Quality-of-Life Changes Among Patients With Obsessive-Compulsive Disorder in a Partial Hospitalization Program
Abstract
Thirty treatment-resistant patients with a primary DSM-IV diagnosis of obsessive-compulsive disorder were assessed at admission to and discharge from a partial hospitalization program to determine whether improvement in symptoms of the disorder was associated with improvements in patients' quality of life. Symptom severity was measured using the Yale-Brown Obsessive Compulsive Scale (YBOCS). Quality of life was measured using Lehman's Quality of Life (QOL) scale, which includes several objective and subjective indexes. YBOCS scores significantly improved with treatment, as did scores on the majority of the QOL subjective indexes and on the objective social, health, and activity indexes. No significant association between changes in YBOCS scores and QOL scores was found.
Contemporary clinical research should focus not only on symptomatic but also on functional improvement among patients with severe mental illness. However, functional impairment has been assessed in only a few studies of patients with obsessive-compulsive disorder (1,2). Koran and associates (2) found that patients with the disorder have poor quality of life, with scores comparable to those of depressed patients. The usefulness of these results is limited by the study's use of comparison with published norms from a historical control group, its cross-sectional nature, and its use of an instrument not specifically developed for a psychiatric population. Measurements of functional status among patients with anxiety disorders have been generally sparse, and there is no agreement on what scales are most appropriate (3,4).
We have previously described management of treatment-resistant patients in the partial hospitalization program for patients with obsessive-compulsive disorder at the University of California, Los Angeles (UCLA) (5). This program uses strict reinforcement of medication compliance and cognitive-behavioral therapy administered over several hours a day. Forty percent of previously treatment-resistant patients responded to this treatment within the six weeks of the program, as determined by a 25 percent reduction in their score on the Yale-Brown Obsessive Compulsive Scale (YBOCS) (6). The response was sustained over a period of 18 months.
In the study reported here we used Lehman's Quality of Life (QOL) scale (7) to evaluate change in functional status of a sample of patients with obsessive-compulsive disorder who were treated in the program. The goals of the study were to evaluate whether the scale was adaptable for use with the patient population with obsessive-compulsive disorder and whether patients' score on the QOL changed as measurements of the severity of obsessive-compulsive symptoms improved.
Methods
Thirty consecutive patients with obsessive-compulsive disorder admitted to the UCLA partial hospitalization program during the six-month period from January through June 1996 were treated with a combination of cognitive-behavioral therapy, medication, and psychosocial interventions over six weeks, as described in our previous report (5). All patients signed an informed consent form approved by the UCLA human subject protection committee before their enrollment in this study.
Patients' diagnoses of obsessive-compulsive disorder were confirmed by a research psychiatrist using the Structured Clinical Interview for DSM-IV (SCID) (8). The sample included 20 men and ten women, ranging in age from 18 to 56 years, with a mean age of 34 years. The majority of the subjects were Caucasian; two were Asian, and two were Latino. Only four were married. Five patients were employed, 26 received some form of disability benefits, and one both worked and received disability benefits. Twelve subjects lived with their family or relatives.
Severity of the symptoms of obsessive-compulsive disorder was assessed at entry into the program and at discharge using the YBOCS (6). The average admission YBOCS score was 30.04±3.82. The severity of affective symptoms was measured using the Hamilton Rating Scale for Depression (HRSD) and the Hamilton Rating Scale for Anxiety (HRSA) (9,10).
Patients' functional status was measured at program entry and at discharge using Lehman's QOL scale (7). The QOL has been used in the assessment of the quality of life of patients with schizophrenia (7) but not in research with patients with anxiety disorders. The short form of this scale can be administered as a clinician-rated interview within a half-hour. It measures several parameters of quality of life, including activities, family, social, work, and financial functioning. These dimensions are measured using both objective data, such as the patient's number of social meetings and the amount of support the patient receives from the family, and subjective ratings of the patient's satisfaction with experience in each dimension. The satisfaction ratings are made using a simple 8-point scale ranging from 1, terrible, to 8, delightful.
Data were analyzed using SPSS-PC statistical software. Patients' symptom severity and QOL scores were compared at program admission and discharge using repeated-measures analysis of variance (ANOVA). The Wilcoxon matched-pairs signed-ranks test was used to compare nonparametric variables before and after treatment. Pearson product-moment correlations were calculated to examine the associations between the change in QOL score and changes in symptom severity.
Results
Table 1 summarizes the statistically significant changes in the objective and subjective measures of the QOL scale between admission and discharge and the results of the repeated-measures ANOVAs. Significant changes were found for only three of the eight objective QOL measures—activities, social, and health. On the subjective measures of the QOL, changes in nearly every dimension were statistically significant. The greatest changes occurred in the activities, social, and health dimensions. The patients' YBOCS scores decreased significantly between admission and discharge.
The Wilcoxon matched-pairs signed- ranks tests showed no changes in pre- and posttreatment nonparametric comparisons of some variables of interest, such as work, disability, employment, and family support.
Correlations between change in YBOCS, HRSD, and HRSA scores and change in scores on the subscales of the QOL were performed to test the association between improvements in symptom severity and changes in the objective and subjective measures of quality of life. Changes in most of the QOL subscales were not significantly associated with changes in YBOCS scores. The strongest correlation was found between the change in YBOCS score and the change in total score on the QOL (r=.42, p=.02). Other correlations were weak, sporadic, and difficult to interpret.
Discussion and conclusions
The results suggest that the quality of life of severely ill patients with treatment-resistant obsessive-compulsive disorder improved between admission to and discharge from a specialized partial hospitalization program. Most statistically significant changes occurred in the subjective subscales that measure patients' perception of their life situations. The greatest changes occurred in subjective satisfaction with activities, health, and life as a whole. The only subjective variable that did not show a significant change was patients' appraisal of their financial situation.
Most of the objective parameters, including employment, disability, and family support, did not change significantly, although significant changes were noted for the objective indicators of health, general activity, and social activity. These three dimensions were directly related to the goals of the major components of the partial hospitalization program, including cognitive-behavioral therapy and social and rehabilitative interventions.
Changes in YBOCS scores were not associated with changes in the QOL subscales, suggesting that the outcome measures used in this study may be changing independently. These findings are similar to those of Koran and associates (2), who found minimal association between YBOCS scores and QOL scores. These findings suggest clinicians should carefully observe changes in the objective parameters of the QOL scale while treating patients' primary symptoms and should target improvements in these parameters in further therapeutic interventions.
This study had several limitations, including the short length of the treatment period, the small sample size, and the absence of a comparison group. A six-week program usually does not provide enough time to make a significant change in all areas of a patient's life. Employment may be difficult to obtain for even greatly improved patients while they are enrolled in a partial hospitalization program for treatment of obsessive-compulsive disorder, and a longer period of vocational rehabilitation may be needed. A study involving a larger sample, more sophisticated analyses, and a longer follow-up period would be needed to determine more definitively the clinical variables associated with changes in patients' quality of life.
Acknowledgments
This study was partly supported by an unrestricted grant from Solvay Pharmaceuticals to Dr. Saxena and Dr. Bystritsky. The authors thank Anthony Lehman, M.D., for use of the Quality of Life scale.
The authors are affiliated with the University of California, Los Angeles, Neuropsychiatric Institute and Hospital. Dr. Bystritsky is clinical professor and director of the anxiety disorders program. Dr. Saxana is assistant professor and director of obsessive-compulsive disorder research. Ms. Maidment is nurse coordinator. Dr. Vapnik is a nurse therapist. Dr. Tarlow is associate clinical professor and director of psychological treatment in the obsessive-compulsive disorder program. Dr. Rosen is assistant clinical professor. Address correspondence to Dr. Bystritsky, Anxiety Disorders Program, University of California, Los Angeles, Neuropsychiatric Institute and Hospital, 300 Westwood Boulevard, Los Angeles, California 90024 (e-mail, [email protected]).
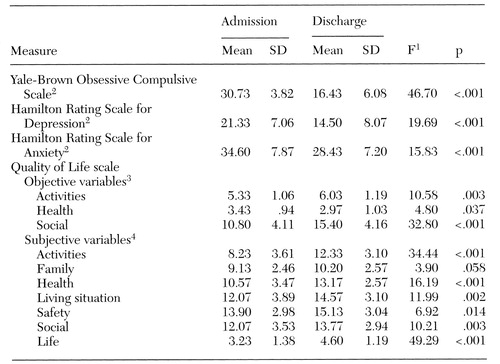 |
Table 1. Mean admission and discharge measures of symptom severity and quality of life among 30 patients with treatment-resistant obsessive-compulsive disorder treated in a partial hospitalization program
1 Analysis of variance for repeated measures, df=1,29
2 Higher scores indicate more severe symptoms.
3 Higher scores indicate a better quality of life.
4 Rated on a scale from 1, terrible, to 8, delightful. Some reported scores consist of summed scores from several questions.
1. Hollander E, Kwon JH, Stein DJ, et al: Obsessive-compulsive and spectrum disorders: overview and quality of life issues. Journal of Clinical Psychiatry 57(suppl 8):3-6, 1996Medline, Google Scholar
2. Koran LM, Thienemann ML, Davenport R: Quality of life for patients with obsessive-compulsive disorder. American Journal of Psychiatry 153:783-788, 1996Link, Google Scholar
3. Scherbourne CD, Wells KB, Judd LL: Functioning and well-being of patients with panic disorder. American Journal of Psychiatry 153:213-218, 1996Link, Google Scholar
4. Safren SA, Heimberg RG, Brown EJ, et al: Quality of life in social phobia. Depression and Anxiety 4(3):126-133, 1996-1997Google Scholar
5. Bystritsky A, Munford PR, Rosen RM, et al: A preliminary study of partial hospital management of severe obsessive-compulsive disorder. Psychiatric Services 47:170- 174, 1996Link, Google Scholar
6. Goodman WK, Price LH, Rasmussen SA, et al: The Yale-Brown Obsessive Compulsive Scale: I. development, use, and reliability. Archives of General Psychiatry 46:1006-1011, 1989Crossref, Medline, Google Scholar
7. Lehman AF: Measures of quality of life among persons with severe and persistent mental disorders. Social Psychiatry and Psychiatric Epidemiology 31:78-88, 1996Crossref, Medline, Google Scholar
8. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Education (SCID-I/P, Version 2.0). New York, New York State Psychiatric Institute, Biometrics Research Department, 1996Google Scholar
9. Hamilton M: A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry 23:56-62, 1960Crossref, Medline, Google Scholar
10. Hamilton M: The assessment of anxiety state by ratings. British Journal of Medical Psychology 32:50-55, 1959Crossref, Medline, Google Scholar



