New Insights Into the Mechanisms of Ketamine’s Antidepressant Effects: Understanding the Role of VEGF in Mediating Plasticity Processes
Major depressive disorder causes a staggering burden worldwide (1). Because many first-line treatments are not efficacious, the psychiatric community continues to push for alternate pharmacological interventions, particularly for those suffering from treatment-resistant depression (2). Ketamine has gained attention as an alternative to typical antidepressants, as the induction of its antidepressant effects occurs within hours, as opposed to over the course of several weeks (3). While our understanding of the precise mechanisms that mediate the effects of ketamine has remained elusive, several preclinical studies suggest that ketamine affects synaptic plasticity in the medial prefrontal cortex (mPFC) and hippocampus via several cell signaling pathways (4). Although research in clinical populations is essential for moving forward with ketamine and other fast-acting antidepressants, animal models can help bridge the gap between behavioral manifestations and the neural mechanisms that underlie responses to these drugs. Such research has been facilitated by developments over the last decade that have allowed researchers to manipulate neural circuits and the genes that regulate these circuits.
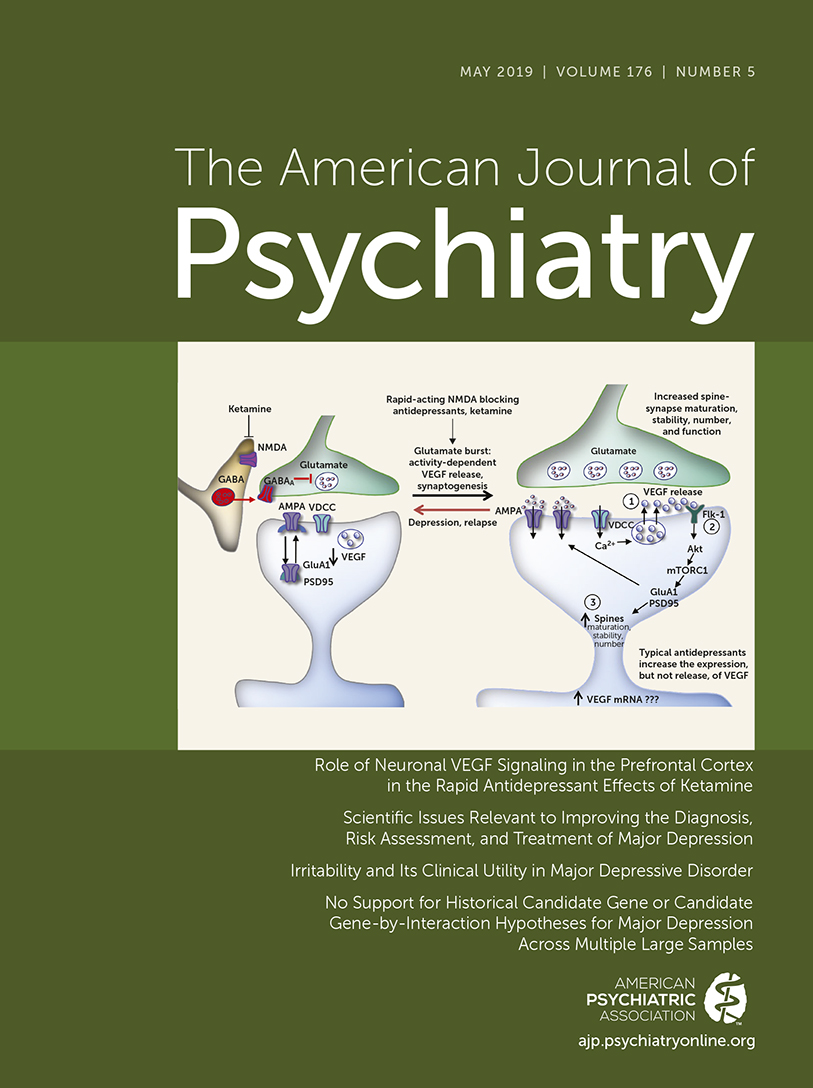
It is important to note that ketamine, while effective in rapidly reducing depressive symptoms, is a drug that is subject to abuse and has significant side effects, raising concerns about its widespread clinical utility. Gaining insight into the mechanisms underlying ketamine’s antidepressant effects paves the way for developing new rapid-acting antidepressants without the dissociative effects and abuse potential of ketamine. In this regard, understanding the contribution of the many signaling systems that have been implicated in the mechanism of action of ketamine, including the N-methyl-d-aspartate (NMDA) receptor (5), the AMPA receptor (6), the glutamatergic system (4), and the opiate system (7), is essential. Consistent with the conception of major depressive disorder as a disorder of neuroplasticity (8), the function of neurotrophic factors, such as brain-derived neurotrophic factor (BDNF), has also been linked to ketamine response (9) and independently to major depression (4). A new article in this issue of the Journal by Deyama et al. (10) provides convincing evidence using myriad research methods in rodents to support the involvement of another neurotrophic factor, vascular endothelial growth factor (VEGF), which signals via its receptor, fetal liver kinase 1 (Flk-1), to mediate the effects seen following ketamine administration in a preclinical model of behavioral responses associated with depressive symptoms.
Deyama et al. use a series of complementary molecular and behavioral methods to demonstrate that VEGF–Flk-1 signaling is involved in the mechanisms underlying the rapid antidepressant effects of ketamine. The authors genetically engineered mice to produce a neuron-specific deletion of VEGF or Flk-1 in the pyramidal cells of the mPFC and hippocampus. This conditional knockout of VEGF or Flk-1 blocked the acute effects of ketamine as assessed using behavioral paradigms thought to reflect constructs associated with depression. By blocking the availability of VEGF in the mPFC with a specific antibody, the authors also showed that the behavioral and neural effects of ketamine are related to the synaptic release of VEGF. In addition, VEGF infused into the mPFC resulted in ketamine-like behavioral effects. The authors confirmed involvement of VEGF–Flk-1 signaling using a different method to knock down the expression of Flk-1 in mPFC neurons. Similar to the conditional knockout, this short hairpin RNA-mediated knockdown blocked the behavioral effects of ketamine administration. Importantly, in the absence of stressful challenges, these molecular manipulations did not affect baseline behaviors. Together, these results indicate that VEGF–Flk-1 signaling in the mPFC is both necessary and sufficient for the acute behavioral actions of ketamine.
To understand how VEGF–Flk-1 signaling mediates antidepressant-like effects, the authors explored processes related to neuroplasticity. Using neuronal cultures, the authors found that application of ketamine or VEGF increased dendritic branching, an effect that was blocked by an Flk-1 inhibitor. In control mice, an injection of ketamine significantly increased synaptic density in mPFC pyramidal neurons, an effect that did not occur in the VEGF knockout mice. Together, these findings indicate that the antidepressant effects of ketamine, thought to involve the induction of neuroplasticity, are in part mediated by VEGF–Flk-1 signaling in the mPFC.
As ketamine treatment becomes more ubiquitous in the clinic, with the first treatment approved by the Food and Drug Administration for nasally administered esketamine recently becoming available (11, 12), research such as the work presented by Deyama et al. is essential for clarifying the mechanisms by which ketamine affects the brain. These results clearly support an essential role for VEGF signaling in the mPFC in mediating the antidepressant effects of ketamine; however, whether these results will translate to humans remains to be seen. Several studies have assessed levels of VEGF in clinical populations and, although increased blood VEGF levels have been reported in patients with major depression, the opposite or no relationship has also been reported (13, 14). This discrepancy is likely due to the use of distal measurements (i.e., serum, plasma), which may not reflect changes in VEGF signaling occurring in circumscribed regions of the brain. Interestingly, a study with a small sample has reported that ECT, a prominent intervention for treatment-resistant depression, produces increases in VEGF in the serum of patients with treatment-resistant depression (15). Further clinical studies with larger samples and more sensitive measurements related to brain function will be essential for confirming the importance of VEGF signaling in ketamine administration in humans and for understanding its relation to other proposed signaling systems.
Although the present study suggests that VEGF is important, this does not preclude the involvement of other neuronal systems in mediating the effects of ketamine, such as signaling via BDNF and other neurotrophic factors. BDNF has been independently linked to the plasticity associated with ketamine administration in the mPFC (16) and hippocampus (17), as well as to antidepressant responses in humans (9). Both BDNF and VEGF signaling converge on the mechanistic target of rapamycin complex 1 (mTORC1) pathway (4, 18), which has also been implicated in ketamine’s mechanism of action (19, 20). Understanding at a subcellular level how these ligands and their receptor systems interact, particularly with other proposed mechanisms of action, such as glutamine, NMDA receptor, and AMPA receptor signaling, will contribute to the identification of additional novel treatment strategies. Studies designed to parse these interactions necessitate the use of animal models, and the conditional knockout models characterized in the present study will be valuable in understanding the complex interplay between the many neurotrophic factors, neurotransmitters, and other cellular processes involved.
It is also important to appreciate the complexities of the neural circuitry that underlies adaptive and maladaptive mood regulation. In addition to the mPFC, which is a focus of the present study, other prefrontal regions and subcortical structures, such as the hippocampus and amygdala, are implicated in major depressive disorder (21). Thus, an interesting unanswered question is the extent to which VEGF signaling influences the interplay between the mPFC and various other regions involved in mood regulation (22). Another group has confirmed that VEGF signaling in the hippocampus is at least partly responsible for the antidepressant effects of ketamine (23). Moreover, the activation of pathways between the ventral hippocampus and the mPFC recapitulates the effects of a single dose of ketamine (24) in a process that appears to be dependent on BDNF signaling. In addition to understanding the molecules involved, defining the specific circuitry in which they exert their effects will be an important step for future targeted manipulations in preclinical models that will guide molecularly based, circuit-specific treatment development.
Progress in understanding major depressive disorder, particularly in its treatment-resistant forms, is challenging. This is partially due to the complexities in our current construct of major depression, which is highly heterogeneous and likely involves different pathophysiologies. Additionally, because of methodological constraints, research in patient populations is limited in its ability to precisely identify molecular and cellular mechanisms. Although studies in animal models cannot fully capture the complex phenotypes associated with depression (25), they provide useful insights into the molecular underpinnings of the neural circuit alterations implicated in psychiatric disorders and their treatment. Deyama et al. add to our knowledge of the mechanisms by which ketamine induces its antidepressant effects, pointing to the VEGF system as a mediator of neural plasticity in the mPFC. Ketamine is a novel and promising treatment for those suffering from depression, and further understanding its mechanism of action paves the way for a new generation of fast-acting antidepressants with reduced potential for off-target effects.
1 : The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry 2015; 76:155–162Crossref, Medline, Google Scholar
2 : Diagnosis and definition of treatment-resistant depression. Biol Psychiatry 2003; 53:649–659Crossref, Medline, Google Scholar
3 : A randomized trial of an N-methyl-d-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 2006; 63:856–864Crossref, Medline, Google Scholar
4 : Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med 2016; 22:238–249Crossref, Medline, Google Scholar
5 : Ketamine and other N-methyl-d-aspartate receptor antagonists in the treatment of depression: a perspective review. Ther Adv Chronic Dis 2015; 6:97–114Crossref, Medline, Google Scholar
6 : Antidepressant effects of ketamine and the roles of AMPA glutamate receptors and other mechanisms beyond NMDA receptor antagonism. J Psychiatry Neurosci 2017; 42:222–229Crossref, Medline, Google Scholar
7 : Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry 2018; 175:1205–1215Link, Google Scholar
8 : A neurotrophic model for stress-related mood disorders. Biol Psychiatry 2006; 59:1116–1127Crossref, Medline, Google Scholar
9 : BDNF: a key transducer of antidepressant effects. Neuropharmacology 2016; 102:72–79Crossref, Medline, Google Scholar
10 : Role of neuronal VEGF signaling in the prefrontal cortex in the rapid antidepressant effects of ketamine. Am J Psychiatry 2019; 176:388–400Link, Google Scholar
11 : Efficacy and safety of intranasal esketamine adjunctive to oral antidepressant therapy in treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry 2018; 75:139–148Crossref, Medline, Google Scholar
12 FDA News Release: FDA approves new nasal spray medication for treatment-resistant depression; available only at a certified doctor’s office or clinic. US Food and Drug Administration, Silver Spring, Md, 2019 (https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm632761.htm)Google Scholar
13 : VEGF and depression: a comprehensive assessment of clinical data. J Psychiatr Res 2013; 47:1080–1087Crossref, Medline, Google Scholar
14 : Role of trophic factors GDNF, IGF-1 and VEGF in major depressive disorder: a comprehensive review of human studies. J Affect Disord 2016; 197:9–20Crossref, Medline, Google Scholar
15 : Vascular endothelial growth factor (VEGF) serum concentration during electroconvulsive therapy (ECT) in treatment resistant depressed patients. Prog Neuropsychopharmacol Biol Psychiatry 2011; 35:1322–1325Crossref, Medline, Google Scholar
16 : BDNF release is required for the behavioral actions of ketamine. Int J Neuropsychopharmacol 2014; 18:pyu033Google Scholar
17 : Acute administration of ketamine in rats increases hippocampal BDNF and mTOR levels during forced swimming test. Ups J Med Sci 2013; 118:3–8Crossref, Medline, Google Scholar
18 : Ketamine: promising path or false prophecy in the development of novel therapeutics for mood disorders? Neuropsychopharmacology 2015; 40:259–267Crossref, Medline, Google Scholar
19 : mTOR-dependent synapse formation underlies the rapid antidepressant effects of NMDA antagonists. Science 2010; 329:959–964Crossref, Medline, Google Scholar
20 : Psychiatric disorders: ketamine modifies mood through mTOR. Nat Rev Neurosci 2010; 11:666–667Crossref, Medline, Google Scholar
21 : Neurobiology of depression. Neuron 2002; 34:13–25Crossref, Medline, Google Scholar
22 : Interactions among the medial prefrontal cortex, hippocampus and midline thalamus in emotional and cognitive processing in the rat. Neuroscience 2006; 142:1–20Crossref, Medline, Google Scholar
23 : Hippocampal VEGF is necessary for antidepressant-like behaviors but not sufficient for antidepressant-like effects of ketamine in rats. Biochim Biophys Acta 2016; 1862:1247–1254Crossref, Medline, Google Scholar
24 : Activation of a ventral hippocampus–medial prefrontal cortex pathway is both necessary and sufficient for an antidepressant response to ketamine. Mol Psychiatry 2016; 21:1298–1308Crossref, Medline, Google Scholar
25 : Animal models of neuropsychiatric disorders. Nat Neurosci 2010; 13:1161–1169Crossref, Medline, Google Scholar