Randomized Trial of Psychiatric Care With Representative Payeeship for Persons With Serious Mental Illness
Abstract
OBJECTIVES: This randomized clinical trial assessed whether a community-based representative payee program that was coordinated with psychiatric care from the Department of Veterans Affairs was more effective than customary treatment. METHODS: In the experimental condition representative payeeship was provided by a community agency that worked to enroll clients and coordinate payeeship with clinical care through communication with clinical staff. The control condition consisted of customary clinical care that included the typical availability of representative payeeship. Hypotheses were that, compared with the control group, the experimental group would experience greater enrollment in a representative payee program; improved residential status; improved quality of life, including fewer symptoms of mental illness; less substance abuse; and improved money management. Participants were interviewed at baseline and at six and 12 months. Outcomes were analyzed with analysis of covariance by using covariates from the baseline. RESULTS: A total of 184 participants were enrolled at baseline (94 in the experimental group and 90 in the control group). A total of 152 interviews were completed at six months, and 149 were completed at 12 months. At 12 months, 31 percent of patients in the experimental group and 14 percent of those in the control group were receiving representative payee services. At 12 months, significant positive effects were observed for the experimental group on enrollment in a representative payeeship, alcohol and drug use, quality of life, and money management. Residential status approached significance. CONCLUSIONS: Use of a coordinated representative payee program was found to be effective in improving outcomes at 12 months. Although this evidence supports the wider implementation of a coordinated representative payee program, only 31 percent of the experimental group had their money banked with a representative payee. Therefore, future studies should focus on achieving a better understanding of the causal components of the intervention.
Money management in the form of representative payeeship for persons with severe mental illnesses has been suggested to be an effective strategy to support stable community living. For example, Luchins and colleagues (1) provided recent reviews of the clinical issues, and Monahan and colleagues (2) reviewed the legal issues that are involved in a majority of cases in which money management is involuntary. Put briefly, money management may serve as a linchpin in the service system, because lack of money can result in consequences such as the inability to pay for food and medicine, which can then lead to exacerbations of health problems, criminal activity to obtain money, inability to pay rent, and, ultimately, homelessness or institutionalization.
The problem is that, without help, some psychiatric patients may misuse or waste their money because of personal vulnerability factors, such as delusions, cognitive and perceptual impairments, lack of skills, impulsive behavior, and susceptibility to victimization. Social vulnerability factors influence livelihood as well. These factors include lack of positive supports from family and friends and a lack of community resources. Oftentimes, family, friends, and the community may actually have negative effects on the livelihood of persons with severe mental illness.
This randomized controlled trial was conducted in a medical center of the Department of Veterans Affairs (VA) that had a pilot program that involves the coordination of its community treatment program with a representative payee program that was provided by a non-VA community agency. Although housing provision was not part of the program, the key to improved residential status was hypothesized to be the coordination between the representative payee agency and VA staff, first to achieve representative payeeship and subsequently to pay rent and other bills. Clients who were receiving care from the VA were either self-referred or referred by providers to volunteer for random assignment to one of two conditions. The experimental condition consisted of representative payeeship provided by a community agency called Independent Positive Living Under Supervision (I-PLUS). I-PLUS then worked proactively to enroll clients and coordinate payeeship with clinical care through communication with clinical staff. The control condition consisted of customary clinical care that included the typical availability of representative payeeship. However, in the control condition the representative payee program was not provided by I-PLUS and was not coordinated with clinical care. More background and details of the intervention are described below and may be found in other sources (3,4) or from the first author.
Pransky's "risk and protective factors" model (5) notes the importance of resource limitations and victimization as risk factors for homelessness. The importance of resources was further supported by Herman and colleagues (6), whose interviews with persons who had episodes of homelessness and mental illness reported needs for managing money, obtaining VA benefits, addressing legal issues, and finding housing. Studies of representative payee programs have tended to evaluate other outcomes in addition to homelessness, such as hospitalization (7,8), service use (8,9), and substance use (10,11,12).
Very few studies have examined the role of mental health agencies as providers of representative payee services. One descriptive study has been identified in which staff of a mental health agency functioned as payees for 89 individuals with mental illness (13). More than half the group had either been a crime victim or been arrested in the year before enrollment. By using data collected over one year, several findings were positive: 77 percent reported no days of homelessness, 82 percent were living within their monthly allocation after a year in the program, 9 percent had been crime victims since enrollment, and 9 percent had been arrested. Staff ratings also indicated an increase in cooperation with treatment.
An assessment of the representative payee program offered at Community Counseling Centers of Chicago followed 56 individuals with severe mental illness who were enrolled in the representative payee program for one year and had one year of previous service use data (13). Compared with the year before enrollment, the year after enrollment showed a markedly decreased average number of days spent in state hospitals, from a mean±SD of 66±105 days to a mean of 7±17 days (p<.001). Although a rigorous study design was lacking, the findings suggested that the representative payee program was effective in reducing hospital stays.
Recently, Tsemberis and colleagues (14) studied a housing first model that included money management and counseling. The findings were positive for housing stability, but the study did not examine the effects of money management and the effects of counseling separate from housing provision.
Methods
Study aim
The aim of our study was to determine, in a randomized clinical trial, whether a community-based representative payee program that was coordinated with VA psychiatric community care was more clinically effective than customary treatment for veterans who had no representative payee or representative payeeship that was not coordinated with their care. Institutional review board approval for the study was obtained from the Hines VA Hospital and North Chicago VA Medical Center's human subjects subcommittee and from the University of Illinois at Chicago's Office for the Protection of Research Subjects.
Participants
A total of 184 participants met the criteria for enrollment in a representative payee program. The first criterion was need for the program. Need mainly focused on risk of homelessness as a result of money management problems and was determined by using the Determination of Need for Representative Payeeship scale (15), which was assessed by 12 risk and need characteristics. Other criteria for enrollment included presence of a serious mental illness as assessed with the Severity of Psychiatric Illness scale, possibly with a co-occurring substance use disorder (16,17,18), and engagement with the VA mental health treatment system.
Usual care
Although the Veterans Benefits Administration of the VA has a money management system in place called the Fiduciary Program, this program serves only a fraction of the patients who need it. VA clinicians may use informal strategies for managing the money of the many patients outside the Fiduciary Program, and a few patients have a VA hospital director as their representative payee (5). Outside the VA, the Social Security Administration (SSA) may require that some persons have a representative payee as a condition of receiving SSA checks, and some persons may voluntarily and independently set up a type of representative payee relationship with a family member or friend.
The coordinated representative payee program
The psychiatry service at North Chicago VA Medical Center developed a pilot program that combined traditional psychiatric case management with financial services offered by a community-based, nonprofit representative payee agency called Independent Positive Living Under Supervision (I-PLUS). The goal was to make money management an integral component of patient care. The coordination of representative payeeship with clinical care to improve enrollment and awareness of the program were viewed as the key to success. This coordination did not involve any formal incentives or a quid pro quo system involving treatment adherence. Rather, it involved voluntary patient enrollment and mutual recognition and communication between the patient, case manager, and representative payee about the issues of good money management in promoting successful treatment and recovery. In contrast, members of the control group had case management, which could refer them to a representative payee. However, in the control group, the representative payee program was not provided by the I-PLUS agency and was not coordinated with clinical care.
Because participation in the study was voluntary, so was participation in the coordinated representative payee program. Achieving adherence to clinical recommendations was by no means easy, because enrollment took several months and many countervailing influences existed. For example, some clients had become habituated to using the shelter system for housing and the VA as an emergency treatment facility. In this way, they could avoid the high cost of housing and use their benefit funds for other priorities.
The ultimate aim of the coordinated representative payee program was to help adults with severe mental illness maintain stable community residence in "normal" housing—that is, principally their own apartments. When appropriate, the program also sought to help patients become more financially autonomous by providing training, offering support, and gradually decreasing the I-PLUS agency's role. In addition, both the agency and VA staff assumed a "protector" role, to help reduce the incidence of financial victimization of adults with severe mental illness. Details of the intervention are available elsewhere (4,5) or by contacting the lead author.
Enrollment process
The enrollment process started with providing psychiatry staff with information about the availability of the coordinated representative payee program. Patients were referred by staff or were self-referred in response to announcements in wards or clinics. After informed consent was obtained, all volunteers were interviewed for the study and randomly assigned. Those assigned to the experimental group were referred for an intake interview with a staff person from I-PLUS. Patients assigned to the control group were referred to their case manager, who could help them obtain a representative payee through the usual channels, but not with the I-PLUS agency.
I-PLUS took a proactive role in attempting to enroll clients within two weeks of the baseline interview. I-PLUS staff worked with VA staff as needed to promote enrollment in the coordinated representative payee program. Once participants were enrolled in the program, I-PLUS staff worked with VA staff toward achievement of stable housing with ongoing payment of rent.
Hypotheses, rationale, and outcome measures
Interviews were conducted at baseline and six and 12 months after study enrollment. All outcomes were analyzed with one-tailed tests, because the effectiveness of coordinated representative payeeship was hypothesized to be greater than the effectiveness of usual care. The randomized clinical trial assessed whether, compared with the control group, the experimental group had the outcomes described below.
More frequent enrollment in a representative payee program. Participants in the experimental group were said to have been enrolled in the coordinated representative payee program if their VA benefit, social security, or employment check was successfully banked at I-PLUS and if I-PLUS was designated as their representative payee. Participants in the control group self-reported whether they had a representative payee and the type of representative payee—for example, family, friend, or nursing home.
Improved housing stability. Housing stability is a prerequisite for other improved outcomes, such as reduced hospitalization and improved quality of life. The Residential Follow-Back Calendar (RFBC) was used to assess housing over the six months before baseline and the six and 12 months after baseline. The RFBC has been successfully used for this purpose (19). In a Substance Abuse and Mental Health Services Administration cooperative agreement, two-week retests were conducted on individual RFBC variables with 151 to 158 participants, in which days literally homeless had a test-retest correlation of .90.
Improved health-related quality of life, including less mental illness symptoms. Coordinated representative payeeship was expected to have a direct effect on general quality of life because being housed, fed, and stabilized psychiatrically are basic components of this construct. Participants' perceived quality of life was assessed by asking, "How do you feel about your life in general?" This question was asked at the beginning and end of each interview. Responses were measured on a 7-point scale, with answers ranging from "terrible" to "delighted." This question and the 7-point scale were adapted from a previous investigation of quality of life (20). This measure of life satisfaction was computed by averaging each participant's responses to the two questions. If a response to one of the items was missing, it was replaced by the remaining valid response.
We posited a link between money management and reduced mental health symptoms, because it is plausible that the lifestyle improvements noted above—improved adherence to treatment regimens promoted by coordinated representative payeeship and the removal of stressors related to the inability to manage money—would have a beneficial effect on mental health. To assess these potential benefits, we used the Colorado Symptom Index (21), which was found to have Cronbach's alphas averaging .9 across eight projects that served persons who had mental illness and a substance use disorder and were at risk of homelessness (22). Analyses supported the construct validity of the Colorado Symptom Index as a measure of symptom severity.
Less substance abuse and dependence. We used the Timeline Follow-Back (TLFB) calendar method to document substance use in the previous six months (23). The TLFB has been found to have substantial retest reliability estimates in populations of alcoholics in outpatient and inpatient care who are veterans—for example, scores of .85, .94, and .94, respectively, on number of days abstinent (23). On cross-validation tests of participant and collateral reports, correlations ranged from .79 to .92 on abstinence in six studies (23). Alcohol use was reported in drinking days over the past three months, and drug use was reported in months of drug use over the past six months. For example, if cocaine was used at all during each of the previous six months and marijuana was used in two of those months, the total number of drug months would be eight.
Improved money management. The client's risk of financial instability is the primary reason for the existence of a representative payee program. The representative payee obtains financial control because clients are unable to maintain financial stability on their own. We developed the Money Mismanagement Measure to assess problems handling one's money and financial exploitation. The final version of the measure consisted of 22 items with an alpha of .87 and strong indicators of construct validity (24).
Enrollment and original timeline
After a three month start-up, the goal of the project was to enroll and randomly assign 240 participants to the experimental and control conditions over 20 months. The project began on January 1, 2001, and enrollment began on time in April 2001. However, only one person enrolled in that month. We quickly learned that our goal of enrolling 12 patients per month for 20 months would be difficult to achieve. In the end we enrolled 184 patients (77 percent of the target). Ninety-four were in the experimental group, and 90 were in the control group. Enrollment was closed at the end of February 2003. An average of eight participants were enrolled per month for 23 months, rather than the planned 12 participants per month for 20 months.
Analysis plan
All analyses were done with the SPSS for Windows (25) statistical analysis program. We report the findings for participants at the six- and 12-month observation points.
Baseline comparability. The baseline comparability analysis included demographic characteristics and psychosocial variables, such as mental health symptoms, employment, history of drug and alcohol use, residential history, residential status, substance use, quality of life, income sources, and insurance coverage. In total, this amounted to 102 individual variables.
Analysis of covariance. Even if the groups were similar at baseline, they could become different after baseline because of differential attrition. To control for this possibility, analysis of covariance (ANCOVA) was used in the posttest analyses. For this analysis, the study groups were dummy coded as 0 for the control group and 1 for the coordinated representative payee group. Each dependent variable was also regressed on the baseline assessment of that same variable used as a covariate and on the baseline assessment of severity of psychiatric illness (16,17,18) and determination of need for a representative payee (15). Theoretically, the best baseline predictor would be the baseline assessment of the dependent variable. Psychiatric severity and need for a representative payee were also judged to be generally useful predictors of the study variables because they would tend to be correlated with the variables.
Post hoc analysis of covariance. A post hoc analysis of covariance that used the same covariates as above was performed to compare the performance of patients in the experimental group who enrolled in the coordinated representative payee program (reference group) with the performance of those in the experimental group who did not enroll in the program as well as with the performance of those in the control group. The post hoc analysis was done only on the 12-month follow-up because it included the full observable effect of the treatment.
Results
Baseline comparability
Individual t tests indicated that random assignment was successful in making the groups comparable. Of the 102 variables that were analyzed, only four (hours worked in the past week, age at first psychiatric hospitalization, having Medicare in the past month, and having social security in the past month) indicated statistically significant differences between the groups (p<.05). This level is roughly the level of chance. Table 1 displays comparisons of the demographic characteristics of the two groups, and Table 2 displays several of the other key variables that were used in the baseline comparability analysis.
Six- and 12-month follow-up rates
A total of 184 participants were interviewed at baseline (94 in the coordinated representative payee group and 90 in the control group). Six-month interviews were completed for 152 participants (83 percent), and 12-month interviews were completed for 149 (81 percent). Eighty participants in the experimental group (85 percent) and 72 in the control group (80 percent) had complete data at both baseline and six months. Seventy-six participants in the experimental group (81 percent) and 73 in the control group (81 percent) had complete data at both baseline and 12 months.
Six-month enrollment findings
At six months, 24 patients in the experimental group (26 percent) were enrolled in I-PLUS. It typically took four or five months before a client's SSA or VA benefit check was banked at I-PLUS. Therefore, at six months clients had received only a month or two of full treatment.
At six months, 16 patients in the control group (18 percent) had a representative payee. Two patients used their wife as a representative payee, four used their mother, six used a family member, two used a VA hospital director, one used a Catholic charity, and one used an attorney. Significantly more persons in the experimental group had a representative payee, compared with those in the control group (p=.04, one-tailed).
Six-month outcomes
As shown in Table 3, at six months, the ANCOVA analysis provided significant findings on quality of life favoring the experimental group. The negative values indicate a decrease in the problem area for the experimental group. The positive value for quality of life indicates an increase favoring the experimental group. Although homelessness, alcohol use, and drug months were in the expected direction, they did not reach statistical significance.
Twelve-month enrollment findings
Twenty-nine members of the experimental group (31 percent) had enrolled in I-PLUS at 12 months. These participants had averaged about seven months in representative payeeship since their checks had been banked with I-PLUS. An additional two persons in the coordinated representative payee group (2 percent) had a representative payee that did not work through I-PLUS—that is, a family member or agency. For the 12-month analyses, only 25 persons who had banked with I-PLUS had complete data.
At 12 months, 13 members of the control group (14 percent) had a representative payee of some kind. Two used their wife as a representative payee, two used their mother, four used a family member, two used a hospital director of the VA, one used a nursing home, one used a bank, and one used an attorney. Significantly more persons in the experimental group had a representative payee, compared with those in the control group (p=.002, one-tailed). Clearly, the experimental group received more I-PLUS treatment and more representative payee services in general, regardless of the provider.
Twelve-month outcomes
As shown in Table 4, at 12 months, compared with the control group, the experimental group showed significant decreases in alcohol use, drug months, and money mismanagement and significant increases in quality of life. No significant difference was seen in homelessness or psychological symptoms, although the reduction in homelessness approached significance (p=.06).
Twelve-month post hoc outcomes.Table 5 displays the mean differences in 12-month outcomes between persons in the experimental group who enrolled in coordinated representative payeeship (reference group of persons who had banked money with I-PLUS), those in the experimental group who did not enroll in coordinated representative payeeship, and those in the control group. Most noteworthy is that the differences between the reference group and the control group were statistically significant, even though the size of the reference group was quite small (25 persons).
Discussion
At 12 months, the reduction in homelessness in the experimental group approached but did not reach statistical significance. This finding can be viewed as positive for a number of reasons. The significance criterion is sensitive to sample size; therefore, the same effect size (that is, 11 fewer days of being homeless in the previous six months) would be significant with a few more cases.
At 12 months significant differences in four of the other five outcomes were indicated by the ANCOVA results. This finding indicates that important issues that contribute to housing stability were being affected by coordinated representative payeeship. For example, compared with the control group, the experimental group had significantly reduced money mismanagement, and better money management facilitates paying rent. However, housing is less tractable than the other variables because it depends on the availability of low-income units and more preparation, involvement, and commitment of others. Also, lead time is required for a successful housing placement. Because the outcomes generally tended to improve from six to 12 months, we could only speculate that with more time in coordinated representative payeeship, members of the experimental group would have more housing stability. This hypothesis should be tested in future research.
An important aspect of the study is that even though all patients in the experimental group volunteered for the study, only 31 percent of the experimental participants actually enrolled and had their money banked with I-PLUS at 12 months. Meanwhile, about 14 percent of the patients in the control group self-reported money management of some sort. Despite the apparent low use of representative payee services in the experimental group, the ANCOVA results indicated that coordinated representative payeeship was effective. We do not know how extensive the services were that were offered by the coordinated representative payee program, such as level of communication about money management between the representative payee and case manager. We also do not know of the potential side effects of experimental group assignment—for example, whether persons in the experimental group who did not bank their money with I-PLUS modified their behavior because of the perceived threat of money management. The coordinated representative payeeship model holds that the collaboration of the VA clinical staff with the representative payee agency is the key ingredient that makes a difference in outcomes of patients with serious mental illness and a need for representative payeeship.
Unfortunately, examining certain key implementation issues more closely was beyond the scope of this study. For example, it would be important to see whether the coordination of the I-PLUS agency and clinical staff in attempting to enroll the clients heightened clinicians' awareness and clients' awareness of money management. This result would support the idea that coordination of care that includes a focus on money management is helpful in improving outcomes. It was expected that money management in the control group would be relatively ineffectual with potential for abuse, because nonprofessional representative payees would be less regulated and accountable than the I-PLUS agency, which worked with a cadre of VA case managers. However, examining this issue was beyond the scope of the current study.
The generalizability of the results is limited by the voluntary nature of the program. It was not possible to enroll everyone who was judged to need money management in the study. With a greater enrollment percentage, as would be the case in more typical mandated programs (2), it is likely that larger effects would have been observed (26). Also, the time lag of four or five months before the successful banking of benefit checks reduced the observable period of full treatment. However, our findings indicate that being involved in the process of banking funds and other ongoing therapeutic activities were beneficial.
In future work, it would be helpful to have substantial lead time to conduct an awareness campaign with clinicians and patients to let them know what coordinated representative payeeship is, answer their questions, and generally prepare clinicians to support the selection and referral of needy patients. This change in protocol could improve program implementation during the study period. As it was, we conducted the awareness campaign as the research project was implemented. This process gave the advantage of studying real-world implementation and its actual effectiveness. This study revealed that implementation of money management on a voluntary basis is difficult and merits further study. Very careful attention must be paid to communicating with both clinicians and patients about the sensitive issue of money management if coordinated representative payee programs are to be successfully implemented.
Conclusions
Although we thought that it would be difficult to enroll participants in a formal, coordinated representative payee program on a voluntary basis, our enrollment rate of 31 percent was somewhat less than we had expected. Even so, this enrollment rate was substantially more than that found in the control group. Even with rather modest implementation, psychiatric care coordinated with representative payeeship was found to be effective in reducing money mismanagement, decreasing alcohol and drug use, and improving quality of life over 12 months.
The coordinated representative payee intervention is relevant to the VA because it involved an enhancement to current treatment that is rarely used but is potentially available nationwide—for example, through agencies such as those used by the SSA. Also, coordinated representative payeeship requires modest additional resources, although it has the potential to promote the more appropriate use of benefits, improve the outcomes of care, and reduce use of more expensive services for a possible net reduction in costs. This study was the first to use a randomized controlled trial to study a representative payee program. As such, it provided evidence that supports wider implementation of the coordinated representative payee model as an alternative to promote improved residential stability for persons with severe mental illnesses. Future studies that focus on achieving a better understanding of the causal components of the intervention will be required.
Acknowledgments
This material is based on work supported by the VA Office of Research and Development, Health Services Research and Development Service under grant IIR98-154. Contributions from Atul Mahableshwarkar, M.D., Rolf Larson, M.S., and Kathy Batesky, B.S.N., were instrumental to the study.
Dr. Conrad and Dr. Matters are affiliated with the division of health policy and administration at the University of Illinois at Chicago School of Public Health, 2035 West Taylor Street, Chicago, Illinois 60612 (e-mail, [email protected]). Ms. Donner and Mr. Clark are with the Midwest Center for Health Services and Policy Research at the Hines Department of Veterans Affairs (VA) Hospital in Hines, Illinois, with which Dr. Conrad is also affiliated. Dr. Lutz is with the department of psychiatry at the North Chicago VA Hospital in North Chicago. Ms. Lynch is with Independent Positive Living Under Supervision in Waukegan, Illinois.
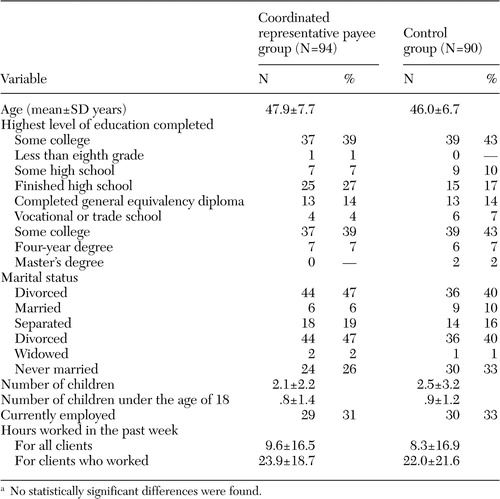 |
Table 1. Baseline demographic characteristics of veterans with serious mental illness and a need for representative payeeship, by study conditiona
a No statistically significant differences were found.
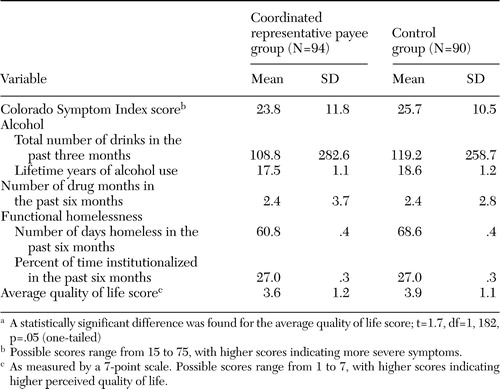 |
Table 2. Baseline clinical characteristics of veterans with serious mental illness and a need for representative payeeship, by study conditiona
a A statistically significant difference was found for the average quality of life score; t=1.7, df=1, 182, p=.05 (one-tailed)
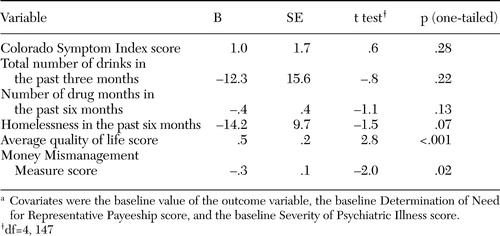 |
Table 3. Analysis of covariance results of the six-month outcomes of 80 veterans in the representative payee group and 72 in the control groupa
a Covariates were the baseline value of the outcome variable, the baseline Determination of Need for Representative Payeeship score, and the baseline Severity of Psychiatric Illness score.
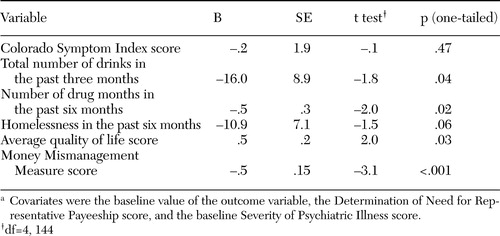 |
Table 4. Analysis of covariance results of the 12-month outcomes of 76 veterans in the representative payee group and 73 in the control groupa
a Covariates were the baseline value of the outcome variable, the Determination of Need for Representative Payeeship score, and the baseline Severity of Psychiatric Illness score.
 |
Table 5. Post hoc one-way analysis of variance with covariates comparing 12-month outcomes among persons in the experimental group who were enrolled in a coordinated representative payeeship program (reference group; N=25) with those of persons in the experimental group who were not enrolled (N=51) and those of a control group (N=73)a
a Means were adjusted by using the following covariates: baseline value of the outcome variable, the baseline Determination of Need for Representative Payeeship score, and the baseline Severity of Psychiatric Illness score. The mean difference is the adjusted mean for persons in the experimental group with coordinated representative payee minus, first, the adjusted mean for persons in the experimental group without coordinated representative payee, and, second, the adjusted mean for persons in the control group. All results were in the direction indicating benefit of being in the experimental group with a coordinated representative payeeship.
1. Luchins DJ, Roberts DL, Hanrahan P: Representative payeeship and mental illness: a review. Administration and Policy in Mental Health 30:341–353,2003Crossref, Medline, Google Scholar
2. Monahan J, Bonnie RJ, Appelbaum PS, et al: Mandated community treatment: beyond outpatient commitment. Psychiatric Services 52:1198–1205,2001Link, Google Scholar
3. Conrad KJ, Mahableshwarhar A, Lutz G, et al: Coordinating VA psychiatric community care with representative payeeship. Illinois Morbidity and Mortality Review, Special Issue: Veterans in the Community. Illinois Public Health Leadership Institute 3:24–29,1998Google Scholar
4. Conrad KJ, Mahableshwarkar A, Lutz G, et al: Helping patients with severe mental illness manage money. Federal Practitioner 20:32–54,2003Google Scholar
5. Pransky J: Prevention: The Critical Need. Springfield, Mo, Burrell Foundation, 1991Google Scholar
6. Herman DB, Struening EL, Barrow SM: Self-reported needs for help among the homeless men and women. Evaluation and Program Planning 17:249–256,1994Crossref, Google Scholar
7. Luchins D, Hanrahan P, Conrad KJ, et al: An agency-based representative payee program and improved community tenure of persons with mental illness. Psychiatric Services 49:1218–1222,1998Link, Google Scholar
8. Ries RK, Comtois KA: Managing disability benefits as part of treatment of persons with severe mental illness and comorbid drug/alcohol disorders. American Journal on Addictions 6:330–337,1994Google Scholar
9. Ries RK, Dyck DG: Representative payee practices of community mental health centers in Washington State. Psychiatric Services 48:811–814,1997Link, Google Scholar
10. Rosenheck R, Lam J, Randolph F: Impact of representative payees on substance use among homeless persons with serious mental illness. Psychiatric Services 48:800–806,1997Link, Google Scholar
11. Herbst MD, Batki SL, Manfredi LB, et al: Treatment outcomes for methadone clients receiving lump-sum payments at initiation of disability benefits. Psychiatric Services 47:119–120,1996Link, Google Scholar
12. Spittle B: The effect of financial management on alcohol-related hospitalization. American Journal of Psychiatry 148:221–223,1991Abstract, Google Scholar
13. Stoner MR: Money management services for the homeless mentally ill. Hospital and Community Psychiatry 40:751–753,1989Abstract, Google Scholar
14. Tsemberis S, Gulcur L, Nakai M: Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health 94:651–655,2004Crossref, Medline, Google Scholar
15. Conrad KJ, Matters M, Hanrahan P, et al: Characteristics of persons with mental illness in a representative payee program. Psychiatric Services 49:1223–1225,1998Link, Google Scholar
16. Lyons JS, Coleta J, Devens M, et al: The validity of the severity of psychiatric illness in a sample of psychogeriatric patients. International Journal of Psychogeriatrics 7:407–412,1995Crossref, Medline, Google Scholar
17. Lyons JS, O'Mahoney MT, Doheny KM, et al: The prediction of short stay psychiatric inpatients. Administration and Policy in Mental Health 23:17–25,1995Crossref, Google Scholar
18. Lyons JS, O'Mahoney MT, Miller SI, et al: Predicting readmission to the psychiatric hospital in a managed care environment: implications for quality indicators. American Journal of Psychiatry 154:337–340,1997Link, Google Scholar
19. Bebout R, Drake R, Xie H, et al: Housing status among formerly homeless, dually diagnosed adults in Washington, DC. Psychiatric Services 48:936–941,1997Link, Google Scholar
20. Lehman, AF: Quality of Life Interview Core Version. Baltimore, Johns Hopkins University, 1991Google Scholar
21. Ciarlo JA, Edwards DW, Kiresuk TJ, et al: Colorado Symptom Index. Washington, DC, National Institute of Mental Health, 1981Google Scholar
22. Conrad KJ, Yagelka J, Matters MD, et al: Reliability and validity of a modified Colorado Symptom Index in a national homeless sample. Mental Health Services Research 3:141–153,2001Crossref, Medline, Google Scholar
23. Sobell LC, Sobell MB: Timeline Followback (TFLB) Users' Manual. Toronto, Canada, Addiction Research Foundation, 1992Google Scholar
24. Conrad KJ, Matters MD, Luchins D, et al: Development and cross-validation of a money mismanagement measure. Journal of Applied Measurement, in pressGoogle Scholar
25. SPSS for Windows, Release 11.5.0. Chicago, SPSS, Inc, 2002Google Scholar
26. Berk RA, Smyth GK, Sherman LW: When random assignment fails: some lessons from the Minneapolis spouse abuse experiment. Journal of Quantitative Criminology 4:209-223, 198Google Scholar



