Joint Contributions of Rare Copy Number Variants and Common SNPs to Risk for Schizophrenia
Abstract
Objective:
Both rare copy number variants (CNVs) and common single-nucleotide polymorphisms (SNPs) contribute to liability to schizophrenia, but their etiological relationship has not been fully elucidated. The authors evaluated an additive model whereby risk of schizophrenia requires less contribution from common SNPs in the presence of a rare CNV, and tested for interactions.
Method:
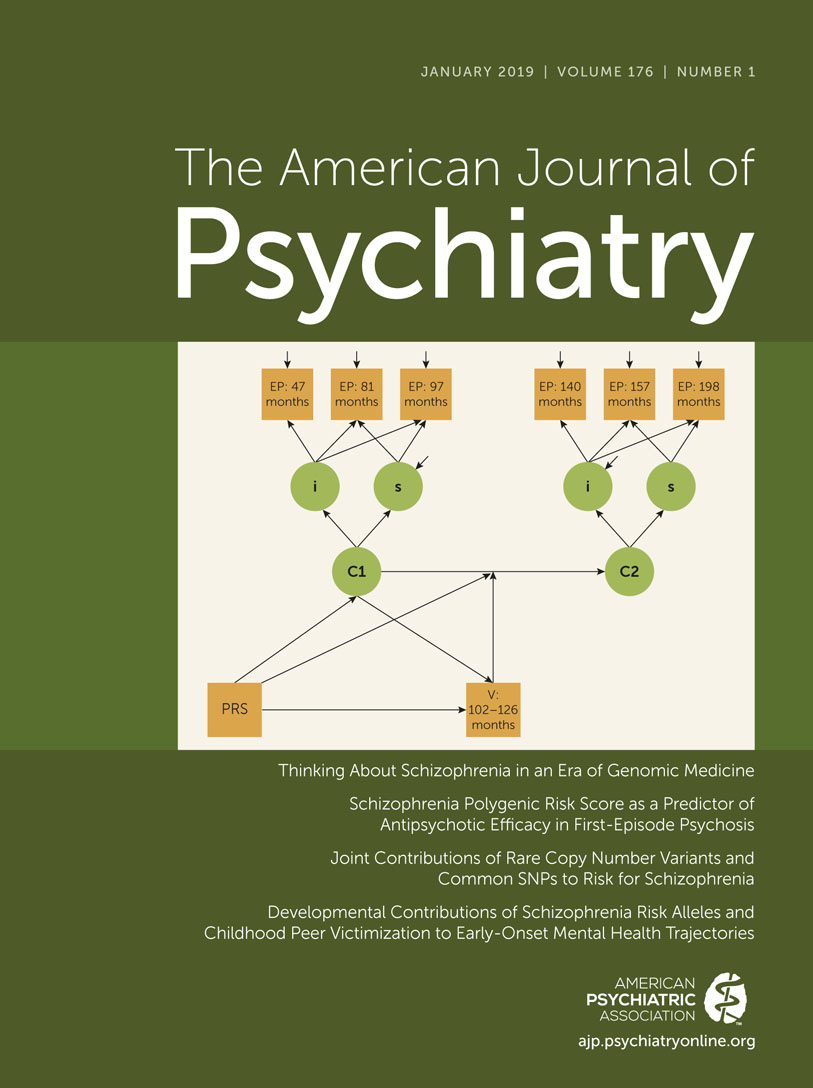
Genetic data from 21,094 case subjects with schizophrenia and 20,227 control subjects from the Psychiatric Genomics Consortium were examined. Three classes of rare CNVs were assessed: CNVs previously associated with schizophrenia, CNVs with large deletions ≥500 kb, and total CNV burden. The mean polygenic risk scores (PRSs) between study subjects with and without rare CNVs were compared, and joint effects of PRS and CNVs on schizophrenia liability were modeled by using logistic regression.
Results:
Schizophrenia case subjects carrying risk CNVs had a lower polygenic risk than case subjects without risk CNVs but a higher risk than control subjects. For case subjects carrying known risk CNVs, the PRS was diminished in proportion to the effect size of the CNV. The strongly associated 22q11.2 deletion required little added PRS to produce schizophrenia. Large deletions and increased CNV burden were also associated with lower polygenic risk in schizophrenia case subjects but not in control subjects or after removal of known risk CNV carriers.
Conclusions:
The authors found evidence for interactive effects of PRS and previously associated CNVs for risk for schizophrenia, and the results for large deletions and total CNV burden support an additive model. These findings offer insights into the genetic architecture of schizophrenia by illuminating how different established genetic risk factors act and interact to influence liability to schizophrenia.