Prevalence and Heritability of Compulsive Hoarding: A Twin Study
Abstract
Objective: Compulsive hoarding is a serious health problem for the sufferers, their families, and the community at large. It appears to be highly prevalent and to run in families. However, this familiality could be due to genetic or environmental factors. This study examined the prevalence and heritability of compulsive hoarding in a large sample of twins. Method: A total of 5,022 twins completed a validated measure of compulsive hoarding. The prevalence of severe hoarding was determined using empirically derived cutoffs. Genetic and environmental influences on compulsive hoarding were estimated using liability threshold models, and maximum-likelihood univariate model-fitting analyses were employed to decompose the variance in the liability to compulsive hoarding into additive genetic and shared and nonshared environmental factors (female twins only; N=4,355). Results: A total of 2.3% of twins met criteria for caseness, with significantly higher rates observed for male (4.1%) than for female (2.1%) twins. Model-fitting analyses in female twins showed that genetic factors accounted for approximately 50% of the variance in compulsive hoarding, with nonshared environmental factors and measurement error accounting for the other half. Conclusions: Compulsive hoarding is highly prevalent and heritable, at least in women, with nonshared environmental factors also likely to play an important role.
Compulsive hoarding is defined as the acquisition of a large number of possessions with failure to discard them; clutter that precludes activities for which living spaces were designed; and significant distress or impairment in functioning caused by the hoarding (1) . It represents a serious health problem for the sufferers, their families, and the community at large. Compulsive hoarding is associated with substantial psychiatric and medical comorbidity, including obsessive-compulsive disorder, mood disorders, social phobia, personality disorders, obesity, a wide range of chronic and severe medical concerns (2 – 7) , social isolation (4 , 8) , family burden (9) , work impairment, high mental health service utilization, and even risk of eviction (7) . Therapeutic response to antidepressants and behavior therapy is poor or partial at best (10 – 14) .
Two recent epidemiological reports suggest that hoarding may be highly prevalent in the community. Samuels et al. (15) analyzed data from the Hopkins Epidemiology of Personality Disorder Study (N=742) and estimated the prevalence of compulsive hoarding at nearly 4% of the population. A much higher lifetime prevalence, more than 14%, was reported in the National Comorbidity Survey Replication (16) . However, it is unclear from these studies how many individuals exhibit sufficiently distressing and interfering problems to qualify for a diagnosis of compulsive hoarding as defined by Frost and Hartl (1) . If more stringent criteria were applied, the prevalence of “excessive” hoarding might be substantially lower.
Compulsive hoarding is a clearly familial condition, with a large proportion of sufferers reporting at least one first-degree relative with hoarding problems (4 , 6 , 17 , 18) . For example, Pertusa et al. (4) recently found that over 50% of a sample of severe compulsive hoarders (regardless of whether or not they had obsessive-compulsive disorder) had a first-degree relative with hoarding problems. Recent studies of sibling pairs concordant for obsessive-compulsive disorder have also confirmed that hoarding is robustly familial (19 – 22) . However, this familiality could be due to genetic or environmental factors. Twin studies are particularly well suited to disentangling the contribution of these factors.
Our aims in this study were therefore twofold: 1) to estimate the prevalence of severe compulsive hoarding in a sample of 5,022 monozygotic and dizygotic twins, and 2) to estimate the contribution of genetic and shared and nonshared environmental factors to compulsive hoarding in a subsample of 4,355 female twins.
Method
Participants
Participants were monozygotic and dizygotic twins from the TwinsUK adult twin registry (www.twinsuk.ac.uk). The sample characteristics have been described in detail elsewhere (23) . Briefly, the registry was started in 1993 and consists of nearly 10,000 Caucasian monozygotic and dizygotic twins, age 16 or older from all over the United Kingdom. All twins were initially recruited through a series of media advertisements that were not disorder specific. The twin sample has been shown to be comparable to age-matched population singletons in terms of disease-related and lifestyle characteristics (24) . The Peas in the Pod questionnaire (25) was used to ascertain zygosity, which was further confirmed in cases of uncertainty by DNA fingerprinting or from genome-wide scans.
The Hoarding Rating Scale–Self-Report (HRS-SR; 7, 9) was sent to all active twins in the registry (N=8,313) as part of a larger wave of data collection. A total of 5,022 twins returned the questionnaire ( Figure 1 ). Responders and nonresponders were comparable in terms of zygosity (53% and 50% monozygotic, respectively) and socioeconomic status (Index of Multiple Deprivation [26] mean score, 3.7 [SD=1.2] compared with 3.3 [SD=1.3], respectively). However, nonresponders were more likely to be male (56% compared with 36%; χ 2 =189.9, df=1, p<0.01) and younger (mean age, 46 years [SD=14, range=16–90] compared with 55 years [SD=13; range=17–86]; t=28.8, df=8312, p<0.01).
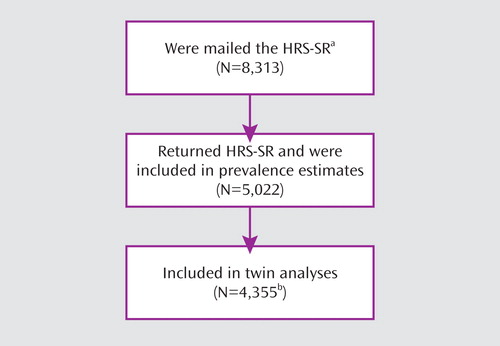
a HRS-SR=Hoarding Rating Scale–Self-Report.
b The following were excluded from the analysis: male twins (N=509), opposite-sex dizygotic twins (N=104), and singleton twins for whom the co-twin sex was unknown (N=54).
The sample available for analysis included 2,053 twin pairs (125 monozygotic males, 65 dizygotic males, 971 monozygotic females, 857 dizygotic females, and 35 dizygotic twins of the opposite sex) and 916 singleton twins (73 monozygotic males, 56 dizygotic males, 383 monozygotic females, 316 dizygotic females, 34 dizygotic opposite-sex twins, and 54 dizygotic twins whose co-twin sex was unknown). Over 80% of the sample was female (N=4,459; 89.3%), and the mean age was 55.5 years (SD=13.4; range=17–86).
The St. Thomas’ Hospital (London) research ethics committee approved the study, and all twins provided informed consent.
Instruments
The HRS-SR is a brief self-administered instrument consisting of five items (clutter, difficulty discarding, excessive acquisition, distress, and impairment), each measured on a Likert scale ranging from 0 (none) to 8 (extreme), with 4 reflecting “moderate” symptoms; total score can range from 0 to 40. The HRS-SR correlates strongly with the interview version of the instrument (27) , and both versions have excellent psychometric properties (internal consistency, test-retest reliability, and interrater reliability), discriminate between hoarding and nonhoarding groups, and correlate highly with other measures of hoarding (7 , 9 , 27) . A receiver operating characteristic analysis determined that scores over 17 on the total score of the interview version of the instrument discriminate hoarding from nonhoarding cases with a sensitivity and specificity of 0.95 (27) . We therefore used this cutoff score to determine caseness in this sample.
In this study, the HRS-SR had good internal consistency (Cronbach’s alpha=0.86), and a principal-components analysis revealed a single factor structure explaining 64% of the variance. Factor loadings ranged from 0.74 (excessive acquisition) to 0.84 (distress).
Prevalence Estimates
Analyses of prevalence rates were performed using Stata, version 10 (Stata Corp, College Station, Tex.), which allows control for the effects of clustering of individuals within families.
Twin Analyses
Because the HRS-SR distribution was positively skewed (skewness=2.56), polychoric correlations and genetic and environmental influences on compulsive hoarding were estimated using liability threshold models, fit to raw data in the statistical program Mx (http://www.vcu.edu/mx/). This method assumes that a disorder, in this case compulsive hoarding, has an underlying continuous distribution of liability, with each threshold representing a discrete category (28) . Individuals whose liability is above a certain threshold will experience hoarding symptoms; individuals whose liability is above a higher threshold will have more pronounced symptoms or meet criteria for caseness. In our analyses, we used three thresholds, representing different categories of symptom severity: no symptoms (i.e., an HRS-SR score of 0); minimal symptoms (HRS-SR scores ranging from 1 to 5); moderate symptoms (HRS-SR scores ranging from 6 to 16); and severe symptoms or caseness (HRS-SR scores ranging from 17 to 40). We chose to use three thresholds (as opposed to more than three) because these provided a good representation of variability in symptom severity within our sample while ensuring sufficient, and roughly equal, numbers of cases within each category.
The differing levels of genetic resemblance between monozygotic and dizygotic twins were employed to disentangle genetic and environmental influences. Polychoric correlations provide an estimate of the magnitude of similarity within pairs of twins. Because monozygotic twins share all of their genetic makeup and dizygotic twins share on average about 50% of their genes, monozygotic twins are expected to be more similar than dizygotic twins if genetic influence is important. Shared environmental influence is seen as the extent to which genetic factors do not account for twin resemblance. Nonshared environmental influence (and error of measurement) is implicated to the degree that genetic and shared environmental sources of variance cannot account for all of the observed variation. The most direct estimate of nonshared environmental factors is the degree to which monozygotic correlations depart from unity.
Maximum-likelihood univariate model-fitting analyses were employed to decompose the variance in the liability to compulsive hoarding into additive genetic (A) and shared (C) and nonshared (E) environmental factors. As is standard procedure with analysis of raw data, the data were first fitted to a saturated model (i.e., a model in which polychoric correlations and thresholds are estimated freely), and goodness of fit, in terms of a log-likelihood chi-square statistic and Akaike’s information criterion, was obtained by comparing the –2 log-likelihood statistic of the more parsimonious genetic model (ACE model) to that of the saturated model. To establish the best fit for the data, alternative models were tested by systematically dropping paths from the full model (i.e., AE, CE, E). The nested and full models were compared using the likelihood ratio test (29) , and the relative improvement or worsening of the fit was assessed on the basis of a change in chi-square relative to the change in degrees of freedom.
The small number of male twins (N=509) and dizygotic opposite-sex twins (N=104) did not afford sufficient power to test quantitative and qualitative sex differences in the liability to compulsive hoarding. For this reason, twin analyses were performed using data from same-sex female twins only. Singleton twins for whom the co-twin sex was unknown (N=54) were also excluded, resulting in a final sample of 4,355 for twin analyses ( Figure 1 ).
Results
Prevalence of Compulsive Hoarding
Table 1 summarizes prevalence rates of compulsive hoarding as estimated from the number of twins who met criteria for caseness on the HRS-SR (score ≥17). Overall, 2.3% (N=117; mean HRS-SR score=21.18 [SD=4.98]) of the whole sample reported symptoms severe enough to indicate caseness. A significantly higher rate of severe hoarding was observed for male than for female twins (χ 2 =7.14, df=1, p<0.01). Similarly, a significantly higher rate of any hoarding symptoms (versus no symptoms) was observed for male than for female twins (χ 2 =8.35, df=3, p<0.01).
Heritability of Compulsive Hoarding
Polychoric correlations for monozygotic (N=1,354 pairs) and dizygotic (N=1,173 pairs) female twins were 0.52 (95% confidence interval [CI]=0.45–0.57) and 0.27 (95% CI=0.19–0.35), respectively. The pattern of correlations indicates greater similarity for monozygotic than dizygotic twins, suggesting a meaningful genetic basis for compulsive hoarding and negligible shared environmental effects. The moderate monozygotic correlation is indicative of nonshared environmental influence.
Model-fitting results and standardized parameter estimates are summarized in Table 2 . In the saturated model, liability thresholds could be equated across zygosity and birth order without any loss in fit, indicating that the prevalence of compulsive hoarding is similar for monozygotic and dizygotic twins and for first- and second-born twins. Comparisons of the ACE model with the fully saturated model indicate that the more parsimonious genetic model fits the data well. Dropping the shared environmental parameter (C) did not result in a significant loss in fit. In contrast, dropping the genetic parameter (A) resulted in a significantly worse fit to the data, indicating that additive genetic factors are important in explaining variability in this trait. Dropping both the additive genetic and shared environmental parameters resulted in an increasingly worse fit.
Table 2 shows standardized parameter estimates based on the full ACE model. Consistent with the pattern of correlations, genetic factors accounted for approximately 50% of the variance in compulsive hoarding, with nonshared environmental factors and measurement error accounting for the other half.
Discussion
In this study, we examined the prevalence and heritability of compulsive hoarding traits in a large sample of twins using a reliable and valid instrument that assesses the key domains of compulsive hoarding: difficulties discarding, clutter, excessive acquisition, distress, and impairment. Because this instrument has empirically derived cutoffs, we were able to estimate the prevalence of significant hoarding problems, or caseness, in this cohort. We were also able, for the first time, to estimate the contribution of additive genetic and environmental factors to compulsive hoarding, albeit only in female participants. Several conclusions can be drawn from the data.
A Prevalent Problem
Approximately 2% of the twins in this large sample reported hoarding behaviors that may be sufficiently distressing and interfering to represent a significant problem. Their average scores on the HRS-SR (mean=21 out of 40) were similar to those obtained in clinically ascertained hoarding samples (mean=25) (27) . This prevalence estimate is lower than the 5% obtained in an epidemiological study of personality disorders (15) and much lower than the 14% reported in the National Comorbidity Survey Replication (16) . These studies estimated the prevalence of hoarding based on unidimensional measures, which do not assess the broad hoarding phenotype (including clutter and excessive acquisition) and its associated interference and distress. This may have resulted in an overestimation of the prevalence of compulsive hoarding.
We found a significantly greater prevalence of compulsive hoarding problems in men (4.1%) than in women (2.1%), which is consistent with results from another epidemiological study (15) but is in sharp contrast with clinically ascertained hoarding samples, which are almost invariably predominantly female (see references 4 , 8 , 30 , for example). Perhaps women are more likely than men to seek help about their hoarding problems. The identification of people, particularly men, with severe hoarding problems and their engagement with mental health professionals and other agencies represents a substantial challenge for the future.
A Heritable Disorder
The results of the twin analyses suggest that genetic factors account for approximately 50% of the variance in compulsive hoarding, with nonshared environmental factors and measurement error accounting for the other half. Environmental factors shared by siblings growing up in the same family did not contribute to individual differences in the liability to compulsive hoarding, suggesting that these factors may be less important in the etiology of this trait.
Our findings are consistent with those of previous research, indicating that hoarding is a robustly familial condition (see references 4 , 19 , 20 – 22 , for example). In addition, they show, for the first time, that familial resemblance in this respect is mainly due to genetic factors, at least in women. That is, although environmental influences were important, they tended to be of the kind that makes members of the same family different rather than alike. These results are in line with research on obsessive-compulsive disorder and other anxiety disorders, which shows that variability in these traits is best explained by moderate genetic and unique environmental influence, but negligible shared environmental effects (31 , 32) .
A number of molecular genetic studies have begun to identify susceptibility genes for compulsive hoarding in the context of Tourette’s syndrome (33) and obsessive-compulsive disorder (6 , 34 – 36) . Findings from these studies have so far been inconsistent, and further research is clearly needed to identify genes that increase the liability to compulsive hoarding in individuals for whom hoarding occurs independently of other disorders (4 , 15) . Using suitable instruments, such as the HRS-SR, will facilitate this task.
Our results clearly show that nongenetic factors also play an important role in compulsive hoarding. Indeed, nonshared environmental factors and measurement error accounted for up to 50% of the variance. Although the amount of measurement error is unknown, these findings underscore the importance of identifying specific environmental factors that may increase the risk of developing this condition. Recent studies have suggested a possible association between traumatic life events and the onset and severity of compulsive hoarding (37 , 38) . While it is possible that nonshared environmental influences reflect negative life events, further research exploring putative environmental risk factors is clearly needed.
Limitations
Some caveats must be kept in mind when interpreting these results. First, our prevalence estimates are based on a self-report measure rather than a clinician-administered diagnostic interview. Any cutoff used for the measure—even if empirically derived, as ours was—is necessarily arbitrary, and different cutoffs might have produced different prevalence estimates. If compulsive hoarding is included as a discrete disorder in DSM-V (39) and its diagnostic criteria are operationalized, researchers will be able to establish its precise prevalence as a syndrome. Second, twin samples may not be entirely representative of the general population, although the characteristics of the twins in this study have been shown to be similar to those of individuals drawn from an age-matched singleton population (24) . Third, our sample was 90% female, and it was not possible to fit heritability models for women and men separately, because there was insufficient power to examine men alone. Fourth, because compulsive hoarding was measured at a single point in time, it was not possible to estimate measurement error and adjust heritability and nonshared environment estimates accordingly. Our findings should also be interpreted in view of the more general limitations of the twin design (28) . Finally, it must be acknowledged that hoarding symptoms may be the common end product of a variety of organic and psychiatric problems. A certain level of noise may therefore have influenced our heritability estimates.
Conclusions
Compulsive hoarding is highly prevalent in the population. It is also clearly heritable, at least in women, although nonshared environmental factors are also likely to play an important role. It is possible that traumatic experiences or other environmental risk factors interact with particular genes to precipitate compulsive hoarding, and future research should address this. Future studies should also examine the degree of genetic and environmental overlap between compulsive hoarding and other psychiatric symptoms in order to help clarify the nosological status of compulsive hoarding. Finally, genome-wide scans of compulsive hoarding in large community samples are warranted.
1. Frost RO, Hartl TL: A cognitive-behavioral model of compulsive hoarding. Behav Res Ther 1996; 34:341–350Google Scholar
2. Frost RO, Steketee G, Williams LF, Warren R: Mood, personality disorder symptoms, and disability in obsessive compulsive hoarders: a comparison with clinical and nonclinical controls. Behav Res Ther 2000; 38:1071–1081Google Scholar
3. Mataix-Cols D, Baer L, Rauch SL, Jenike MA: Relation of factor-analyzed dimensions of obsessive-compulsive disorder to personality disorders. Acta Psychiatr Scand 2000; 102:199–202Google Scholar
4. Pertusa A, Fullana MA, Singh S, Alonso P, Menchón JM, Mataix-Cols D: Compulsive hoarding: OCD symptom, distinct clinical syndrome, or both? Am J Psychiatry 2008; 165:1289–1298Google Scholar
5. Samuels J, Bienvenu OJ, Riddle M, Cullen B, Grados M, Liang KY, Hoehn-Saric R, Nestadt G: Hoarding in obsessive compulsive disorder: results from a case-control study. Behav Res Ther 2002; 40:517–528Google Scholar
6. Samuels JF, Bienvenu OJ, Pinto A, Fyer AJ, McCracken JT, Rauch SL, Murphy DL, Grados MA, Greenberg BD, Knowles JA, Piacentini J, Cannistraro PA, Cullen B, Riddle MA, Rasmussen SA, Pauls DL, Willour VL, Shugart YY, Liang KY, Hoehn-Saric R, Nestadt G: Hoarding in obsessive-compulsive disorder: results from the OCD collaborative genetics study. Behav Res Ther 2007; 45:673–686Google Scholar
7. Tolin DF, Frost RO, Steketee G, Gray KD, Fitch KE: The economic and social burden of compulsive hoarding. Psychiatry Res 2008; 160:200–211Google Scholar
8. Steketee G, Frost R: Compulsive hoarding: current status of the research. Clin Psychol Rev 2003; 23:905–927Google Scholar
9. Tolin DF, Frost RO, Steketee G, Fitch KE: Family burden of compulsive hoarding: results of an Internet survey. Behav Res Ther 2008; 46:334–344Google Scholar
10. Mataix-Cols D, Rauch SL, Manzo PA, Jenike MA, Baer L: Use of factor-analyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive-compulsive disorder. Am J Psychiatry 1999; 156:1409–1416Google Scholar
11. Mataix-Cols D, Marks IM, Greist JH, Kobak KA, Baer L: Obsessive-compulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: results from a controlled trial. Psychother Psychosom 2002; 71:255–262Google Scholar
12. Saxena S, Maidment KM, Vapnik T, Golden G, Rishwain T, Rosen RM, Tarlow G, Bystritsky A: Obsessive-compulsive hoarding: symptom severity and response to multimodal treatment. J Clin Psychiatry 2002; 63:21–27Google Scholar
13. Tolin DF, Frost RO, Steketee G: An open trial of cognitive-behavioral therapy for compulsive hoarding. Behav Res Ther 2007; 45:1461–1470Google Scholar
14. Saxena S, Brody AL, Maidment KM, Baxter LR Jr: Paroxetine treatment of compulsive hoarding. J Psychiatry Res 2007; 41:481–487Google Scholar
15. Samuels JF, Bienvenu O, Grados MA, Cullen B, Riddle MA, Liang KY, Eaton WW, Nestadt G: Prevalence and correlates of hoarding behavior in a community-based sample. Behav Res Ther 2008; 46:836–844Google Scholar
16. Ruscio AM, Stein DJ, Chiu WT, Kessler RC: The epidemiology of obsessive compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry (Epub ahead of print, Aug 26, 2008)Google Scholar
17. Winsberg ME, Cassic KS, Koran LM: Hoarding in obsessive-compulsive disorder: a report of 20 cases. J Clin Psychiatry 1999; 60:591–597Google Scholar
18. Seedat S, Stein DJ: Hoarding in obsessive-compulsive disorder and related disorders: a preliminary report of 15 cases. Psychiatry Clin Neurosci 2002; 56:17–23Google Scholar
19. Cullen B, Brown CH, Riddle MA, Grados MA, Bienvenu OJ, Hoehn-Saric R, Shugart YY, Liang KY, Samuels J, Nestadt G: Factor analysis of the Yale-Brown Obsessive Compulsive Scale in a family study of obsessive-compulsive disorder. Depress Anxiety 2007; 24:130–138Google Scholar
20. Chacon P, Rosario-Campos MC, Pauls DL, Hounie AG, Curi M, Akkerman F, Shimabokuro FH, de Mathis MA, Lopes AC, Hasler G, Miguel EC: Obsessive-compulsive symptoms in sibling pairs concordant for obsessive-compulsive disorder. Am J Med Genet B Neuropsychiatr Genet 2007; 144B:551–555Google Scholar
21. Hasler G, Pinto A, Greenberg BD, Samuels J, Fyer AJ, Pauls D, Knowles JA, McCracken JT, Piacentini J, Riddle MA, Rauch SL, Rasmussen SA, Willour VL, Grados MA, Cullen B, Bienvenu OJ, Shugart YY, Liang KY, Hoehn-Saric R, Wang Y, Ronquillo J, Nestadt G, Murphy DL; OCD Collaborative Genetics Study: Familiality of factor analysis-derived YBOCS dimensions in OCD-affected sibling pairs from the OCD Collaborative Genetics Study. Biol Psychiatry 2007; 61:617–625Google Scholar
22. Pinto A, Greenberg BD, Grados MA, Bienvenu OJ, Samuels JF, Murphy DL, Hasler G, Stout RL, Rauch SL, Shugart YY, Pauls DL, Knowles JA, Fyer AJ, McCracken JT, Piacentini J, Wang Y, Willour VL, Cullen B, Liang KY, Hoehn-Saric R, Riddle MA, Rasmussen SA, Nestadt G: Further development of YBOCS dimensions in the OCD Collaborative Genetics Study: symptoms vs. categories. Psychiatry Res 2008; 160:83–93Google Scholar
23. Spector TD, Williams FM: The UK Adult Twin Registry (TwinsUK). Twin Res Hum Genet 2006; 9:899–906Google Scholar
24. Andrew T, Hart DJ, Snieder H, de Lange M, Spector TD, MacGregor AJ: Are twins and singletons comparable? a study of disease-related and lifestyle characteristics in adult women. Twin Res Hum Genet 2001; 4:6464–6477Google Scholar
25. Sarna S, Kaprio J, Sistonen P, Koskenvuo M: Diagnosis of twin zygosity by mailed questionnaires. Hum Hered 1978; 28:241–254Google Scholar
26. Noble M, McLennan D, Wilkinson K, Whitworth A, Barnes H, Dibben C: The English Indices of Deprivation 2007. London, Communities and Local Government, 2008 (http://www.communities.gov.uk/documents/communities/pdf/733520.pdf)Google Scholar
27. Tolin D, Frost R, Steketee G: A Brief Interview for Assessing Compulsive Hoarding: The Hoarding Rating Scale–Interview. Psychiatry Res (in press)Google Scholar
28. Rijsdijk FV, Sham PC: Analytic approaches to twin data using structural equation models. Brief Bioinform 2002; 3:119–133Google Scholar
29. Neale MC, Cardon LR: Methodology for genetic studies of twins and families. Dordrecht, the Netherlands, Kluwer Academic, 1992Google Scholar
30. Mataix-Cols D, Nakatani E, Micali N, Heyman I: Structure of obsessive-compulsive symptoms in pediatric OCD. J Am Acad Child Adolesc Psychiatry 2008; 47:773–778Google Scholar
31. van Grootheest DS, Cath DC, Beekman AT, Boomsma DI: Twin studies on obsessive-compulsive disorder: a review. Twin Res Hum Genet 2005; 8:450–458Google Scholar
32. Hettema JM, Neale MC, Kendler KS: A review and meta-analysis of the genetic epidemiology of anxiety disorders. Am J Psychiatry 2001; 158:1568–1578Google Scholar
33. Zhang H, Leckman JF, Pauls DL, Tsai CP, Kidd KK, Campos MR; Tourette Syndrome Association International Consortium for Genetics: Genomewide scan of hoarding in sib pairs in which both sibs have Gilles de la Tourette syndrome. Am J Hum Genet 2002; 70:896–904Google Scholar
34. Liang KY, Wang Y, Shugart YY, Grados M, Fyer AJ, Rauch S, Murphy D, McCracken J, Rasmussen S, Cullen B, Hoehn-Saric R, Greenberg B, Pinto A, Knowles J, Piacentini J, Pauls D, Bienvenu O, Riddle M, Samuels J, Nestadt G: Evidence for potential relationship between SLC1A1 and a putative genetic linkage region on chromosome 14q to obsessive-compulsive disorder with compulsive hoarding. Am J Med Genet B Neuropsychiatr Genet 2008; 5:1000–1002Google Scholar
35. Alonso P, Gratacòs M, Menchón JM, Segalàs C, González JR, Labad J, Bayés M, Real E, de Cid R, Pertusa A, Escaramís G, Vallejo J, Estivill X: Genetic susceptibility to obsessive-compulsive hoarding: the contribution of neurotrophic tyrosine kinase receptor type 3 gene. Genes Brain Behav 2008; 7:778–785Google Scholar
36. Lochner C, Kinnear CJ, Hemmings SM, Seller C, Niehaus DJ, Knowles JA, Daniels W, Moolman-Smook JC, Seedat S, Stein DJ: Hoarding in obsessive-compulsive disorder: clinical and genetic correlates. J Clin Psychiatry 2005; 66:1155–1160Google Scholar
37. Hartl TL, Duffany SR, Allen GJ, Steketee G, Frost RO: Relationships among compulsive hoarding, trauma, and attention-deficit/hyperactivity disorder. Behav Res Ther 2005; 43:269–276Google Scholar
38. Cromer KR, Schmidt NB, Murphy DL: Do traumatic events influence the clinical expression of compulsive hoarding? Behav Res Ther 2007; 45:2581–2592Google Scholar
39. Mataix-Cols D, Pertusa A, Leckman JF: Issues for DSM-V: how should obsessive-compulsive and related disorders be classified? (editorial). Am J Psychiatry 2007; 164:1313–1314Google Scholar





