In This Issue
What Is the Right Dose?
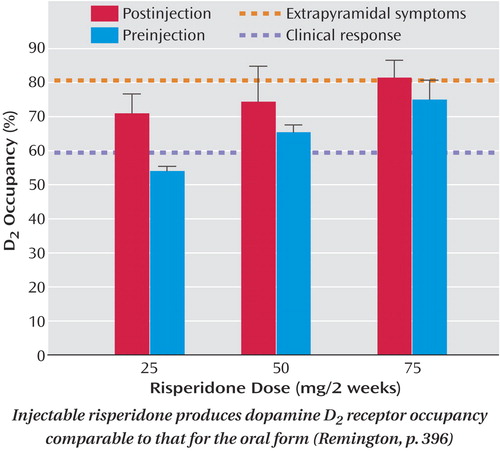
Risperidone is the first of the newer, or “atypical,” antipsychotics to become available in a long-acting injectable form. Remington et al. p. 396) used positron emission tomography (PET) to measure the drug’s binding to dopamine D2 receptors in the brain. All three doses tested-25, 50, and 75 mg every 2 weeks-produced the degree of D2 receptor occupancy considered necessary for clinical response (see figure below). The 75-mg dose slightly exceeded the threshold associated with extrapyramidal side effects. These occupancy levels are comparable to those for standard doses of oral risperidone. This article and the one by Spencer et al. p. 387) on short-acting versus long-acting methylphenidate are striking examples of the use of PET to determine optimal therapeutic doses of psychotropic medication for clinical use.
Cognitive Behavior Therapy for Schizophrenia
Adding cognitive behavior therapy to pharmacologic treatment of schizophrenia may improve relapse prevention, positive symptoms, and adherence to drug regimens. Although not definitive, the evidence is compelling enough that cognitive behavior therapy is widely accepted as an adjunctive treatment for schizophrenia in the United Kingdom. Turkington et al. p. 365) stress that medication is the mainstay of schizophrenia treatment but describe benefits of cognitive behavior therapy for some patients who have residual symptoms, deny their illness, or are demoralized by emphasis on the schizophrenia diagnosis. American-based guidelines also recommend cognitive behavior therapy for patients with treatment-resistant schizophrenia. An editorial by Keith p. 362) gives a historical perspective on psychotherapies in the treatment of schizophrenia.
Computer Game for Cognitive Testing
Sorkin et al. p. 512) created an enjoyable computer game that tests sensory integration and working memory, i.e., short-term retention and use of information, in persons with schizophrenia. Wearing 3-D glasses, patients navigate through a virtual maze (see figure above), choosing doors according to a rule that changes after 4–6 correct choices. Performance on the test is able to achieve the same 85% accuracy rate in distinguishing schizophrenia patients from healthy comparison subjects. The validity of this method was further verified by correlations between several of the measurements and standard diagnostic ratings of schizophrenia. Although the results are exploratory, they suggest a new use of technology to help evaluate patients' mental strengths and weaknesses.
Autoimmune Diseases and Schizophrenia
Links between schizophrenia and autoimmune disorders, such as celiac disease, Sjogren’s syndrome, and type 1 diabetes, have been tantalizing but inconsistent. Population-based evidence now comes from Eaton et al. p. 521), who paired a Danish schizophrenia register with hospitalizations for 29 autoimmune diseases. The 7,704 schizophrenia patients admitted to psychiatric facilities between 1981 and 1998 had a nearly 50% higher prevalence of one or more autoimmune disorders than did matched comparison subjects. Five diseases were more prevalent in both the schizophrenia patients and their parents: thyrotoxicosis, intestinal malabsorption, acquired hemolytic anemia, interstitial cystitis, and Sjogren’s syndrome. These epidemiological findings confirm several previously reported associations between schizophrenia and autoimmune disorders and may eventually steer research to common etiologic pathways.