Systematic Review and Meta-Analysis of Multiple-Session Early Interventions Following Traumatic Events
Abstract
Objective: The authors sought to determine the efficacy of multiple-session psychological interventions to prevent and treat traumatic stress symptoms beginning within 3 months of a traumatic event. Method: Nine computerized databases were searched, and manual searches were conducted of reference lists of selected articles as well as two journals. In addition, key researchers in the field were contacted to determine whether they were aware of other relevant studies. The reviewers identified randomized controlled trials of multiple-session psychological treatments aimed at preventing or reducing traumatic stress symptoms in individuals within 3 months of exposure to a traumatic event. Details of the studies were independently extracted by two reviewers, and outcome data were entered into the Review Manager software package. Quality assessment was also conducted by two researchers independently. Results: Twenty-five studies examining a range of interventions were identified. For treatment of individuals exposed to a trauma irrespective of their symptoms, there was no significant difference between any intervention and usual care. For treatment of traumatic stress symptoms irrespective of diagnosis, trauma-focused cognitive-behavioral therapy (CBT) was more effective than waiting list or supportive counseling conditions. The difference was greatest for treatment of acute stress disorder and acute posttraumatic stress disorder. Conclusions: Trauma-focused CBT within 3 months of a traumatic event appears to be effective for individuals with traumatic stress symptoms, especially those who meet the threshold for a clinical diagnosis.
There is now a large body of literature to show that a variety of traumatic experiences can cause significant psychological difficulties for large numbers of people (see references 1 – 6 , for example). Many individuals show great resilience in the face of such experiences and will manifest short-lived or subclinical stress reactions that diminish over time (7) , and most people recover without medical or psychological assistance (8) . Nevertheless, a range of psychological difficulties may develop following trauma in some of those who have been exposed, including acute stress disorder and posttraumatic stress disorder (PTSD). The rate of acute stress disorder has been reported to be 13% in motor vehicle accident survivors (9) and 19% in victims of violent crime (10) . Reported rates of acute PTSD (defined as PTSD symptoms for less than 3 months) have varied across different trauma populations, from 23% in motor vehicle accident victims (6) to 47% in rape victims (11) . Epidemiological research suggests that one-third of individuals who develop acute PTSD remain symptomatic for 6 years or longer (12) . The impact on social, interpersonal, and occupational functioning can be marked and enduring for those who develop chronic PTSD (13) .
Over the past three decades, clinicians have been increasingly involved in attempts to develop interventions that might mitigate the effects of trauma and prevent the onset of chronic PTSD. Although psychological debriefing (also known as critical incident stress debriefing) was a widely used intervention for some years, it came under increasing scrutiny in the 1990s. Systematic reviews (14 , 15) failed to find evidence for the efficacy of single-session individual debriefing, and many experts in the field now caution against its use (16 , 17) . Increasingly the field has turned its attention to other models of intervention (13 , 18 – 21) . A common theme has been the suggestion that efforts should be focused on identifying those most at risk of developing ongoing problems in the aftermath of traumatic incidents and directing resources and interventions mainly to them.
Although there is considerable evidence for the efficacy of multiple-session trauma-focused psychological interventions to treat chronic PTSD (22 – 24) , the early use of such interventions has not received the same level of scrutiny. A number of randomized controlled trials have been conducted with early interventions, but the issues of how effective they are, whom to offer intervention to, the timing of intervention, and the mode of intervention remain contentious. To help clarify the potential utility of these interventions, we performed a systematic review and meta-analysis of randomized controlled trials of psychological interventions aimed at preventing or treating PTSD within 3 months of a traumatic event.
Method
Data Sources
The electronic databases MEDLINE, ClinPSYC, PsychLit, EMBASE, PILOTS, LILACS, PSYNEBS, SocioFile, CINAHL, and the Cochrane Depression, Anxiety, and Neurosis Group Trials Register were searched until July 2007 using the Cochrane optimal randomized controlled trial search strategy combined with the following keywords: PTSD, trauma, acute stress disorder, acute posttraumatic stress disorder, acute post-traumatic stress disorder, early intervention, early psychological intervention, preventative, prevention, PTSD prevention, crisis, crisis intervention, psychological first aid, cognitive, behaviour, behavior, behavioural, behavioral, cognitive-behavioural, cognitive-behavioral, exposure, eye movement desensitization and reprocessing, psychological, psychotherapy, psychodynamic, stress inoculation, relaxation, anxiety management, psychoeducation, collaborative care, collaborative intervention, recovery, facilitating recovery, critical incident stress debriefing, debriefing, critical incident stress management, counseling, counselling, supportive counselling, and supportive counseling. Manual searches were undertaken of the Journal of Traumatic Stress and the Journal of Consulting and Clinical Psychology . Reference lists of studies identified in the search, related review articles, and management guidelines were scrutinized. Internet searches of known web sites and discussion forums were conducted, and key researchers in the field were contacted to determine whether they were aware of other relevant studies.
Study Selection
All abstracts were read independently by two of the reviewers to determine whether they potentially met the inclusion criteria. If either reviewer thought the study potentially met the criteria, the full manuscript was obtained and read independently by three of the reviewers. To be included, a study had to be a randomized controlled trial that considered one or more defined psychological interventions or treatments (excluding single-session interventions) aimed at preventing or reducing traumatic stress symptoms following events that appeared to fulfill DSM-IV criterion A1 for PTSD or acute stress disorder in comparison with a placebo control, other control (e.g., usual care or waiting list control), or alternative psychological treatment condition. All studies had to have been completed and analyzed by September 2007. Presence or absence of symptoms, sample size, language, and publication status were not used to determine whether a study should be included. The review considered studies involving adults only.
Data Extraction
A data extraction sheet was designed to record data, which were then entered into the Review Manager software package, version 4.2 (25) . Information extracted included demographic details of participants, details of the traumatic event, the randomization process, the interventions used, dropout rates, and outcome data. Quality was assessed by rating studies according to randomization, allocation concealment, blinding of assessors, and intention to treat. Each study was also rated using quality assessment criteria derived from the literature on key methodological issues pertinent to psychological intervention research on traumatic stress (26 – 29) . Data were extracted and quality assessed by two reviewers independently. Any disagreements were discussed with a third reviewer and a consensus achieved.
Data Synthesis
Given the differences between studies with respect to participants’ symptom severity and the interval between exposure to a traumatic event and commencement of the intervention, we separated the trials into three groups based on work previously conducted in this area (16) : studies that offered an intervention to any individual exposed to a traumatic event irrespective of their symptoms with the aim of preventing PTSD; studies providing interventions begun within 3 months with the aim of preventing PTSD or ongoing distress in individuals with traumatic stress symptoms; and studies providing interventions begun within 3 months with the aim of preventing PTSD or ongoing distress in individuals with acute stress disorder or acute PTSD.
In order to combine information from several studies, all interventions offered to any individual exposed to a traumatic event with the aim of preventing PTSD were considered together. The efficacy of trauma-focused cognitive-behavioral therapy (CBT) was considered in individuals with traumatic stress symptoms. Trauma-focused CBT was defined as any intervention that focused on the trauma using exposure to trauma memories and trauma reminders with or without cognitive therapy and other cognitive-behavioral techniques. The exposure-based therapy with anxiety management (30) and exposure-based therapy with hypnosis (31) arms in two studies were combined with the exposure therapy arm to generate a single mean and standard deviation. The combined results were then compared with the waiting list arm to avoid double counting.
The data were analyzed for summary effects using Review Manager. Continuous outcomes were analyzed using weighted mean differences when all trials measured outcome on the same scale. When some trials measured outcomes on different scales, standardized mean differences were used, based on the assumption that all scales measure the same underlying symptom or condition. Relative risk was calculated for categorical outcome measures, and 95% confidence intervals were computed for all outcomes.
Available case analysis and intent-to-treat analysis with imputation using the last-observation-carried-forward method were performed when enough information was available. In cases where the information presented in the paper was inadequate to perform these analyses, further information was requested from the lead author.
Heterogeneity between studies was assessed by observing the I 2 test of heterogeneity, which measures the percentage of variation that is not due to chance (32) . An I 2 of less than 30% was taken to indicate mild heterogeneity, and a fixed-effects model was used. When the I 2 was 30% or greater, a random-effects model was used. A visual inspection of the forest plots was used as a test of the robustness of these findings.
Results
Two hundred fifty titles and abstracts were identified through the search process, and 49 papers were reviewed in detail by three of the authors independently to establish whether they met the inclusion criteria. Twenty-five studies were found to meet the inclusion criteria, and another two papers (33 , 34) reported long-term follow-up on three studies (30 , 31 , 35) . Twenty-four studies were reported in English and one (36) in French. A flow diagram of the systematic review and a table summarizing the characteristics of the studies are presented in the data supplement that accompanies the online edition of this article.
Synthesis of Results
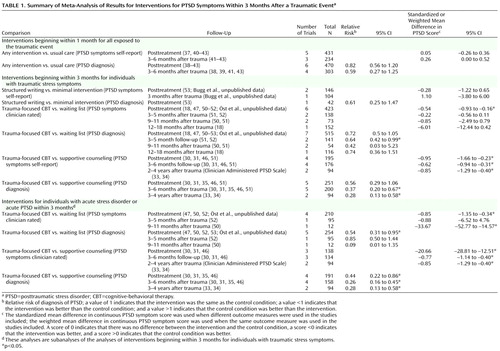
The outcomes for individual studies are indicated in Table S1 in the online data supplement. The postintervention and follow-up results of the meta-analyses for comparisons that included more than one study are listed in Table 1 , and examples of forest plots are presented in Figures 1 , 2 , and 3 . The outcomes reported are rates of PTSD and severity of PTSD (clinician rated unless unavailable, in which case self-report data are used).
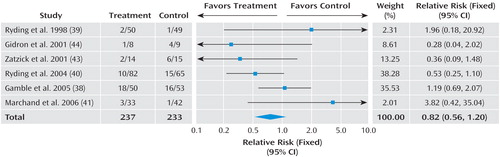
a Total events: treatment, 36; control, 43. Test for heterogeneity: χ 2 =7.97, df=5, p=0.16, I 2 =37.2%. Test for overall effect: z=1.01, p=0.31.
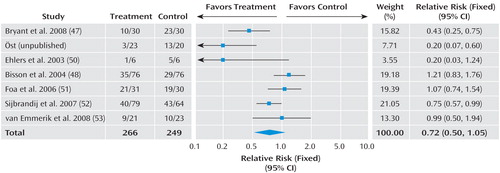
a Total events: treatment, 119; control, 142. Test for heterogeneity: χ 2 =21.01, df=6, p=0.002, I 2 =71.4%. Test for overall effect: z=1.71, p=0.09.
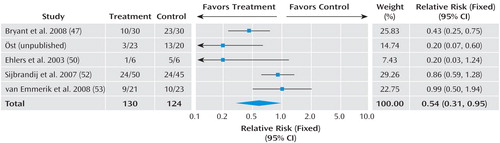
a Total events: treatment, 47; control, 76. Test for heterogeneity: χ 2 =12.11, df=4, p=0.02, I 2 =67.0%. Test for overall effect: z=2.15, p=0.03.
Studies offering intervention to individuals involved in a traumatic event irrespective of symptoms
Eight studies (36 – 42 , 43) evaluated brief psychosocial interventions aimed at preventing PTSD in individuals exposed to a specific traumatic event. All started within 1 month of the trauma. Meta-analysis of the studies with sufficient data available showed no significant differences between those who received an intervention and those who did not (see Table 1 ; see also Figure S1 in the online data supplement). The only statistically significant differences observed for specific interventions were in favor of the waiting list control group over adapted critical incident stress debriefing for self-reported PTSD symptoms immediately after the trauma (41) and for preventive counseling over monitoring or usual care for clinician-assessed PTSD symptoms 3 months after trauma (38) . Two studies (44 , 45) evaluated a two-session memory structuring intervention in individuals who had been involved in a motor vehicle accident and had a heart rate >95 bpm in the emergency department. No statistically significant differences were found between the interventions and the control conditions.
Studies offering intervention to individuals with traumatic stress symptoms within 3 months after a traumatic event
Fifteen studies (30 , 31 , 35 , 46 – 55 ; A. Bugg et al., unpublished 2007 data; L. Öst et al., unpublished 2004 data) evaluated interventions for individuals who had traumatic stress symptoms within 3 months after a traumatic event. No statistically significant differences were observed between structured writing and minimal intervention. Statistically significant differences were observed in favor of trauma-focused CBT over the waiting list condition and supportive counseling at posttreatment assessment. Follow-up data were incomplete, but statistically significant differences were present at several time points, particularly over supportive counseling.
Studies offering intervention to individuals with a diagnosis of acute stress disorder or acute PTSD within 3 months after a traumatic event
Eleven studies (30 , 31 , 35 , 46 , 47 , 49 , 50 , 52 , 53 ; Bugg et al., unpublished 2007 data; Öst et al., unpublished 2004 data) offered interventions to individuals with a diagnosis of acute stress disorder or acute PTSD. The analyses of these studies are subanalyses of the analyses of symptomatic individuals described above, with four studies excluded. Statistically significant differences were observed in favor of trauma-focused CBT over the waiting list control condition and supportive counseling. The only evidence to support any other form of treatment was for cognitive restructuring, which was significantly better than the waiting list condition but less effective than trauma-focused CBT in one study (47) .
Methodological Quality of Included Studies
Only 12 studies adequately described a method of allocation judged to make no bias possible (31 , 37 , 38 , 43 , 46 – 48 , 50 , 52 , 53 , 55 ; Bugg et al., unpublished 2007 data). Reporting of adequate concealment procedures was present in only seven studies (31 , 37 , 43 , 47 , 48 , 50 ; Bugg et al., unpublished 2007 data). Adequate blinding of the assessor of outcome measures was present in 16 studies (30 , 31 , 35 , 38 , 41 , 43 , 44 – 48 , 50 , 51 , 53 , 55) ; Bugg et al., unpublished 2007 data). Loss to follow-up was fully reported with reasons by group in 16 studies (31 , 35 , 38 , 41 , 43 , 46 – 54 ; Bugg et al., unpublished 2007 data; Öst et al., unpublished 2004 data).
The overall quality of the studies in relation to the other methodological and reporting factors considered was variable. Fewer than 10 studies fully reported whether training was offered to assessors and how performance, supervision, or reliability checks of assessors were performed (four studies), whether treatment fidelity was independently checked and adequate (five studies), whether power calculation was reported (four studies), whether follow-up extended beyond 6 months (nine studies), and whether there were any side effects (one study).
In order to determine the impact of quality on outcome, the three studies included in the analysis of trauma-focused CBT versus waiting list for individuals with traumatic stress symptoms (47 , 48 , 50) that achieved the highest quality ratings for the four Cochrane quality criteria were included in a sensitivity analysis. This resulted in a reduction in the magnitude of intervention effect, with superiority over waiting list control only approaching statistical significance (three studies, N=224, standardized mean difference –0.75, 95% CI=–1.53 to 0.02).
Discussion
Main Findings
There was no evidence that a multiple-session intervention aimed at everyone, irrespective of their symptoms, following a traumatic event was effective. Trauma-focused CBT was significantly better than waiting list or usual care at reducing traumatic stress symptoms in individuals who were symptomatic at entry into the study, but the magnitude of effect varied. The magnitude was largest for individuals who were diagnosed with acute stress disorder or acute PTSD. Evidence of the benefits of trauma-focused CBT for symptomatic individuals who did not meet full diagnostic criteria for these conditions was weak.
Heterogeneity
There was evidence of both clinical and statistical heterogeneity in the included studies.
Although all the trials attempted to reduce traumatic stress symptoms, the nature of the interventions was quite diverse. This was partially dealt with by separating interventions into predetermined groups, although we decided to combine the interventions provided to individuals irrespective of their symptoms in order to maximize the information available. There were more studies evaluating trauma-focused CBT than other interventions, but the specific interventions in the trauma-focused CBT group were not identical. All were trauma focused, but some interventions primarily used a prolonged exposure paradigm (e.g., reference 48 ), whereas others (e.g., reference 50 ) primarily used cognitive techniques with more limited exposure. It was not possible to conduct a formal analysis comparing studies with varying amounts of exposure because of limited detail regarding the specific amount of exposure delivered. However, there did not appear to be a direct relationship between more exposure and improved outcome or vice versa among interventions included in the trauma-focused CBT group. This seems at odds with the Institute of Medicine’s recent conclusion that exposure therapy is the only type of psychological treatment with sufficient evidence of efficacy in the treatment of PTSD (56) , although exposure therapy was superior to cognitive restructuring with no exposure in the single study included in this review that directly compared these two interventions (47) .
In addition, the total number of hours of intervention provided varied from around 4 hours to around 16 hours. There were also differences in the clinical populations, especially with regard to the severity of symptoms at entry to the studies. On the basis of previous work on this topic (16) , we grouped trials in a clinically meaningful manner according to the intervention and the clinical populations included, but this approach is not empirically based, which should be considered when interpreting the results. We concluded that the trials grouped together were essentially trying to measure the same thing and that it was worthwhile summarizing their combined results, but the variation means that caution should be applied when interpreting the results (32) .
Methodological Quality
The overall quality of the studies was varied. Using the Cochrane quality criteria, 16 (64%) studies fully reported loss to follow-up with reasons, 15 (60%) described using appropriately blinded assessors to measure outcome, 12 (48%) described appropriate randomization with no bias possible, and only seven (28%) reported adequate allocation concealment. The small sample sizes of most of the studies are also an important limitation. However, the intervention and control groups appeared well matched at baseline in most studies, reducing the risk of the reported unadjusted mean outcomes being influenced by baseline differences.
Several studies, including those that provided more positive results, had strong methodological characteristics. A meta-analysis of the highest-quality studies resulted in a larger effect size (0.75) for the efficacy of trauma-focused CBT versus waiting list control than the meta-analysis of all studies irrespective of quality (0.54), but the former meta-analysis just failed to reach statistical significance. This is probably a power issue and, contrary to previous research (57) , does not suggest that poorer-quality studies falsely elevated the apparent efficacy of the intervention.
The choice of control condition is particularly important in early intervention research, where a reduction in symptoms over the duration of the trial would be expected given the natural course of traumatic stress reactions (58) . The development of a psychological treatment placebo is very difficult, if not impossible, as is blinding of participants and therapists. Some of the waiting list and usual care groups may have received some form of intervention by virtue of contact through symptom monitoring, but this was not properly evaluated, and it is not possible to determine what impact this might have had on outcomes.
Only one study (47) reported adverse effects, and it is unclear whether any occurred in other studies. The dropout rates were mostly no higher in the intervention groups than in the control groups across the studies reviewed, which suggests that the interventions did not cause major adverse effects. However, the absence of tolerability assessment is a key shortcoming in the trials identified and one that has previously been noted in psychological treatment studies of chronic PTSD (22) .
Implications for Practice
The results suggest that no psychological intervention can be recommended for routine use following traumatic events. This is consistent with the results of single-session interventions, although, in contrast to them (14) , with the possible exception of adapted critical incident stress debriefing, no evidence was found of any harm occurring as a result of an intervention. Trauma-focused CBT was the only early intervention with convincing evidence of efficacy in reducing and preventing traumatic stress symptoms, but only for symptomatic individuals and particularly for those who met the diagnostic criteria for acute stress disorder or acute PTSD. The less convincing evidence in favor of trauma-focused CBT for all symptomatic individuals raises some interesting clinical implications. Positive outcomes in the meta-analysis for all symptomatic individuals appear to have been bolstered by the outcomes from studies focusing specifically on individuals meeting all diagnostic criteria for acute stress disorder and acute PTSD. This suggests that the presence of a specific diagnosis may be the most important predictor of who will benefit from trauma-focused CBT. However, when planning how best to detect such individuals, it is important to heed the research suggesting that merely screening for acute stress disorder is problematic as it misses many individuals who go on to develop PTSD (59) .
While the majority of symptomatic individuals are likely to gain some benefit from trauma-focused CBT 1 to 3 months after a traumatic event, the magnitude of this benefit may not be very large. Whether the magnitude of improvement is likely to be significant enough to justify the routine provision of trauma-focused CBT to all symptomatic individuals is open to debate. The evidence suggests that trauma-focused CBT should be offered to all who suffer from acute stress disorder or acute PTSD and that limiting it to this group can be justified, particularly when resources are limited. The results for non-trauma-focused CBT interventions were disappointing, but it remains possible that elements from them are effective, particularly if used with more symptomatic individuals. For example, behavioral reactivation (54) has clearly not yet been evaluated with an adequately powered trial and would benefit from further evaluation.
The results of this review support calls that have been made for a stepped or stratified care system whereby those with the most severe symptoms are offered more complex interventions (18) . The fact that trauma-focused CBT appears to be an effective treatment suggests that more work should be done to determine whether it could be delivered as part of a screening program after major traumatic events.
Implications for Research
Further well-designed randomized controlled trials of trauma-focused CBT starting within the first 3 months after traumatic events with longer follow-up periods are needed. Given the modest overall effects of trauma-focused CBT, the development and trialing of other psychological treatments are important. The finding that exposure therapy was superior to cognitive restructuring in one study requires replication, and the comparison of treatments with more or less exposure should be pursued in the future.
Most of the studies included in this review attempted to evaluate individual psychological therapy. Given the important role of social support as a predictor of outcome (60 , 61) , it would be of interest to examine interventions aimed at couples and families to improve familial response. It would also be of interest to evaluate forms of community intervention and interventions aimed at improving coping skills and enhancing positive and helpful behaviors (J.I. Ruzek, unpublished 2007 paper). Future research should also consider adverse events and tolerability of treatment, carefully control for additional intervention, and explore the optimal time to intervention, how long treatment should last, and whether other techniques can be incorporated into existing treatments to improve their efficacy.
1. Goenjian A: A mental health relief programme in Armenia after the 1988 earthquake: implementation and clinical observations. Br J Psychiatry 1993; 163:230–239Google Scholar
2. Green BL, Grace MC, Lindy JD, Gleser GC, Leonard AC, Crummier TL: Buffalo Creek survivors in the second decade: comparison with unexposed and nonlitigant groups. J Appl Soc Psychol 1990; 20:1033–1050Google Scholar
3. Kulka RA, Schlenger WE, Fairbank JA, Jordan BK, Hough RL, Marmar CR, Weiss DS: Trauma and the Vietnam War Generation: Report of Findings From the Vietnam Veterans Study. New York, Bruner/Mazel, 1990Google Scholar
4. Kilpatrick DG, Saunders BE, Veronen LJ, Best CL, Von JM: Criminal victimization: lifetime prevalence reporting to police, and psychological impact. Crime Delinq 1987; 33:479–489Google Scholar
5. North CS, Smith EM, Spitznagel EL: Postraumatic stress disorder in survivors of a mass shooting. Am J Psychiatry 1994; 151:82–88Google Scholar
6. Ehlers A, Mayou RA, Bryant B: Psychological predictors of chronic posttraumatic stress disorder after motor vehicle accidents. J Abnorm Psychol 1998; 107:508–519Google Scholar
7. Bonanno GA: Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol 2004; 59:20–28Google Scholar
8. McNally RJ, Bryant RA, Ehlers A: Does early psychological intervention promote recovery from posttraumatic stress disorder? Psychological Science in the Public Interest 2003; 4:45–79Google Scholar
9. Harvey AG, Bryant RA: The relationship between acute stress disorder and posttraumatic stress disorder: a prospective evaluation of motor vehicle accident survivors. J Consult Clin Psychol 1998; 66:507–512Google Scholar
10. Brewin CR, Andrews B, Rose S, Kirk M: Acute stress disorder and posttraumatic stress disorder in victims of violent crime. Am J Psychiatry 1999; 156:360–366Google Scholar
11. Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W: A prospective examination of post-traumatic stress disorder in rape victims. J Trauma Stress 1992; 5:455–475Google Scholar
12. Kessler R, Sonnega A, Bromet E, Hughes M, Nelson CB: Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995; 52:1048–1060Google Scholar
13. Litz BT, Gray MJ: Early intervention for trauma in adults: a framework for first aid and secondary prevention, in Early Intervention for Trauma and Traumatic Loss. Edited by Litz BT. New York, Guilford, 2004Google Scholar
14. Rose S, Bisson J, Churchill R, Wessely S: Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database Syst Rev 2005; issue 3Google Scholar
15. van Emmerik AA, Kamphuis JH, Hulsbosch AM, Emmelkamp PM: Single session debriefing after psychological trauma: a meta-analysis. Lancet 2002; 360:766–771Google Scholar
16. National Collaborating Centre for Mental Health: Post-Traumatic Stress Disorder: The Management of PTSD in Adults and Children in Primary and Secondary Care. London, Gaskell, 2005Google Scholar
17. Australian Centre for Posttraumatic Mental Health: Australian Guidelines for the Treatment of Adults With Acute Stress Disorder and Posttraumatic Stress Disorder. Melbourne, 2007Google Scholar
18. Bisson JI, Roberts N, Macho G: Service innovations: the Cardiff Traumatic Stress Initiative: an evidence-based approach to early psychological intervention following traumatic events. Psychiatr Bull 2003; 27:145–147Google Scholar
19. Ehlers A, Clark DM: Early psychological interventions for adult survivors of trauma: a review. Biol Psychiatry 2003; 53:817–826Google Scholar
20. Litz B, Gray M, Bryant R, Adler A: Early intervention for trauma: current status and future directions. Clin Psychol 2002; 9:112–134Google Scholar
21. Gray MJ, Litz BT: Behavioral interventions for recent trauma. Behav Modif 2005; 29:189–215Google Scholar
22. Bisson JI, Ehlers A, Matthews R, Pilling S, Richards D, Turner S: Psychological treatments for chronic post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry 2007; 190:97–104Google Scholar
23. Bradley R, Greene J, Russ E, Dutra L, Westen D: A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry 2005; 162:214–227Google Scholar
24. Bisson J, Andrew M: Psychological treatment of post-traumatic stress disorder. Cochrane Database Syst Rev 2007; 3:CD003388Google Scholar
25. Cochrane Collaboration: Review Manager (RevMan) version 4.2 for Windows. Oxford, Cochrane Collaboration, 2003Google Scholar
26. Moncrieff J, Churchill R, Drummond C: Development of a quality assessment for trials of treatment for depression and neurosis. Int J Methods Psychiatr Res 2001; 10:126–133Google Scholar
27. Foa EB, Meadows EA: Psychosocial treatments for posttraumatic stress disorder: a critical review. Annu Rev Psychol 1997; 48:449–480Google Scholar
28. Hertlein KM, Ricci RJ: A systematic research synthesis of EMDR studies: implementation of the platinum standard. Trauma Violence Abuse 2004; 5:285–300Google Scholar
29. Kenardy J, Carr V: Imbalance in the debriefing debate: what we don’t know outweighs what we do. Bulletin of the Australian Psychological Society 1996; 17:4–6Google Scholar
30. Bryant RA, Sackville T, Dang ST, Moulds M, Guthrie R: Treating acute stress disorder: an evaluation of cognitive behavior therapy and supportive counseling techniques. Am J Psychiatry 1999; 156:1780–1786Google Scholar
31. Bryant RA, Moulds ML, Guthrie RM, Nixon RDV: The additive benefits of hypnosis and cognitive-behavioral therapy in treating acute stress disorder. J Consult Clin Psychol 2005; 73:334–340Google Scholar
32. Fletcher J: What is heterogeneity and is it important? Br Med J 2007; 334:94–96Google Scholar
33. Bryant RA, Moulds ML, Nixon RVD: Cognitive behaviour therapy of acute stress disorder: a four-year follow-up. Behav Res Ther 2003; 41:489–494Google Scholar
34. Bryant RA, Moulds ML, Nixon RDV, Mastrodomenico J, Felmingham K, Hopwood S: Hypnotherapy and cognitive behaviour therapy of acute stress disorder: a 3-year follow-up. Behav Res Ther 2006; 44:1331–1335Google Scholar
35. Bryant RA, Harvey AG, Dang ST, Sackville T, Basten C: Treatment of acute stress disorder: a comparison of cognitive-behavioral therapy and supportive counseling. J Consult Clin Psychol 1998; 66:862–866Google Scholar
36. André C, Lelord F, Légeron P, Reignier A, Delattre A: [Effectiveness of early intervention on 132 bus drivers victims of aggressions: a controlled trial]. L’Encephale 1997; 23:65–71 (French)Google Scholar
37. Kazak AE, Simms S, Alderfer MA, Rourke MT, Crump T, McClure K, Jones P, Rodriguez A, Boeving A, Hwang W, Reilly A: Feasibility and preliminary outcomes from a pilot study of a brief psychological intervention for families of children newly diagnosed with cancer. J Pediatr Psychol 2005; 30:644–655Google Scholar
38. Gamble J, Creedy D, Moyle W, Webster J, McAllister M, Dickson P: Effectiveness of a counseling intervention after a traumatic childbirth: a randomized controlled trial. Birth 2005; 32:11–19Google Scholar
39. Ryding E, Wijma K, Wijma B: Postpartum counselling after an emergency caesarean. Clin Psychol Psychother 1998; 5:231–237Google Scholar
40. Ryding El, Wiren E, Johansson G, Ceder B, Dahlstrom A: Group counseling for mothers after emergency cesarean section: a randomized controlled trial of intervention. Birth 2004; 31:247–253Google Scholar
41. Marchand A, Guay S, Boyer R, Iucci S, Martin A, St-Hilaire M: A randomized controlled trial of an adapted form of individual critical incident stress debriefing for victims of an armed robbery. Brief Treat Crisis Interv 2006; 6:122–129Google Scholar
42. Brom D, Kleber RJ, Hofman MC: Victims of traffic accidents: incidence and prevention of post-traumatic stress disorder. J Clin Psychol 1993; 49:131–140Google Scholar
43. Zatzick D, Roy-Byrne P, Russo JE, Rivara FP, Koike A, Jurkovich GJ, Katon W: Collaborative interventions for physically injured trauma survivors: a pilot randomized effectiveness trial. Gen Hosp Psychiatry 2001; 23:114–123Google Scholar
44. Gidron Y, Gal R, Freedman S, Twiser I, Lauden A, Snir Y, Benjamin J: Translating research findings to PTSD prevention: results of a randomized-controlled pilot study. J Trauma Stress 2001; 14:773–780Google Scholar
45. Gidron Y, Gal R, Givati G, Lauden A, Snir Y, Binjamin J: Interactive effects of memory structuring and gender in preventing posttraumatic stress symptoms. J Nerv Ment Dis 2007; 195:1–4Google Scholar
46. Bryant RA, Moulds M, Guthrie R, Nixon RDV: Treating acute stress disorder following mild traumatic brain injury (letter). Am J Psychiatry 2003; 160:585–587Google Scholar
47. Bryant RA, Mastrodomenico J, Felmingham KL, Hopwood S, Kenny L, Kandris E, Cahill C, Creamer M: Treatment of acute stress disorder: a randomized controlled trial. Arch Gen Psychiatry 2008; 65:659–667Google Scholar
48. Bisson JI, Shepherd JP, Joy D, Probert R, Newcombe RG: Early cognitive-behavioural therapy for post-traumatic stress symptoms after physical injury. Br J Psychiatry 2004; 184:63–69Google Scholar
49. Echeburua E, de Corral P, Sarasua B, Zubizarreta I: Treatment of acute posttraumatic stress disorder in rape victims: an experimental study. J Anxiety Disord 1996; 10:185–199Google Scholar
50. Ehlers A, Clark D, Hackmann A, McManus F, Fennell M, Herbert C, Mayou R: A randomized controlled trial of cognitive therapy, a self-help booklet, and repeated assessments as early interventions for posttraumatic stress disorder. Arch Gen Psychiatry 2003; 60:1024–1032Google Scholar
51. Foa EB, Zoellner LA, Feeny NC: An evaluation of three brief programs for facilitating recovery after assault. J Trauma Stress 2006; 19:29–43Google Scholar
52. Sijbrandij M, Olff M, Reitsma JB, Carlier IVE, de Vries MH, Gersons BPR: Treatment of acute posttraumatic stress disorder with brief cognitive behavioral therapy: a randomized controlled trial. Am J Psychiatry 2007; 164:82–90Google Scholar
53. van Emmerik AA, Kamphuis JH, Emmelkamp PM: Treating acute stress disorder and posttraumatic stress disorder with cognitive behavioral therapy or structured writing therapy: a randomized controlled trial. Psychother Psychosom 2008; 77:93–100Google Scholar
54. Wagner AW, Zatzick DF, Ghesquiere A, Jurkovich GJ: Behavioral activation as an early intervention for posttraumatic stress disorder and depression among physically injured trauma survivors. Cogn Behav Pract 2007; 4:341–349Google Scholar
55. Zatzick D, Roy-Byrne P, Russo J, Rivara F, Droesch R, Wagner A, Dunn C, Jurkovich G, Uehara E, Katon W: A randomized effectiveness trial of stepped collaborative care for acutely injured trauma survivors. Arch Gen Psychiatry 2004; 61:498–506Google Scholar
56. Committee on Treatment of Posttraumatic Stress Disorder, Institute of Medicine of the National Academies: Treatment of Posttraumatic Stress Disorder: An Assessment of the Evidence. Washington, DC, National Academies Press, 2008Google Scholar
57. Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, Tugwell P, Klassen TP: Does quality of reports of randomised trials affect estimates of intervention efficacy in meta-analyses? Lancet 1998; 352:609–613Google Scholar
58. Galea S, Vlahov D, Resnick H, Ahern J, Susser E, Gold J, Bucuvalas M, Kilpatrick D: Trends of probable post-traumatic stress disorder in New York City after the September 11 terrorist attacks. Am J Epidemiol 2003; 158:514–524Google Scholar
59. Bryant R: Acute stress disorder. Psychiatry 2006; 5:238–239Google Scholar
60. Brewin CR, Andrew B, Valentine JD: Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 2000; 68:748–766Google Scholar
61. Ozer EJ, Best SR, Lipsey TL, Weiss DS: Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull 2003; 129:52–73Google Scholar