=0.02). Inspection of the mean scores for childhood behavior for the subjects with substance abuse showed no differences between the clinical outcome groups, while the mean scores for the subjects without substance abuse showed systematic differences. Therefore, we examined the differences in childhood behavior for the clinical outcome groups after excluding subjects with substance abuse from all diagnostic categories. We pooled across gender since it had neither a significant main effect nor an interaction with any of the other variables. After exclusion of the subjects with substance abuse, a one-way ANOVA with clinical outcome as the independent variable indicated that childhood behavior significantly differentiated the outcome groups (F=4.20, df=2, 121, p=0.02). Tukey honestly significant difference pairwise multiple comparison tests supported our hypothesis that subjects who developed adulthood schizophrenia-related psychoses displayed significantly more behavioral problems in childhood than those with adulthood affective and/or anxiety disorders (p=0.02) or those with substance abuse only or no disorder (p=0.01).
To address the question of the specificity of childhood problem behaviors that are associated with schizophrenia versus those associated with internalizing disorders, we performed chi-square analyses on the individual items composing the childhood behavior variable. We found no significant difference for any of the behavior items between the group with adulthood schizophrenia-related psychoses and the group with affective and/or anxiety disorders.
DISCUSSION
The New York High-Risk Project provided a rare opportunity to examine possible differences among the three parental risk groups with respect to childhood behavioral disturbances and, more important, the relationship between such disturbances and different psychiatric outcomes in adulthood. It is essential to note, however, that as core schizophrenia occurred only in the offspring of schizophrenic parents and the even broader category of schizophrenia-related psychoses was very rare (1.1%) in the normal comparison group (22, 27)), no inferences can be drawn about a predictive relationship between childhood behavioral problems and later development of these diagnoses in the general population. This caution is not applicable to the other outcome categories, whose rates did not differ in the three parental risk groups.
Although the hypothesized differences between the parental risk groups with respect to childhood behavior problems were not found, several other significant relationships did emerge, especially when the influence of substance abuse was taken into account. While substance abuse showed a significant interaction with our outcome groups, it is notable that in the group with adulthood schizophrenia-related psychoses, childhood behavioral problems were greater among subjects without substance abuse (mean score=5.22) than those with comorbid substance abuse (mean score=6.34). (Lower scores reflect more behavioral problems.) Carpenter and colleagues (29) have described a deficit form of schizophrenia, in which low rates of substance abuse and early manifestation of the disorder are typical. Our subjects with adulthood schizophrenia-related psychoses but no substance abuse, who exhibited the most marked behavioral abnormalities in childhood, might have such a deficit form of schizophrenia. To investigate group differences in schizophrenia-related psychoses, we looked at the ages at onset of psychosis in subjects with and without substance abuse. The mean ages at onset in the subjects with schizophrenia-related psychoses with substance abuse and schizophrenia-related psychoses without substance abuse were 21.30 years (SD=5.25) and 17.60 years (SD=3.65), respectively. However, to be less speculative, we would need to rate our subjects with schizophrenia-related psychoses for the deficit syndrome. In the other outcome groups (affective/anxiety disorders and substance abuse only or no disorder), as shown in table 3, more behavioral problems in childhood were exhibited by subjects with substance abuse than by those without.
Our findings show considerable consistency with the results of prior investigations on behavioral problems as antecedents to schizophrenia (e.g., references 7, 30, and 31) and research pointing to childhood behavioral problems as precursors of the onset of substance use during adolescence (17), substance use disorders generally (15, 16, 32), and alcoholism specifically (e.g., references 33 and 34). The need for more investigation into the relationships among childhood behavioral problems, substance abuse, and other psychiatric outcomes is demonstrated by 1) our finding of significant interactions among these three dimensions and 2) the observation that subjects without substance abuse who later developed schizophrenia-related psychoses had significantly more childhood behavioral problems than those who developed affective and/or anxiety disorders or no mental disorder.
One possible limitation of the analyses could be the exclusive reliance on parents as a source of data on childhood behavior. While data from additional sources might have improved the validity of these assessments, the parental ratings reflect the subjective attitude of the parent toward the child and may be considered to provide information about the parent-child interaction and, thus, the family climate in which the child was brought up. The factor reflecting childhood behavior, based on parental ratings, has been used previously in the New York High-Risk Project in an examination of the relationship of life-history variables to various pathological outcomes (26). That analysis revealed a negative relationship between a high score on the factor (reflecting good child behavior) and hospitalization for psychiatric disorders by a mean age of 27, indicating that subjects with a low frequency of childhood behavioral problems are unlikely to be hospitalized for mental disorder in young adulthood. The results presented here give further and stronger evidence of a remarkable degree of continuity over a long time period involving both a major change in environment and multiple life transitions. Teachers’ reports (30) have also been shown to constitute an important and reliable source of information on childhood behavior. Although our data examined here came from the parents, an earlier New York High-Risk Project report noted that teachers’ ratings of problem behavior in school (20) described young adolescent subjects at risk for schizophrenia as “unpleasant, unpopular, negativistic, maladjusted, nervous and low motivated” compared with normal comparison subjects. Thus, teachers’, as well as parents’, reports have indicated a higher frequency of behavioral problems in the offspring of schizophrenic parents than in the normal comparison children in this sample.
Another potential limitation of these analyses is that externalizing behavioral problems may be an overt expression of different underlying etiopathic entities linked to different developmental pathways and disorders and that the childhood behaviors considered here are rather crude and unspecific. However, these behaviors were not chosen arbitrarily but were derived from a factor analysis, and our results are consistent with well-established findings from child psychiatric studies (35 showing that parents can more reliably detect externalizing behaviors than internalizing processes or more complex features, such as social competence. Also important to point out is that the childhood behavior variable does not relate to the concept of conduct disorder in childhood, which is characterized by antisocial and aggressive behavior (36). Thirteen subjects (7%) from our sample here received the diagnosis of “conduct disorder in their past” during the first diagnostic follow-up in the New York High-Risk Project, when they were in their early 20s. Their mean score for childhood behavior (7.08) did not differ from the mean for the group with substance abuse only or no disorder. However, only one of those subjects developed schizophrenia-related psychosis with comorbid substance abuse, four were diagnosed with affective disorder and substance abuse, one was diagnosed with pure substance abuse, one was diagnosed with affective and anxiety disorders, and six did not develop any adulthood psychiatric disorder.
Nonwhites were not part of the original samples in the New York High-Risk Project, which were obtained at the beginning and middle of the 1970s. Our conclusions are thus limited to Caucasian (white) populations. Also, as noted earlier, the findings with respect to schizophrenia-related psychoses cannot be generalized beyond the offspring of schizophrenic parents.
In summary, our results support the view that in offspring of schizophrenic parents, schizophrenia-related psychoses can be followed back to early disturbances and suggest that childhood behavioral problems have links to adulthood psychopathology. At this point it remains to be explored whether the types of childhood behavioral disturbances considered here are related to other dysfunctions, such as attentional deviance and affective abnormalities, which have previously been reported to distinguish subjects at high risk for schizophrenia and preschizophrenic persons from normal comparison subjects. However, regardless of parental risk group, children characterized by early behavioral dysfunction also seem to be more likely to develop other psychiatric disorders in adulthood than subjects free of such childhood problems.
Received May 13, 1998; revised Sept. 24, 1998; accepted Oct. 6, 1998. From the University Hospital for Child and Adolescent Neuropsychiatry, University of Vienna, Austria; and the Department of Medical Genetics, New York State Psychiatric Institute, New York. Address reprint requests to Dr. Amminger, University Hospital for Child and Adolescent Neuropsychiatry, Waehringer Guertel 18-20, A-1090 Vienna, Austria; [email protected] (e-mail). Supported in part by NIMH grant MH-19560 to Dr. Erlenmeyer-Kimling and by NIMH grant MH-20906 to the Clinical Research Center, New York State Psychiatric Institute.
 |
 |
 |
1. Weinberger DR: Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry 1987; 44:660–669Crossref, Medline, Google Scholar
2. Jones P, Done DJ: From birth to onset: a developmental perspective of schizophrenia in two national birth cohorts, in Neurodevelopment and Adult Psychopathology. Edited by Keshavan MS, Murray RM. New York, Cambridge University Press, 1997, pp 119–136Google Scholar
3. Pogue-Geile MF: Developmental aspects of schizophrenia. Ibid, pp 137–154Google Scholar
4. Baum KM, Walker EF: Childhood behavioral precursors of adult symptom dimensions in schizophrenia. Schizophr Res 1995; 16:111–120Crossref, Medline, Google Scholar
5. Roff JD, Knight R, Wertheim E: A factor-analytic study of childhood symptoms antecedent to schizophrenia. J Abnorm Psychol 1976; 85:543–549Crossref, Medline, Google Scholar
6. Lewine RRJ, Watt N, Prentky RA, Fryer JH: Childhood behavior in schizophrenia, personality disorder, depression, and neurosis. Br J Psychiatry 1978; 133:347–357Crossref, Medline, Google Scholar
7. Watt NF: Patterns of childhood social development in adult schizophrenics. Arch Gen Psychiatry 1978; 35:160–165Crossref, Medline, Google Scholar
8. Done DJ, Crow TJ, Johnstone EC, Sacker A: Childhood antecedents of schizophrenia and affective illness: social adjustment at ages 7 and 11. BMJ 1994; 309:699–703Crossref, Medline, Google Scholar
9. Jones P, Rodgers B, Murray R, Marmot M: Child development risk factors for adult schizophrenia in the British 1946 birth cohort. Lancet 1994; 344:1398–1402Crossref, Medline, Google Scholar
10. Roff M: Some life history factors in relation to various types of adult maladjustment, in Life History Research in Psychopathology, vol 1. Edited by Roff M, Ricks DF. Minneapolis, University of Minnesota Press, 1970, pp 265–287Google Scholar
11. Woerner M, Pollack M, Rogalski C, Pollack Y, Klein D: A comparison of the school records of personality disorders, schizophrenics, and their sibs, in Life History Research in Psychopathology, vol 2. Edited by Roff M, Robins LN, Pollack M. Minneapolis, University of Minnesota Press, 1972, pp 47–65Google Scholar
12. Champion LA, Goodall G, Rutter M: Behaviour problems in childhood and stressors in early adult life, I: a 20 year follow-up of London school children. Psychol Med 1995; 25:231–246Crossref, Medline, Google Scholar
13. Robins LN: Deviant Children Grown Up. Baltimore, Williams & Wilkins, 1966Google Scholar
14. Robins LN, Price RK: Adult disorders predicted by childhood conduct problems: results from the NIMH Epidemiologic Catchment Area project. Psychiatry 1990; 54:116–132Google Scholar
15. Lynskey MT, Fergusson DM: Childhood conduct problems and attention deficit behaviors, and adolescent alcohol, tobacco, and illicit drug use. J Abnorm Child Psychol 1995; 23:281–302Crossref, Medline, Google Scholar
16. Mässe LC, Tremblay RE: Behavior of boys in kindergarten and the onset of substance use during adolescence. Arch Gen Psychiatry 1997; 54:62–68Crossref, Medline, Google Scholar
17. Drake RE, Mueser KT, Clark RE, Wallach MA: The course, treatment, and outcome of substance disorder in persons with severe mental illness. Am J Orthopsychiatry 1996; 66:42–51Crossref, Medline, Google Scholar
18. Dixon L, McNary S, Lehman AF: Remission of substance use disorders among psychiatric inpatients with mental illness. Am J Psychiatry 1998; 155:239–243Abstract, Google Scholar
19. Watt NF, Anthony EJ, Wynne LC, Rolf J (eds): Children at Risk for Schizophrenia: A Longitudinal Perspective. New York, Cambridge University Press, 1984Google Scholar
20. Watt NF, Grubb TW, Erlenmeyer-Kimling L: Social, emotional, and intellectual behavior at school among children at high risk for schizophrenia. J Consult Clin Psychol 1982; 50:171–181Crossref, Medline, Google Scholar
21. Erlenmeyer-Kimling L, Cornblatt B: The New York High-Risk Project: a follow-up report. Schizophr Bull 1987; 13:451–461Crossref, Medline, Google Scholar
22. Erlenmeyer-Kimling L, Squires-Wheeler E, Hilldoff Adamo U, Bassett AS, Cornblatt BA, Kestenbaum CJ, Rock D, Roberts SA, Gottesman II: The New York High-Risk Project: psychoses and cluster A personality disorders in offspring of schizophrenic parents at 23 years of follow-up. Arch Gen Psychiatry 1995; 52:857–865Crossref, Medline, Google Scholar
23. Spitzer RL, Endicott J: Schedule for Affective Disorders and Schizophrenia—Lifetime Version, 3rd ed. New York, New York State Psychiatric Institute, Biometrics Research, 1979Google Scholar
24. Spitzer RL, Endicott J, Robins E: Research Diagnostic Criteria (RDC) for a Selected Group of Functional Disorders, 3rd ed. New York, New York State Psychiatric Institute, Biometrics Research, 1978Google Scholar
25. SPSS-X User’s Guide, 3rd ed. Chicago, SPSS, 1988, pp 480–498Google Scholar
26. Erlenmeyer-Kimling L, Rock D, Squires-Wheeler E, Roberts S, Yang J: Early life precursors of psychiatric outcomes in adulthood in subjects at risk for schizophrenia or affective disorders. Psychiatry Res 1991; 39:239–256Crossref, Medline, Google Scholar
27. Erlenmeyer-Kimling L, Hilldoff Adamo U, Rock D, Roberts SA, Bassett AS, Squires-Wheeler E, Cornblatt BA, Endicott J, Pape S, Gottesman II: The New York High-Risk Project: prevalence and comorbidity of axis I disorders in offspring of schizophrenic parents at 25-year follow-up. Arch Gen Psychiatry 1997; 54:1096–1102Crossref, Medline, Google Scholar
28. SPSS Base 7.5 for Windows User’s Guide. Chicago, SPSS, 1997Google Scholar
29. Carpenter WT Jr, Heinrichs DW, Wagman AMI: Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry 1988; 145:578–583Link, Google Scholar
30. Olin SS, John RS, Mednick SA: Assessing the predictive value of teacher reports in a high risk sample for schizophrenia: a ROC analysis. Schizophr Res 1995; 16:53–66Crossref, Medline, Google Scholar
31. Parnas J, Schulsinger F, Schulsinger H, Mednick SA, Teasdale TW: Behavioral precursors of schizophrenia spectrum: a prospective study. Arch Gen Psychiatry 1982; 39:658–664Crossref, Medline, Google Scholar
32. Ohannessian CM, Stabenau JR, Hesselbrock VM: Childhood and adulthood temperament and problem behaviors and adulthood substance use. Addict Behav 1995; 20:77–86Crossref, Medline, Google Scholar
33. Hesselbrock MN: Childhood behavior problems and adult antisocial personality disorder in alcoholism, in Psychopathology and Addictive Disorders. Edited by Meyer RD. New York, Guilford Press, 1986, pp 78–94Google Scholar
34. Cloninger CR, Sigvardsson S, Bohman M: Childhood personality predicts alcohol abuse in young adults. Alcohol Clin Exp Res 1988; 12:494–505Crossref, Medline, Google Scholar
35. Cox AD: Interviews with parents, in Child and Adolescent Psychiatry: Modern Approaches, 3rd ed. Edited by Rutter M, Taylor E, Hersov L. Cambridge, Mass, Blackwell Science, 1994, pp 22–33Google Scholar
36. Robins LN: Conduct disorder. J Child Psychol Psychiatry 1991; 32:193–212Crossref, Medline, Google Scholar



