Elevated Suicide Rate Among HIV-Positive Persons Despite Benefits of Antiretroviral Therapy: Implications for a Stress and Coping Model of Suicide
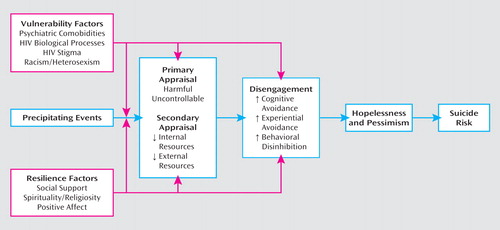
Prior to antiretroviral therapy (ART), viable long-term treatment options for HIV infection were unavailable and advanced HIV disease was a terminal illness. Because HIV-positive persons were acutely aware of the progressive nature of their illness, perceived risk for developing AIDS and AIDS-related life events (e.g., diagnosis of an AIDS-related complex) were important determinants of suicide intent (1). The burdens of coping with the insidious onset of functional limitations related to advanced HIV disease and the ever-present threat of death may partially explain the markedly elevated suicide rate among HIV-positive persons during this period. Given that the introduction of ART has led to substantial improvements in HIV-related health outcomes, Keiser and colleagues (2) examined whether the suicide rate declined over time in the Swiss HIV Cohort Study compared to the general Swiss population. Their findings indicate that the suicide rate among HIV-positive persons declined in the ART era, and this appeared to be due partially to improvements in health status. However, the suicide rate remains more than three times higher among HIV-positive persons than in the general population. This finding highlights the need for an integrative conceptual model to inform clinical intervention and research that addresses suicide risk in HIV-positive persons. I propose a stress and coping model of suicide risk (Figure 1) in which vulnerability and resilience factors modulate psychological responses to precipitating events that increase suicide risk.
Psychiatric comorbidities are one vulnerability factor for elevated suicide risk. A greater prevalence of comorbid psychiatric conditions among HIV-positive persons may partially explain the higher suicide rate, particularly in the ART era, when improved health status mitigates the effects of disease-related factors on suicide risk. Lending support to this assertion, a review of medical records from individuals in the Swiss HIV Cohort Study who died by suicide indicates that a diagnosis of mental illness and a history of psychiatric treatment were more common in the ART era (2). Although this change may reflect enhanced integration of psychiatric assessment and referral in HIV specialty clinics, other investigations support the importance of psychiatric factors (e.g., depression and hopelessness) as correlates of suicide risk in the ART era (3, 4). Because comorbid psychiatric conditions are important drivers of suicide risk, efforts are needed to promote enhanced psychiatric screening and referral in HIV specialty clinics. Physicians should routinely screen HIV-positive persons for comorbid psychiatric disorders and explicitly assess suicidal ideation, plan, and intent. In HIV specialty clinics that use electronic medical records, brief structured assessments with clinical reminders could be implemented to ensure that patients are routinely screened. In addition to routine screening, data from the Swiss HIV Cohort Study also highlight the need for innovative interventions that promote access to and utilization of mental health treatment. Among HIV-positive individuals who died by suicide in the ART era, more than one-fifth of those with a mental health diagnosis were not receiving any psychiatric treatment (2). Providing mental health and substance abuse treatment on-site in HIV specialty clinics can remove barriers to accessing care and assist with engaging patients who are ambivalent about seeking psychiatric treatment. Addressing structural barriers to psychiatric screening and referral could promote an integrated approach to HIV specialty care that has the potential to more effectively meet the needs of HIV-positive persons.
Although psychiatric comorbidities represent a key determinant of suicide risk among HIV-positive persons, it is important to consider biological and social vulnerability factors that can heighten suicide risk. Underlying biological processes related to HIV infection have important neuropsychiatric sequelae. For example, HIV infection is characterized by chronic immune activation, which promotes the degradation of l-tryptophan (an essential amino acid precursor to serotonin). Indices of tryptophan degradation have been associated with impaired quality of life and greater depressive symptom severity among HIV-positive persons (5, 6). Although l-tryptophan depletion is partially reversed after initiation of ART (5), regular use of stimulants such as methamphetamine is independently associated with lower tryptophan levels after controlling for ART nonadherence among HIV-positive persons (6). The effects of these biobehavioral pathways on suicide risk could be augmented by the stigma and discrimination that HIV-positive persons experience, which are associated with increased depressive symptoms (7). The stress of living with a stigmatized illness is further compounded by experiences of racism and heterosexism that are common among groups that are disproportionately affected by HIV/AIDS. This is supported in part by research demonstrating that the experience of antigay discrimination or violence is associated with suicidal ideation (8). Taken together, these psychiatric, biological, and social vulnerability factors could accentuate the negative impact of stressful life events and promote cognitive and behavioral patterns of responding that increase suicide risk.
Stress and coping theory (9) provides a framework for understanding how psychological responses to stressful life events may increase suicide risk. HIV-positive persons commonly experience a variety of chronic, uncontrollable stressors that can cumulatively contribute to the perception that living with this stigmatized illness is intolerable. Precipitating events are conceptualized as specific stressful life events that are linked to increased suicide risk. These can be general (e.g., bereavement) or HIV-specific (e.g., the experience of ART-related side effects and HIV disease progression) stressors that often revolve around the themes of harm or loss. Individuals actively evaluate or appraise their environments to determine the nature of stressful events (primary appraisals) as well as the internal and external resources available for managing stressors (secondary appraisals). Primary appraisals of precipitating events as harmful and uncontrollable coupled with secondary appraisals of resources as lacking can promote cognitive-behavioral disengagement. Cognitive-behavioral disengagement is characterized by reliance on cognitive and experiential avoidance as a means of coping. Avoidance of thoughts and feelings related to stressful events is often accomplished by a narrowing of one’s attention focus to sensations in the present moment. These cognitive changes promote behavioral disinhibition, which places one at elevated risk for suicidal or parasuicidal behaviors and may also increase engagement in other risk-taking behaviors, such as substance use. Over time, this pattern of cognitive-behavioral disengagement may lead directly to feelings of hopelessness and a pervasive sense of pessimism, which in turn increase suicide risk. The relevance of cognitive-behavioral disengagement is supported by an investigation that found that greater escape-avoidance coping is associated with suicidal ideation (10). However, these cognitive-behavioral vulnerabilities do not universally lead to increased suicide risk. Sources of psychological resilience (e.g., social support) can buffer the deleterious effects of precipitating events and promote the search for meaning (e.g., spirituality/religiosity) that is crucial to reappraising events and building resources for managing life events that were initially viewed as intolerable. Resilience factors that bolster coping self-efficacy (secondary appraisals), enhance positive reappraisal coping efforts, and decrease cognitive-behavioral disengagement may reduce suicide risk (3, 10).
Further research is clearly needed to examine the dynamic interplay among biological, social, and psychological factors in relation to suicide risk in HIV-positive persons. However, these factors should be considered in case conceptualization and the selection of interventions to address suicide risk among HIV-positive persons. Randomized controlled trials support the efficacy of group-based cognitive-behavioral interventions designed to promote more effective coping responses and improve psychological adjustment with HIV-positive persons (11). These may be effective adjuvant treatments to address suicide risk among HIV-positive individuals.
1 : Factors influencing suicide intent in gay and bisexual suicide ideators: differing models for men with and without human immunodeficiency virus. J Pers Soc Psychol 1991; 61:776–788 Crossref, Medline, Google Scholar
2 : Suicide in HIV-infected individuals and the general population in Switzerland, 1988–2008. Am J Psychiatry 2010; 167:143–150 Link, Google Scholar
3 : Correlates of suicidal ideation among HIV-positive persons. AIDS 2007; 21:1199–1203 Crossref, Medline, Google Scholar
4 : Desire for hastened death among patients with advanced AIDS. Psychosomatics 2006; 47:504–512 Crossref, Medline, Google Scholar
5 : Effective antiretroviral therapy reduces degradation of tryptophan in patients with HIV-1 infection. Clin Immunol 2002; 104:242–247 Crossref, Medline, Google Scholar
6 : Stimulant use is associated with immune activation and depleted tryptophan among HIV-positive persons on anti-retroviral therapy. Brain Behav Immun 2008; 22:1257–1262 Crossref, Medline, Google Scholar
7 : HIV-related stigma: adapting a theoretical framework for use in India. Soc Sci Med 2008; 67:1225–1235 Crossref, Medline, Google Scholar
8 : Experiences of harassment, discrimination, and physical violence among young gay and bisexual men. Am J Public Health 2004; 94:1200–1203 Crossref, Medline, Google Scholar
9 : Positive psychological states and coping with severe stress. Soc Sci Med 1997; 45:1207–1221 Crossref, Medline, Google Scholar
10 : Depression and thoughts of suicide among middle-aged and older persons living with HIV-AIDS. Psychiatr Serv 2001; 51:903–907 Link, Google Scholar
11 : Stress management interventions for HIV+ adults: a meta-analysis of randomized controlled trials, 1989 to 2006. Health Psychol 2008; 27:129–139 Crossref, Medline, Google Scholar



