In This Issue
Anticipation in Generalized Anxiety
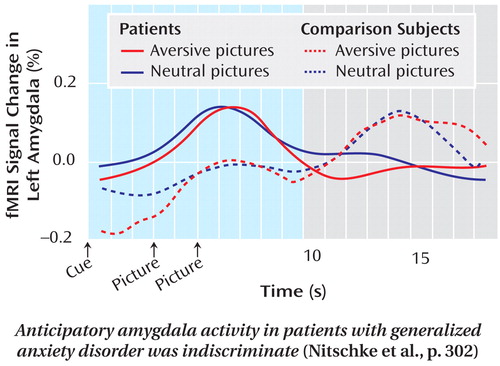
Anticipatory anxiety is a cardinal clinical symptom of generalized anxiety disorder. Nitschke et al. (CME, p. Original article: 302 ) developed a laboratory demonstration of this symptom to examine its physiological basis and to predict treatment response. Patients and a healthy comparison group were told that aversive pictures would be preceded by a minus sign and neutral images would be cued by a circle. Brain activity during viewing of these cues was measured with functional MRI . Responses in the bilateral dorsal amygdala to both types of cues were greater in the generalized anxiety group than the comparison group. Also, higher anticipatory activity in the patients’ anterior cingulate cortex at baseline was related to greater response after 8 weeks of venlafaxine treatment. In an editorial on p. Original article: 263 , Dr. Cameron Carter examines these findings.
Psychotherapy for Eating Disorders
Two enhanced forms of cognitive-behavioral therapy (CBT) led to substantial and equivalent improvement over 20 weeks in patients with a variety of eating disorders. Fairburn et al. (CME, p. Original article: 311 ) report that the subgroup with marked additional psychopathology responded better to the therapy version that explored traits and interpersonal problems, whereas those with less complex cases responded better to CBT focused solely on disordered eating. The study group comprised patients with mixed symptoms of anorexia nervosa and bulimia nervosa and excluded those with very low body mass indices. At the 15-month follow-up, the overall score for eating disorders was within one standard deviation of normal for 51% of the patients. Drs. Scott Crow and Carol Peterson discuss these results in an editorial on p. Original article: 266 .
Antidepressants and Gestational Hypertension
Women who continued to take selective serotonin reuptake inhibitor (SSRI) antidepressants during pregnancy were more than twice as likely as nonusers to develop gestational hypertension. Their risk of preeclampsia was more than four times normal. These estimates by Toh et al. (p. Original article: 320 ) were based on reports from 5,731 women who were interviewed within 6 months of delivery. Those who took SSRIs before pregnancy but stopped by the end of the first trimester did not have a significantly elevated risk of preeclampsia. The authors point out that the study does not differentiate between the effects of the medication and the depression itself. An editorial by Dr. Kimberley Yonkers on p. Original article: 268 explores the possible clinical implications of these data.
Obsessions and Compulsions in a Community Cross-Section
A community developmental study indicates that subsyndromal obsessive thoughts and compulsive behaviors are common in the general population. Fullana et al. (p. Original article: 329 ) analyzed responses from structured interviews at ages 11, 26, and 32 years with nearly all of the 1,037 original participants in the Dunedin, New Zealand, study. Those who reported obsessions or compulsions at age 11 were more likely to report similar symptoms or to receive a diagnosis of obsessive-compulsive disorder (OCD) in adulthood. Only 2% met the criteria for an OCD diagnosis as adults, but subclinical obsessions and compulsions were reported by 13% and 17%, respectively, of the people without mental disorders. Such symptoms were also present in more than one-third of those with other anxiety disorders or depression. Obsessions about inflicting harm and compulsive checking to prevent harm were the most common. The only obsessive and compulsive symptoms associated with treatment seeking were fears of harming others and thoughts deemed to be shameful. Dr. Murray Stein highlights key findings of the study in an editorial on p. Original article: 271 .



