Exploring the Convergence of Posttraumatic Stress Disorder and Mild Traumatic Brain Injury
Abstract
The authors examine the relationship of the two signature injuries experienced by military personnel serving in Afghanistan and Iraq: posttraumatic stress disorder (PTSD) and mild traumatic brain injury (mild TBI). Studies show that a substantial minority of those serving develop persistent emotional sequelae (such as PTSD and other psychological health problems) and/or somatic or cognitive sequelae (postconcussive symptoms) of traumatic exposure. Remarkably, the mechanism (emotional versus biomechanical) and locus (head versus other regions) of injury are weak determinants of whether an individual develops PTSD, persistent postconcussive symptoms, or both. Preexisting or traumatically acquired cognitive dysfunction can increase the risk for these syndromes, probably by reducing cognitive reserve. Structural and functional neuroimaging studies can be interpreted to explain part of the shared symptomatic and functional variance in these syndromes, but this literature is far from consistent and serves mainly to raise new, challenging questions about mutual pathophysiology. The frequent confluence of PTSD and persistent postconcussive symptoms in military personnel strains the bounds of these constructs. New studies are needed to improve our understanding of how emotional and biomechanical stressors can yield these adverse outcomes and how such outcomes can be prevented and treated.
The conflicts in Iraq and Afghanistan have focused renewed attention on the mental health effects of combat (1) . Evolution in how warfare is conducted, as well as in life-saving gear for military personnel, has resulted in a large and growing cohort of individuals who have been exposed to both psychological and biomechanical trauma (2) . Until recently, the underlying pathophysiology and neuropsychiatric sequelae of psychological and biomechanical trauma have been thought to have little in common, and the co-occurrence of posttraumatic stress disorder (PTSD) and traumatic brain injury (TBI) has been considered a relatively rare clinical event. The purpose of this article is to address this issue. First, we provide an overview of the epidemiology of PTSD and mild TBI, with an emphasis on recent studies of U.S. military personnel. Second, we describe the overlap in symptom profiles between PTSD and mild TBI with the aim of developing a conceptual model for their shared and specific variance in functional outcomes. Third, we point to mutual risk factors for PTSD and mild TBI that, if not appreciated, can confound interpretation of the literature on the interrelationship of these syndromes. Fourth, we refer to several recent structural and functional neuroimaging studies to illustrate how current theories of pathophysiology succeed in some respects (but fail in others) in explaining PTSD and mild TBI comorbidity following traumatic injury. Finally, we highlight future directions for research that hold promise for improving our understanding and treatment of the effects of trauma from both psychological and biomechanical forces.
Literature Review
We conducted a PubMed search using the search terms “etiology,” “epidemiology,” or “treatment” in conjunction with “traumatic brain injury,” “traumatic injury,” “posttraumatic stress disorder,” or “combat stress.” We focused on more recent articles, in particular those that address the comorbid occurrence of PTSD and mild TBI. We used these articles to find links to earlier seminal works. We also reviewed recent reports on PTSD (3 , 4) and traumatic brain injury (5) from the Institute of Medicine, as well as relevant articles known to us from our respective experiences in these fields.
PTSD and TBI Comorbidity in Perspective
There are some discussions of comorbid PTSD and TBI in the literature (6 – 13) , but this association did not come to widespread attention until recent reports from the U.S. military in Afghanistan (Operation Enduring Freedom) and Iraq (Operation Iraqi Freedom) (1 , 14 , 15) . This relative inattention to TBI-PTSD comorbidity may reflect the fact that PTSD has been the province of mental health professionals, whereas TBI has been primarily the purview of neurologists, neurosurgeons, neuropsychologists, and physical medicine and rehabilitation specialists. This professional divide is reflected in the dichotomous use of the term “trauma.” Mental health professionals generally understand trauma to signify an event associated with threat of harm or loss of life associated with extreme fear or horror. Neurologists, neurosurgeons, and physiatrists typically understand trauma to mean the result of destructive biomechanical forces acting on the brain or other parts of the body. Understanding and addressing the coalescence of neuropsychiatric sequelae of both of these types of trauma will require a coming together of these and other specialties in a truly interdisciplinary fashion. In an effort to be precise, we will use the modifiers “psychological” and “biomechanical” when appropriate to avoid confusion. We recognize that these are imperfect terms and imply an etiological connection that is still in question.
Although we refer in this article to several civilian studies, it is unclear to what extent the findings can be generalized to military personnel. Many combatants in the conflicts in Afghanistan and Iraq have seen multiple episodes of wounding and death and have been exposed to multiple shock waves with the potential to cause TBI. Repeated deployments add more opportunities for trauma and the worsening of TBI and PTSD. These military conflicts also highlight an additional potential confounding factor: military populations often have high exposure rates to psychologically traumatic events experienced at time points unrelated to the TBI. In contrast, much of the civilian literature considers the issue of comorbid mild TBI and PTSD from a single event. Additional research is needed to understand the extent to which the recent military literature on mild TBI and PTSD comorbidity can be considered to reflect the joint effects of a single exposure (which, arguably, can have emotionally and biomechanically traumatic aspects) as opposed to cumulative or massed effects of distinct emotional and biomechanical trauma exposures.
Epidemiology and Co-Occurrence of PTSD and Mild TBI
Approximately 7.7 million Americans suffer from PTSD, according to recent population-based survey research (16) . The most common causes of PTSD in the civilian sector are motor vehicle crashes and assaults (including domestic violence and rape), with women approximately twice as likely as men to suffer from PTSD (17) . Surveys of military personnel returning from deployments to Iraq and Afghanistan find prevalence rates of PTSD ranging from 8% to 16% (18 , 19) ; it is likely that these rates are underestimates, given the many barriers to reporting mental health problems in the military (20) . Approximately 15% of these veterans seeking care at Veterans Administration hospitals in the United States have been given a diagnosis of PTSD (21) .
An estimated 1.5 million brain injuries occur every year in the United States, and over 5 million Americans (2% of the population) live with disabilities resulting from TBI (22) . In the civilian sector, the leading causes of TBI are falls, motor vehicle crashes, struck-by-or-against events, and assaults (22) . Interestingly, motor vehicle crashes and assaults are also two of the most common causes of PTSD in the U.S. civilian population (17 , 23) , highlighting the overlap in exposures to TBI- and PTSD-causative events. In the U.S. military, TBI is the most common type of physical injury sustained by combatants in Afghanistan and Iraq, and explosion or blast injury is the most common cause (2) . In a 2006 survey of more than 2,500 recently returned army infantry soldiers, 5% reported injuries with loss of consciousness during a yearlong deployment to Iraq, and 10% reported injuries with altered mental status (14) . A recent RAND report (1) suggested even higher rates (19%) of probable TBI in a 2007 telephone survey of almost 2,000 previously deployed service personnel. A similarly high rate (23%) of clinician-confirmed TBI history in a U.S. Army brigade combat team with at least one deployment corroborates these findings (24) .
Although our focus in this article is on PTSD and mild TBI, it is important clinically to recognize that both disorders are associated with higher rates of other psychological health problems, including depression (5 , 25) , substance abuse (26 , 27) , and suicidal behavior in both civilian (20 , 28) and military populations (29 , 30) . Furthermore, the presence of these comorbid conditions may have an impact on conventional treatments (4) , lending additional impetus to the need to understand these interactions more completely.
The Military Experience in Afghanistan and Iraq
Mild TBI (also known as concussion) is characterized by an alteration in the level of consciousness or loss of consciousness for up to 30 minutes, although definitions vary (31 , 32) . Two recent studies highlight the relationship between PTSD and mild TBI in military samples. The aforementioned study of TBI in U.S. soldiers returning from the Iraq war (14) found that 44% of those who reported loss of consciousness met criteria for PTSD, compared with 27% of those who reported altered mental status, 16% of those with other injuries, and 9% of those with no injury. Remarkably, the investigators found that all observed variance in physical health outcomes and symptoms (with the exception of headache) could be accounted for by the presence of PTSD and/or depression. Data were collected 3–4 months after deployment and thus reflect persistent symptoms. In a study using somewhat different methods of evaluation (15) , investigators found that 12% of a cohort of more than 2,200 veterans returning from Afghanistan and Iraq reported a history consistent with mild TBI, and 11% had probable PTSD. Combat-incurred mild TBI approximately doubled the risk for PTSD, and, interestingly, the strongest factor associated with persistent postconcussive symptoms was PTSD. Even when overlapping symptoms ( Figure 1 ) were removed from the PTSD score, the association between postconcussive and PTSD symptoms remained strong. Although a recently released Institute of Medicine report concluded that there was only limited or suggestive evidence of an association between PTSD and mild TBI in Gulf War military populations (5) , these and other data have led to the labeling of PTSD and TBI as signature injuries of Operation Enduring Freedom and Operation Iraqi Freedom and have forced a reconsideration of the relationship between these two disorders.

Overlap in Symptom Profiles
A common clinical presentation in returning service members is a mixture of symptoms that, using current nomenclature, would be classified as either PTSD or persistent sequelae of mild TBI (i.e., persistent postconcussive symptoms), or both. During World War I, the term “shell shock” might have been applied, referring to a syndrome that featured fatigue, indecision, and irritability among its symptoms (33) . In this regard, it could be argued that the current (DSM-IV) diagnostic criteria for PTSD fail to adequately capture the range and configuration of symptoms attributable to 21st-century military combat and that a return to criteria that incorporate postconcussive symptoms would render moot any dialogue about PTSD and mild TBI comorbidity. In fact, there is an affinity in today’s U.S. military to eschew use of the term “PTSD” in favor of the term “combat stress reaction.” The use of this term has the dual advantage of incorporating some of the more mild TBI-like symptoms and of being potentially less stigmatizing. It remains to be seen to what extent “combat stress reaction” gains a foothold in the mental health nomenclature, including DSM-V. A recent Institute of Medicine report (3) concluded that there was good evidence in support of the construct validity and diagnostic criteria for PTSD, although most experts agree that there is room for improvement (34 , 35) . In the interim, a careful examination of the temporal, symptomatic, and preexisting risk factors that might underlie the frequent conjunction of PTSD and mild TBI is in order.
Trajectory of Development and Temporal Antecedents
Consideration of the time interval from the putative event (biomechanical or psychological) to the point of assessment is critical in the diagnosis of mild TBI and/or PTSD. The diagnosis of mild TBI is based on the reporting of symptoms that occur at the time of the event (i.e., altered level or loss of consciousness at the time of application of biomechanical force). In a similar vein, PTSD requires exposure to an event to which the individual responds with extreme fear, helplessness, or horror—the A2 criterion (which, it should be noted, has been criticized as superfluous for diagnosis [ 36 , 37 ]). In both instances, this reporting is often retrospective, sometimes months or even years after the event. Thus, although exposure to a sufficient (and it is quite unclear what is sufficient) biomechanical or psychological trauma is paramount for diagnosis of both these disorders, the exposure itself is rarely documented, raising serious questions about the reliability of recall.
Perhaps even more worrisome is the circularity inherent in diagnosis. If an individual has symptoms that might have resulted from a qualifying exposure, then it may be assumed that the exposure did indeed occur. Taken to its extreme, this line of reasoning has historically led to “epidemics” of falsely remembered childhood sexual or ritual abuse among individuals with emotional problems. It remains to be seen whether veterans of the current conflicts will be assumed to have sustained a TBI if they experience cognitive symptoms following their military experiences. But considerable data suggest that this assumption would be erroneous.
Most individuals who suffer a mild TBI have resolution of any anterograde amnesia within 24 hours. Some may note lingering symptoms, such as headache, disequilibrium, cognitive slowing, fatigue, and irritability (for reviews, see references 38, 39), which remit over the subsequent days to weeks. But a minority of individuals, usually thought to be about 10%–15% of those with a mild TBI, will experience chronic, persistent symptoms 1 year or more following injury; this is often referred to as the (persistent) postconcussive syndrome. The use of this term suggests a consistency of clinical presentation and, more important, an etiology that is not readily supported by the literature. A more accurate view may be that in some cases, symptoms that commonly result from injury to brain regions vulnerable to biomechanical forces associated with mild TBI persist and can become chronic. But a large body of empirical research also shows that some of these symptoms may occur following other types of emotional injury or physical injury to areas other than the head (40) . A recent study of military personnel from the United Kingdom who were deployed to Iraq found that although symptoms often associated with a concussion were common in deployed service personnel, they were as likely to be associated with in-theater experiences that did not involve biomechanical force to the head (e.g., exposure to depleted uranium; aiding the wounded) as they were to blast exposure (41) .
These data clearly indicate the nonspecific nature of postconcussive symptoms, a point that has been made in the civilian literature for years (42) . Moreover, they point to an etiological fallacy that impugns serious discussion about the relationship between PTSD and mild TBI: the fallacy is that the former is caused by psychological injury to the psyche and the latter by biomechanical injury to the brain. But the literature clearly shows that either persistent postconcussive symptoms (i.e., the failure to recover from acute mild TBI symptoms) or PTSD—and other psychological health problems, such as major depression and alcohol abuse—can occur following either emotional or physical trauma (which may or may not involve injury to the brain [43] ). Unclear at present is whether particular characteristics of the exposure or of the individual determine which set of symptoms will predominate and persist.
Risk Factors for Persistent Symptoms
It has been long held in the civilian literature that one predictor of persistent symptoms following mild TBI (i.e., postconcussive symptoms) is the development of psychiatric disorders such as depression and PTSD (39) . This, of course, raises the question of whether the persistent symptoms are better attributed to the remote mild TBI with failure to resolve, to comorbid conditions such as PTSD and depression, or to a combination of these factors. It also raises the question of why there is an increased rate of psychiatric disorders in individuals who have sustained a TBI (14 , 44 , 45) .
There are parallels found in the response to psychological trauma. Acute stress disorder is similar to mild TBI in the way it is configured and diagnosed, in that the diagnosis depends on symptoms that are to have occurred immediately or shortly after the psychological trauma. The diagnosis of PTSD, however, is in large part based on symptoms that fail to resolve at some time point distal to the psychological trauma. As shown in Figure 1 , there is such marked definitional overlap between PTSD and postconcussive symptoms that it goes without saying that many persons who sustain a brain injury will have symptoms of both. Accurate attribution of causality, however, requires knowledge of the typical trajectory of recovery after mild TBI and knowledge of other confounding factors. Interestingly, since mild TBI is almost always associated with pain at the time of injury (as well as chronic pain later) (46) , and since pain at the time of injury is a risk factor for developing PTSD (47) , this would further serve to heighten the likelihood of the co-occurrence of both disorders. It is also worth noting that if the diagnostic criteria for PTSD are simplified in DSM-V to address critiques about its awkward construction and relatively poor utility for identifying persons with impairment following trauma (48 , 49) , the apparent comorbidity between mild TBI and PTSD may be even further accentuated.
Neuropsychological Dysfunction
Although the role of psychological and emotional factors—within and beyond the best-studied domains of PTSD and depression—in failure to recover from presumed mild TBI is being increasingly acknowledged, this by no means excludes an important role for neurological injury. Researchers have suggested that mild TBI may diminish the capacity to employ cognitive resources that would normally be engaged in problem-solving and regulating emotions after trauma, thereby leaving an individual more susceptible to PTSD and related problems (50) ( Figure 2 ).
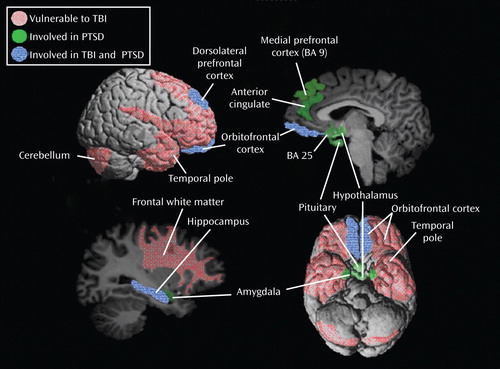
a Several brain regions have been consistently implicated in PTSD (green) including the amygdala, the hippocampus, the orbitofrontal cortex, and the dorsolateral and dorsomedial prefrontal cortex. Several brain regions are vulnerable to the typical biomechanical forces associated with TBI (red), including the orbitofrontal cortex, the dorsolateral prefrontal cortex, the temporal pole, and the hippocampus. Overlap areas (blue) include the orbitofrontal cortex, the dorsolateral prefrontal cortex, and the hippocampus. In addition, tracts connecting the amygdala and the medial prefrontal cortex course through the subfrontal white matter and are thus vulnerable to disruption by TBI. BA=Brodmann’s area.
The role of cognitive and emotional information processing in the genesis of symptoms in both PTSD and persistent sequelae of mild TBI is worth commenting on. Both biomechanical and psychological trauma can result in impaired information processing. Most individuals who suffer a mild TBI have acute cognitive effects, and a significant number (estimated to be 10%–15% of all those injured) have persistent cognitive and behavioral complaints. Several areas of cognitive impairment are frequently reported, including working and short-term memory, speed of information processing, attention, and executive function (5) . Numerous (though by no means all) studies have found evidence of neuropsychological impairment in persons with PTSD (51) . But many such studies almost certainly failed to inquire sufficiently about the possibility of mild TBI (52) , making interpretation of this literature subject to conjecture. In addition, there is an appreciation that there can be cognitive effects of deployment to a theater of operations apart from exposure to mild TBI or development of PTSD (53) .
Cognitive Dysfunction: Risk Factor or Consequence?
There is a confluence of data in PTSD (but surprisingly little data in mild TBI [54] ) showing that IQ prior to trauma exposure is inversely associated with risk for subsequent PTSD and related psychological health problems. Kremen et al. (55) found that preenlistment cognitive ability (as measured by the Armed Forces Qualifying Test) in Vietnam veterans showed a dose-response relationship with risk for PTSD; those in the highest quartile of cognitive ability had a 48% lower risk than those in the lowest quartile). Similarly, in a study of male Vietnam veterans, Gale et al. (56) found that a one-standard-deviation decrease in cognitive ability was associated with a 39% increase in risk of prospectively ascertained PTSD. These findings also extend to nonmilitary samples. In a prospective longitudinal study of Michigan youths, Breslau et al. (57) found that higher IQ at age 6 was associated with a substantially reduced risk (odds ratio 0.2, 95% confidence interval 0.1–0.9) of developing PTSD after trauma exposure. Similarly, in a prospective study of a New Zealand birth cohort, Koenen et al. (58) found that low IQ at age 5 was a significant predictor of risk for PTSD through age 32. These data are consistent with a “cognitive reserve” hypothesis of neuropsychiatric disorders, namely, that individual differences in brain structure and function can buffer the effects of neuropathology—which seems to hold true for a variety of mental disorders (59) . It is not at all unreasonable to expect that lower cognitive reserve, whether congenital or acquired (e.g., via mild TBI), would increase risk for adverse mental health outcomes and, more broadly, functional outcomes. A brief discussion of the neural systems thought to be involved in the pathophysiology of PTSD and mild TBI can further sharpen this dialectic by pointing to particular brain regions that might be affected.
Neuroimaging Studies
PTSD
Numerous functional imaging studies point to overactivity of the amygdala and insular cortex as integral to most cases of PTSD (60 – 63) . Another well-replicated finding in PTSD is the underactivity of cortical regions, such as the anterior cingulate and other parts of the ventromedial prefrontal cortex thought to regulate the expression of fear by limbic regions (60 , 61 , 64) . It is possible that preexisting volumetric abnormalities in some of these regions (e.g., the pregenual anterior cingulate and the insular cortex) may constitute risk factors for the development of PTSD following trauma exposure (65) .
With these data in mind, it should be possible to make neuroanatomically specific hypotheses about the risk of PTSD depending on the location of brain lesions. But this is where the extant theory falls short of the (relatively few) studies that have attempted to test such hypotheses. The most problematic of these is a recent report from the Vietnam Head Injury Study in which PTSD symptoms were studied in a sample of 193 Vietnam War veterans who suffered penetrating brain injuries and emotionally traumatic events (66) . Sixty-two patients met DSM-IV criteria for PTSD according to a structured diagnostic interview, and 131 did not. The investigators categorized patients into three groups based on locus of injury: amygdala, ventromedial prefrontal cortex, and nonamygdala/non-ventromedial prefrontal cortex groups; the three groups were comparable on several other PTSD risk factors (combat exposure severity, length of time served in Vietnam, and Armed Forces Qualifying Test scores). Based on the literature described above, the investigators hypothesized that lesions to the amygdala would reduce risk of PTSD and lesions to the ventromedial prefrontal cortex would increase risk of PTSD. They found, consistent with their hypothesis, that veterans with amygdala damage were significantly less likely to develop PTSD than veterans with damage to other parts of the brain. But ventromedial prefrontal cortical lesions were associated with a reduced likelihood of PTSD (as well as with a reduced risk of major depression [67] )—a finding clearly contrary to their hypothesis. The investigators concluded that amygdala-ventromedial prefrontal cortical circuitry seems important in the pathogenesis of PTSD but that more research is needed to understand the nature of the interaction of the two structures in the genesis and maintenance of PTSD (66) . We would also point out that whereas that particular study focused on focal (penetrating) lesions, diffuse injury to connective, integrative white matter tracts seems to be the modal form of damage in most blast-related (military) and concussive (civilian) mild TBI. For the purposes of our discussion here, we must acknowledge the inadequacy of current neural systems models of PTSD to accommodate these new data and to explain the extensive comorbidity seen between PTSD and mild TBI.
Mild TBI
MRI-based structural techniques, such as diffusion tensor imaging (68) and voxel-based morphometry (69) , and functional imaging techniques, such as positron emission tomography (70) and functional MRI (71) , have been used to study the mechanism of neurobehavioral complaints persisting beyond the usual recovery trajectory (for a review, see reference 72 ). Although the conclusions that can be drawn from these studies are limited by several methodological issues, this literature does suggest that brain regions vulnerable to the impact and inertial biomechanical forces associated with TBI show higher rates of both structural and functional abnormalities (72) . Of particular interest is the observation that the orbital prefrontal cortex and related circuitry (subcortical white matter, basal ganglia, and thalamus) are particularly vulnerable to biomechanical forces commonly associated with TBI (32) , which probably accounts for the prevalence of executive deficits after TBI and contributes to the high rates of emotional and neurobehavioral dysregulation (e.g., depression and PTSD) after injury. Much work, however, remains to be done to clarify the clinical and functional significance of altered structure and function. Careful assessment of injury type and severity, premorbid history of cerebral insults (e.g., repetitive concussions), comorbid conditions (depression, PTSD, substance abuse, and so on), and assessment intervals will be critical.
Future Directions
To advance our understanding of PTSD and mild TBI and their interaction, it will be critical for investigators to attend to both “disorders” when designing and implementing research studies. Because knowledge in these areas is distributed across numerous domains of expertise (psychiatry, neuropsychology, neurology, neurosurgery, and physical medicine and rehabilitation, to name just a few), interdisciplinary research teams will be required and funding mechanisms that support this type of “team science” will be needed.
When these interdisciplinary teams coalesce, their first task will be to operationalize definitions and constructs such that a common “language” is established. In conjunction with this effort, better methods will have to be developed to verify the actual occurrence of TBI (73) . Their next task will be to design studies of brain-injured patients that cover a comprehensive set of risk factors and outcomes. Ideal designs would be prospective, following individuals from the time of injury (or earlier, if populations sufficiently at risk for head injury can be engaged in research) to 12 or 24 months, or longer, into the future. Outcome measures should be symptomatic and functional and should be combined with imaging and psychophysiologic tools that have the potential to reveal similarities and differences in brain structure and function that may discriminate PTSD and persistent symptoms following mild TBI.
One of the most promising tools in this regard is diffusion tensor imaging. This technique permits the tracing of fiber tracts and the quantification of disturbance in their anisotropy, thereby providing a putative biomarker of white matter tract damage (74) . There have been several studies using diffusion tensor imaging in PTSD or mild TBI (75 – 77) , but they have been small and none has yet included samples and measures sufficient to determine the utility of the technique for differentiating these syndromes. This will be a priority for future research, as will the design and implementation of studies capable of spanning the full array of “combat stress reaction” symptoms as possible outcome measures.
As we await the completion of studies that illuminate the pathophysiology of these disorders and their intersection, what can we do to advance clinical therapeutics in persons with combined mild TBI and PTSD? One approach would be to capitalize on the recognition that much distress and dysfunction in persons with persistent postconcussive symptoms is attributable to emotional disorders such as PTSD and major depression and to empirically test the application of evidence-based therapies (e.g., appropriate antidepressants and cognitive-behavioral therapies) for these conditions in such individuals. Another approach would be to design clinical trials using available therapeutics aimed at ameliorating common domains of dysfunction (e.g., stimulants for attentional problems, hypnotics for insomnia, and anticonvulsants for mood dysregulation), taking into consideration the possible pitfalls of such approaches (e.g., risk of substance abuse and dependence with stimulants or hypnotics).
Over time, these lines of research will converge to raise the inevitable question “Are there different etiologies for PTSD?” Is PTSD that is caused by the emotional trauma of being held up at gunpoint the same as PTSD caused by a car bomb that renders the victim unconscious for 10 minutes? Can our conceptual models accommodate the existence of a disorder that can be caused by psychological and/or physical injury? It may be that research leads us to conclude that injury to the brain resulting from psychological and physical “stress” involves a common set of pathophysiological (e.g., excitotoxic, such as glutamatergic [78] ) culprits and that therapies that target neurogenesis in damaged regions will prove beneficial (79) . But it is just as likely that we will learn that PTSD associated with mild TBI is a unique form of illness (harkening back to the World War I concept of “shell shock” or its more modern incarnation, “combat stress reaction”) that will continue to challenge our conceptualizations of psyche and soma, and of brain and mind.
1. Tanielian T, Jaycox LH (eds): The Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, Calif, RAND, 2008Google Scholar
2. Warden D: Military TBI during the Iraq and Afghanistan wars. J Head Trauma Rehabil 2006; 21:398–402Google Scholar
3. Subcommittee on Posttraumatic Stress Disorder of the Committee on Gulf War and Health—Physiologic, Psychologic, and Psychosocial Effects of Deployment-Related Stress (Institute of Medicine): Posttraumatic Stress Disorder: Diagnosis and Assessment. Washington, DC, National Academies Press, 2006Google Scholar
4. Committee on Treatment of Posttraumatic Stress Disorder (Institute of Medicine): Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence. Washington, DC, National Academies Press, 2007Google Scholar
5. Committee on Gulf War and Health (Institute of Medicine): Gulf War and Health, vol 7, Long-Term Consequences of Tramautic Brain Injury. Washington, DC, National Academies Press, 2008Google Scholar
6. Bryant RA: Posttraumatic stress disorder and traumatic brain injury: can they co-exist? Clin Psychol Rev 2001; 21:931–948Google Scholar
7. Harvey AG, Brewin CR, Jones C, Kopelman MD: Coexistence of posttraumatic stress disorder and traumatic brain injury: towards a resolution of the paradox. J Int Neuropsychol Soc 2003; 9:663–676Google Scholar
8. Jones C, Harvey AG, Brewin CR: Traumatic brain injury, dissociation, and posttraumatic stress disorder in road traffic accident survivors. J Trauma Stress 2005; 18:181–191Google Scholar
9. Kennedy JE, Jaffee MS, Leskin GA, Stokes JW, Leal FO, Fitzpatrick PJ: Posttraumatic stress disorder and posttraumatic stress disorder-like symptoms and mild traumatic brain injury. J Rehabil Res Dev 2007; 44:895–920Google Scholar
10. Moore EL, Terryberry-Spohr L, Hope DA: Mild traumatic brain injury and anxiety sequelae: a review of the literature. Brain Inj 2006; 20:117–132Google Scholar
11. Williams WH, Evans JJ, Needham P, Wilson BA: Neurological, cognitive, and attributional predictors of posttraumatic stress symptoms after traumatic brain injury. J Trauma Stress 2002; 15:397–400Google Scholar
12. Bombardier CH, Fann JR, Temkin N, Esselman PC, Pelzer E, Keough M, Dikmen S: Posttraumatic stress disorder symptoms during the first six months after traumatic brain injury. J Neuropsychiatry Clin Neurosci 2006; 18:501–508Google Scholar
13. Sumpter RE, McMillan TM: Errors in self-report of post-traumatic stress disorder after severe traumatic brain injury. Brain Inj 2006; 20:93–99Google Scholar
14. Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA: Mild traumatic brain injury in US soldiers returning from Iraq. N Engl J Med 2008; 358:453–463Google Scholar
15. Schneiderman AI, Braver ER, Kang HK: Understanding sequelae of injury mechanisms and mild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: persistent postconcussive symptoms and posttraumatic stress disorder. Am J Epidemiol 2008; 167:1446–1452Google Scholar
16. Kessler RC, Berglund P, Demler O, Jin R, Walters EE: Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry 2005; 62:593–602Google Scholar
17. Galea S, Ahern J, Tracy M, Hubbard A, Cerda M, Goldmann E, Vlahov D: Longitudinal determinants of posttraumatic stress in a population-based cohort study. Epidemiology 2008; 19:47–54Google Scholar
18. Milliken CS, Auchterlonie JL, Hoge CW: Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA 2007; 298:2141–2148Google Scholar
19. Smith TC, Ryan MA, Wingard DL, Slymen DJ, Sallis JF, Kritz-Silverstein D: New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: prospective population based US military cohort study. BMJ 2008; 336:366–371Google Scholar
20. Sareen J, Cox BJ, Afifi TO, Stein MB, Belik SL, Meadows G, Asmundson GJ: Combat and peacekeeping operations in relation to prevalence of mental disorders and perceived need for mental health care: findings from a large representative sample of military personnel. Arch Gen Psychiatry 2007; 64:843–852Google Scholar
21. Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C: Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med 2007; 167:476–482Google Scholar
22. Langlois JA, Rutland-Brown W, Wald MM: The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil 2006; 21:375–378Google Scholar
23. Breslau N, Peterson EL, Poisson LM, Schultz LR, Lucia VC: Estimating post-traumatic stress disorder in the community: lifetime perspective and the impact of typical traumatic events. Psychol Med 2004; 34:889–898Google Scholar
24. Terrio H, Brenner LA, Ivins BJ, Cho JM, Helmick K, Schwab K, Scally K, Bretthauer R, Warden D: Traumatic brain injury screening: preliminary findings in a US army brigade combat team. J Head Trauma Rehabil 2009; 24:14–23Google Scholar
25. Kim E, Lauterbach EC, Reeve A, Arciniegas DB, Coburn KL, Mendez MF, Rummans TA, Coffey EC: Neuropsychiatric complications of traumatic brain injury: a critical review of the literature (a report by the ANPA Committee on Research). J Neuropsychiatry Clin Neurosci 2007; 19:106–127Google Scholar
26. Mills KL, Teesson M, Ross J, Peters L: Trauma, PTSD, and substance use disorders: findings from the Australian National Survey of Mental Health and Well-Being. Am J Psychiatry 2006; 163:651–658Google Scholar
27. Graham DP, Cardon AL: An update on substance use and treatment following traumatic brain injury. Ann NY Acad Sci 2008; 1141:148–162Google Scholar
28. Simpson G, Tate R: Suicidality in people surviving a traumatic brain injury: prevalence, risk factors, and implications for clinical management. Brain Inj 2007; 21:1335–1351Google Scholar
29. Desai RA, Dausey D, Rosenheck RA: Suicide among discharged psychiatric inpatients in the Department of Veterans Affairs. Mil Med 2008; 173:721–728Google Scholar
30. Gutierrez PM, Brenner LA, Huggins JA: A preliminary investigation of suicidality in psychiatrically hospitalized veterans with traumatic brain injury. Arch Suicide Res 2008; 12:336–343Google Scholar
31. Warden DL, French L: Traumatic brain injury in the war zone. N Engl J Med 2005; 353:633–634Google Scholar
32. Bigler ED: Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. J Int Neuropsychol Soc 2008; 14:1–22Google Scholar
33. Benedek DM, Ursano RJ, Holloway H: Military and disaster psychiatry, in Comprehensive Textbook of Psychiatry, 8th ed. Edited by Sadock H, Kaplan BJ. New York, Lippincott Williams & Williams, 2004, pp 2426–2435Google Scholar
34. Spitzer RL, Rosen GM, Lilienfeld SO: Revisiting the Institute of Medicine report on the validity of posttraumatic stress disorder. Compr Psychiatry 2008; 49:319–320Google Scholar
35. North CS, Suris AM, Davis M, Smith RP: Toward validation of the diagnosis of posttraumatic stress disorder. Am J Psychiatry 2009; 166:34–41Google Scholar
36. Breslau N, Kessler RC: The stressor criterion in DSM-IV posttraumatic stress disorder: an empirical investigation. Biol Psychiatry 2001; 50:699–704Google Scholar
37. Adler AB, Wright KM, Bliese PD, Eckford R, Hoge CW: A2 diagnostic criterion for combat-related posttraumatic stress disorder. J Trauma Stress 2008; 21:301–308Google Scholar
38. Alexander MP: Mild traumatic brain injury: pathophysiology, natural history, and clinical management. Neurol 1995; 45:1253–1260Google Scholar
39. McAllister TW, Arciniegas D: Evaluation and treatment of postconcussive symptoms. Neurorehabilitation 2002; 17:265–283Google Scholar
40. McCrea M: Mild Traumatic Brain Injury and Post-Concussion Syndrome: The New Evidence Base for Diagnosis and Treatment. New York, Oxford University Press, 2008Google Scholar
41. Fear NT, Jones E, Groom M, Greenberg N, Hull L, Hodgetts TJ, Wessely S: Symptoms of post-concussional syndrome are non-specifically related to mild traumatic brain injury in UK Armed Forces personnel on return from deployment in Iraq: an analysis of self-reported data. Psychol Med (Epub ahead of print, Oct 23, 2008)Google Scholar
42. Mittenberg W, DiGiulio DV, Perrin S, Bass AE: Symptoms following mild head injury: expectation as aetiology. J Neurol Neurosurg Psychiatry 1992; 55:200–204Google Scholar
43. Zatzick DF, Rivara FP, Nathens AB, Jurkovich GJ, Wang J, Fan MY, Russo J, Salkever DS, MacKenzie EJ: A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychol Med 2007; 37:1469–1480Google Scholar
44. Fann JR, Burington B, Leonetti A, Jaffe K, Katon WJ, Thompson RS: Psychiatric illness following traumatic brain injury in an adult health maintenance organization population. Arch Gen Psychiatry 2004; 61:53–61Google Scholar
45. Koponen S, Taiminen T, Portin R, Himanen L, Isoniemi H, Heinonen H, Hinkka S, Tenovuo O: Axis I and II psychiatric disorders after traumatic brain injury: a 30-year follow-up study. Am J Psychiatry 2002; 159:1315–1321Google Scholar
46. Nampiaparampil DE: Prevalence of chronic pain after traumatic brain injury: a systematic review. JAMA 2008; 300:711–719Google Scholar
47. Norman SB, Stein MB, Dimsdale JE, Hoyt DB: Pain in the aftermath of trauma is a risk factor for post-traumatic stress disorder. Psychol Med 2008; 38:533–542Google Scholar
48. Norman SB, Stein MB, Davidson JR: Profiling posttraumatic functional impairment. J Nerv Ment Dis 2007; 195:48–53Google Scholar
49. Elhai JD, Grubaugh AL, Kashdan TB, Frueh BC: Empirical examination of a proposed refinement to DSM-IV posttraumatic stress disorder symptom criteria using the National Comorbidity Survey replication data. J Clin Psychiatry 2008; 69:597–602Google Scholar
50. Bryant RA: Disentangling mild traumatic brain injury and stress reactions. N Engl J Med 2008; 358:525–527Google Scholar
51. Vasterling JJ, Brailey K: Neuropsychological Findings in Adults With PTSD. New York, Guilford, 2005Google Scholar
52. Powell JM, Ferraro JV, Dikmen SS, Temkin NR, Bell KR: Accuracy of mild traumatic brain injury diagnosis. Arch Phys Med Rehabil 2008; 89:1550–1555Google Scholar
53. Vasterling JJ, Proctor SP, Amoroso P, Kane R, Heeren T, White RF: Neuropsychological outcomes of army personnel following deployment to the Iraq war. JAMA 2006; 296:519–529Google Scholar
54. Hall RC, Hall RC, Chapman MJ: Definition, diagnosis, and forensic implications of postconcussional syndrome. Psychosomatics 2005; 46:195–202Google Scholar
55. Kremen WS, Koenen KC, Boake C, Purcell S, Eisen SA, Franz CE, Tsuang MT, Lyons MJ: Pretrauma cognitive ability and risk for posttraumatic stress disorder: a twin study. Arch Gen Psychiatry 2007; 64:361–368Google Scholar
56. Gale CR, Deary IJ, Boyle SH, Barefoot J, Mortensen LH, Batty GD: Cognitive ability in early adulthood and risk of 5 specific psychiatric disorders in middle age: the Vietnam Experience Study. Arch Gen Psychiatry 2008; 65:1410–1418Google Scholar
57. Breslau N, Lucia VC, Alvarado GF: Intelligence and other predisposing factors in exposure to trauma and posttraumatic stress disorder: a follow-up study at age 17 years. Arch Gen Psychiatry 2006; 63:1238–1245Google Scholar
58. Koenen KC, Moffitt TE, Poulton R, Martin J, Caspi A: Early childhood factors associated with the development of post-traumatic stress disorder: results from a longitudinal birth cohort. Psychol Med 2007; 37:181–192Google Scholar
59. Koenen KC, Moffitt TE, Roberts AL, Martin LT, Kubzansky L, Harrington H, Poulton R, Caspi A: Childhood IQ and adult mental disorders: a test of the cognitive reserve hypothesis. Am J Psychiatry 2009; 166:50–57Google Scholar
60. Etkin A, Wager TD: Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry 2007; 164:1476–1488Google Scholar
61. Mathew SJ, Price RB, Charney DS: Recent advances in the neurobiology of anxiety disorders: implications for novel therapeutics. Am J Med Genet C Semin Med Genet 2008; 148:89–98Google Scholar
62. Simmons AN, Paulus MP, Thorp SR, Matthews SC, Norman SB, Stein MB: Functional activation and neural networks in women with posttraumatic stress disorder related to intimate partner violence. Biol Psychiatry 2008; 64:681–690Google Scholar
63. Rauch SL, Shin LM, Phelps EA: Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research—past, present, and future. Biol Psychiatry 2006; 60:376–382Google Scholar
64. Liberzon I, Sripada CS: The functional neuroanatomy of PTSD: a critical review. Prog Brain Res 2008; 167:151–169Google Scholar
65. Kasai K, Yamasue H, Gilbertson MW, Shenton ME, Rauch SL, Pitman RK: Evidence for acquired pregenual anterior cingulate gray matter loss from a twin study of combat-related posttraumatic stress disorder. Biol Psychiatry 2008; 63:550–556Google Scholar
66. Koenigs M, Huey ED, Raymont V, Cheon B, Solomon J, Wassermann EM, Grafman J: Focal brain damage protects against post-traumatic stress disorder in combat veterans. Nat Neurosci 2008; 11:232–237Google Scholar
67. Koenigs M, Huey ED, Calamia M, Raymont V, Tranel D, Grafman J: Distinct regions of prefrontal cortex mediate resistance and vulnerability to depression. J Neurosci 2008; 28:12341–12348Google Scholar
68. Kraus MF, Susmaras T, Caughlin BP, Walker CJ, Sweeney JA, Little DM: White matter integrity and cognition in chronic traumatic brain injury: a diffusion tensor imaging study. Brain 2007; 130:2508–2519Google Scholar
69. Gale SD, Baxter L, Roundy N, Johnson SC: Traumatic brain injury and grey matter concentration: a preliminary voxel based morphometry study. J Neurol Neurosurg Psychiatry 2005; 76:984–988Google Scholar
70. Chen SH, Kareken DA, Fastenau PS, Trexler LE, Hutchins GD: A study of persistent post-concussion symptoms in mild head trauma using positron emission tomography. J Neurol Neurosurg Psychiatry 2003; 74:326–332Google Scholar
71. McAllister TW, Flashman LA, McDonald BC, Saykin AJ: Mechanisms of working memory dysfunction after mild and moderate TBI: evidence from functional MRI and neurogenetics. J Neurotrauma 2006; 23:1450–1467Google Scholar
72. Belanger HG, Vanderploeg RD, Curtiss G, Warden DL: Recent neuroimaging techniques in mild traumatic brain injury. J Neuropsychiatry Clin Neurosci 2007; 19:5–20Google Scholar
73. Hoge CW, Goldberg HM, Castro CA: Care of war veterans with mild traumatic brain injury: flawed perspectives. N Engl J Med 2009; 360:1588–1591Google Scholar
74. Huisman TA, Schwamm LH, Schaefer PW, Koroshetz WJ, Shetty-Alva N, Ozsunar Y, Wu O, Sorensen AG: Diffusion tensor imaging as potential biomarker of white matter injury in diffuse axonal injury. AJNR Am J Neuroradiol 2004; 25:370–376Google Scholar
75. Abe O, Yamasue H, Kasai K, Yamada H, Aoki S, Iwanami A, Ohtani T, Masutani Y, Kato N, Ohtomo K: Voxel-based diffusion tensor analysis reveals aberrant anterior cingulum integrity in posttraumatic stress disorder due to terrorism. Psychiatry Res 2006; 146:231–242Google Scholar
76. Rutgers DR, Toulgoat F, Cazejust J, Fillard P, Lasjaunias P, Ducreux D: White matter abnormalities in mild traumatic brain injury: a diffusion tensor imaging study. AJNR Am J Neuroradiol 2008; 29:514–519Google Scholar
77. Wilde EA, McCauley SR, Hunter JV, Bigler ED, Chu Z, Wang ZJ, Hanten GR, Troyanskaya M, Yallampalli R, Li X, Chia J, Levin HS: Diffusion tensor imaging of acute mild traumatic brain injury in adolescents. Neurology 2008; 70:948–955Google Scholar
78. Bremner JD, Elzinga B, Schmahl C, Vermetten E: Structural and functional plasticity of the human brain in posttraumatic stress disorder. Prog Brain Res 2008; 167:171–186Google Scholar
79. Ravindran LN, Stein MB: Pharmacotherapy of PTSD: premises, principles, and priorities. Brain Res 2009 (Epub ahead of print, Mar 27, 2009)Google Scholar



