Natural Recovery and Treatment-Seeking in Pathological Gambling: Results of Two U.S. National Surveys
Abstract
OBJECTIVE: Pathological gambling is described in DSM-IV as a chronic and persisting disorder, but recent community-based longitudinal studies that have highlighted the transitory nature of gambling-related problems have called into question whether this is an accurate characterization. This emerging evidence of high rates of recovery coupled with low rates of treatment-seeking for pathological gambling suggests that natural recovery might be common. The purpose of the present study was to document the rates of recovery, treatment-seeking, and natural recovery among individuals with DSM-IV pathological gambling disorder in two large and representative U.S. national surveys. METHOD: Prevalences of recovery, treatment-seeking, and natural recovery were estimated among individuals from the Gambling Impact and Behavior Study (N=2,417) and the National Epidemiologic Survey on Alcohol and Related Conditions (N=43,093) who reported a lifetime history of DSM-IV pathological gambling disorder (N=21 and N=185, respectively). RESULTS: Among individuals with a lifetime history of DSM-IV pathological gambling, 36%–39% did not experience any gambling-related problems in the past year, even though only 7%–12% had ever sought either formal treatment or attended meetings of Gamblers Anonymous. About one-third of the individuals with pathological gambling disorder in these two nationally representative U.S. samples were characterized by natural recovery. CONCLUSIONS: Pathological gambling may not always follow a chronic and persisting course. A substantial portion of individuals with a history of pathological gambling eventually recover, most without formal treatment. The results of large epidemiological surveys of pathological gambling may eventually overturn the established wisdom about pathological gambling disorder.
Pathological gambling is described in DSM-IV as a chronic and persisting disorder, but recent community-based longitudinal studies that have highlighted the transitory nature of gambling-related problems have called into question whether this is an accurate characterization (1–3). For example, among 35 participants recruited from a New Zealand general population survey with a current diagnosis of problem or pathological gambling, 63% were no longer experiencing the same level of problems at a 7-year follow-up (2). Additional evidence consistent with the results of the longitudinal studies comes from the observation that 39% of the participants in regional North American cross-sectional prevalence surveys with a lifetime diagnosis of problem or pathological gambling did not have a past-year diagnosis (4), suggesting that a substantial fraction of individuals with a history of problem or pathological gambling have recovered from their problems.
However, previous studies have focused on whether individuals with a history of problem or pathological gambling have experienced a reduction in symptoms to below a diagnostic threshold, rather than the complete abatement of symptoms that is generally implied by the concept of recovery. Although there is evidence to suggest that a reduction in symptoms is common among individuals with a history of problem and pathological gambling, the extent to which individuals with clinically significant pathological gambling disorder have a complete abatement of gambling-related problems is unknown. In the Epidemiologic Catchment Area (ECA) study (5), such recovery rates for other psychiatric disorders were relatively high for substance use disorders (54%–59%), intermediate for major depression (42%), and lowest for manic episodes (28%) and somatization disorder (8%).
One of the other major findings from the ECA Study was the surprisingly low rate of treatment-seeking for some psychiatric disorders; for example, the rate of treatment-seeking among individuals with a past-year substance use disorder was relatively low (24%) compared to major depression (54%), bipolar disorder (61%), and somatization disorder (70%) (6). These two sets of findings from the ECA study suggest that there may be an inverse relationship between the probability of recovery from, and of seeking treatment for, a psychiatric disorder. This appears somewhat counterintuitive but can be explained by the phenomenon of natural recovery. In other words, for some disorders, such as substance use disorders, many of those who recover are able to do so without any formal treatment. The emerging evidence of high rates of recovery coupled with low rates of treatment-seeking (e.g., 2.6% among callers to a gambling help line [7]) suggests that natural recovery might be relatively common for pathological gambling disorder as well.
The purpose of the present study was to document the rates of recovery, treatment-seeking, and natural recovery among individuals with DSM-IV pathological gambling disorder in two large and representative U.S. national surveys.
Method
Participants
To establish the replicability of the results, data were drawn from two recent U.S. national surveys (now in the public domain): the Gambling Impact and Behavior Study (8) (GIBS) and the National Epidemiologic Survey on Alcohol and Related Conditions (9) (NESARC). Both studies obtained lifetime and past-year DSM-IV diagnoses of, and treatment-seeking for, pathological gambling. The GIBS, conducted in 1998–1999, included a telephone interview of 2,417 adults identified by using random-digit dialing techniques and obtained an overall survey response rate of 56%. The NESARC, conducted in 2001–2002, was an in-person interview of 43,093 adults identified by using Census-based sampling techniques and obtained an overall survey response rate of 81%. Further details of the GIBS and the NESARC can be found in a number of published studies (e.g., references 10–15) and online (16–17).
Measures
In addition to differences in sampling and interviewing methods, the two surveys also used different instruments to assess DSM-IV pathological gambling. The GIBS used the National Opinion Research Center (NORC) DSM-IV Screen for Gambling Problems (NODS) (18) and the NESARC used the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV) (19). The assessments of lifetime and past-year pathological gambling from the two interviews did not markedly differ. Two modifications were made to the DSM-IV pathological gambling diagnosis from the NESARC public domain data set. A lifetime AUDADIS-IV diagnosis of pathological gambling requires that the respondent meet at least five of 10 DSM-IV criteria in the 12 months preceding the interview and/or before that period (12). In the present study, a lifetime pathological gambling diagnosis required that the respondents meet at least five of 10 DSM-IV criteria at any time in their lives. This minor change was made to make the assessments from the GIBS and the NESARC more comparable. In the AUDADIS-IV diagnosis of pathological gambling, “chasing” wins was also counted toward the DSM-IV criterion A6 (“after losing money gambling, often returns another day to get even [‘chasing’ one’s losses]”). Chasing wins was not included as a criterion of pathological gambling in the present study. This minor change was made to make the assessments from the GIBS and the NESARC more comparable and to more closely conform to the DSM-IV definition of pathological gambling.
Another difference between the pathological gambling assessments in the GIBS and the NESARC surveys was the nature of gambling involvement that was required to enter the diagnostic section for pathological gambling. The NODS diagnostic assessment in the GIBS was only administered to those who reported ever losing more than $100 in a single day or across a single year, whereas the AUDADIS-IV diagnostic assessment in the NESARC was administered to anyone who reported that they had ever gambled at least five times in any 1 year.
In the GIBS interview, a thorough assessment of gambling was conducted, including an assessment of involvement in 11 types of gambling (pull tabs or a lottery, casino gambling, Indian or tribal gambling, noncasino electronic gambling machines, card games, betting on private games, sports betting, on- and off-track betting, bingo, Internet gambling, and charitable gambling) in the past year. Therefore, in the GIBS study, it was possible to ascertain whether or not recovery from pathological gambling was accompanied by abstention from gambling. A similar assessment of past-year gambling involvement was not conducted in the NESARC.
There were several novel features of the NESARC interview that were not present in the GIBS interview. When a lifetime symptom of pathological gambling was endorsed, whether the symptom occurred in the past 12 months and prior to the past 12 months was determined and when at least five pathological gambling symptoms occurred prior to the past 12 months, a series of follow-up questions were asked. The purpose of the follow-up questions was to ascertain the following: 1) whether some of the symptoms were clustered together within the same 12-month period; 2) how many separate clustered periods of pathological gambling there were (periods in which several pathological gambling symptoms co-occurred that were separated from each other in time by at least 1 symptom-free year); 3) the duration of the longest period of clustered pathological gambling; and 4) among participants who had experienced clustered periods of pathological gambling but did not endorse any past-year pathological gambling symptoms, the age that marked the beginning of the current symptom-free period. The internal consistency reliabilities of the 10 diagnostic criteria for assessing lifetime DSM-IV pathological gambling with the NODS (in the GIBS) and the AUDADIS-IV (in the NESARC) were 0.75 and 0.80, respectively. The test-retest reliability of the DSM-IV pathological gambling symptom scores over a 2–4-week retest interval with the NODS was 0.99 (18) and over a 3–20-week retest interval with the AUDADIS-IV was 0.76 (19). In addition, satisfactory reliability and validity have previously been established for a similar measure of pathological gambling based on the DSM-IV criteria (20).
In the GIBS, any participant who endorsed symptoms of pathological gambling was asked, “Have you ever received any kind of help or treatment for gambling problems? Include self-help groups and help from professionals such as doctors or counselors.” Positive responses to this question were followed by queries about seven different forms of treatment, including attending a Gamblers Anonymous meeting. In the NESARC, participants who endorsed at least five symptoms of pathological gambling were asked, “Did you ever go to any kind of counselor, therapist, doctor, psychologist, or any other person like that for help with your gambling?” and were also asked in a separate question whether they had ever gone to Gamblers Anonymous.
Data Analysis
The main outcomes of interest were treatment-seeking, recovery, and natural recovery among individuals with a history of DSM-IV pathological gambling. For the purposes of this study, the prevalence of treatment-seeking was estimated as the percentage of individuals with a lifetime history of DSM-IV pathological gambling who had ever sought help from a professional or attended Gamblers Anonymous. The prevalence of recovery was estimated as the percentage of individuals with a lifetime history of DSM-IV pathological gambling who did not endorse any pathological gambling symptoms in the past 12 months. Natural recovery was estimated as the percentage of individuals with a lifetime history of DSM-IV pathological gambling who experienced recovery and had never sought treatment.
As mentioned previously, estimating the prevalence of recovery from pathological gambling from the proportion of past-year to lifetime cases is probably an overestimate of the rate of recovery because many individuals who do not surpass the past-year diagnostic threshold may still be symptomatic. Another problem with this method arises from the fundamental difference between lifetime and past-year diagnoses (4, 21–22). As typically operationalized in cross-sectional surveys, a lifetime diagnosis of pathological gambling merely requires that a certain number of symptoms (for instance, five for DSM-IV pathological gambling) are ever experienced but not necessarily at the same time. A past-year diagnosis, on the other hand, typically requires that a certain number of symptoms are experienced within the same 12-month period. An individual with a lifetime diagnosis of DSM-IV pathological gambling may never have had five symptoms within a single year, whereas an individual with a past-year diagnosis would. In other words, an individual with a lifetime diagnosis of pathological gambling who has not had at least five symptoms in the past year is not necessarily experiencing a reduced number of pathological gambling symptoms. Again, this may lead to an overestimate of the prevalence of recovery. Yet another problem with estimating the prevalence of recovery from pathological gambling from the proportion of past-year to lifetime cases is that individuals who have been diagnosed with pathological gambling only in the past year (who qualify for both a lifetime and a past-year pathological gambling diagnosis) are inappropriately counted as “nonrecovered” cases. These new-onset cases should be omitted from consideration because they are not informative about recovery. Including such individuals will actually underestimate the prevalence of recovery.
These limitations were circumvented by defining recovery as an absence of pathological gambling symptoms within the past year and by capitalizing on a novel feature of the NESARC study. In the NESARC, the rates of recovery were also estimated among the individuals who endorsed five or more DSM-IV pathological gambling symptoms occurring prior to the past 12 months and who also reported that some of their symptoms had clustered together within the same 12-month period.
All of the analyses were based on weighted data. The sampling weights adjusted the samples so that they were demographically matched to the U.S. Census and to account for unequal participation rates of certain demographic groups. Because the percentages presented in this article are based upon weighted data, they will not match the percentages calculated from the unweighted numbers provided.
Results
Gambling Impact and Behavior Study
Of the 2,417 participants in the GIBS, 21 (0.80%) (10 women, 44.6%) had a lifetime history of DSM-IV pathological gambling. Of the 21 individuals with a lifetime history of DSM-IV pathological gambling, 18 (84.8%) did not meet the diagnostic criteria for DSM-IV pathological gambling, and nine (38.9%) had zero pathological gambling symptoms within the past 12 months (in other words, 50% of those who did not meet the diagnostic criteria for past-year pathological gambling had at least one pathological gambling symptom). Of the nine individuals with a history of DSM-IV pathological gambling who had zero pathological gambling symptoms in the past 12 months, three (30.8%) reported that they had participated in some form of gambling in the past year.
Only two (7.1%) of the 21 individuals with a history of pathological gambling reported having sought any type of treatment for their gambling problems, and of the nine individuals with a history of DSM-IV pathological gambling who had zero pathological gambling symptoms in the past 12 months, only one had sought treatment for gambling problems.
National Epidemiologic Survey on Alcohol and Related Conditions
Of the 43,093 participants in the NESARC, 185 (0.40%) (71 women, 29.6%) had a lifetime history of DSM-IV pathological gambling. Of the 185 individuals with a lifetime history of DSM-IV pathological gambling, 111 (63.0%) did not meet the diagnostic criteria for DSM-IV pathological gambling, and 70 (36.0%) had zero pathological gambling symptoms within the past 12 months (in other words, 37% of those who did not meet the diagnostic criteria for past-year pathological gambling had at least one pathological gambling symptom).
Only 22 (9.9%) (10 women, 47.1%) of those with a history of pathological gambling either had received professional treatment for their gambling problems (N=12, 5.5%) or had attended at least one Gamblers Anonymous meeting (N=16, 7.3%). There was a strong association (r=0.85, p=0.03) between the number of lifetime pathological gambling symptoms experienced and the probability of seeking treatment; 6% of those who endorsed five symptoms sought treatment compared to 4%, 6%, 17%, 31%, and 76% of those with six, seven, eight, nine, and 10 symptoms, respectively. Of the 70 individuals with a history of DSM-IV pathological gambling who had zero pathological gambling symptoms in the past 12 months, only eight had sought treatment for their gambling problems.
Similar rates of recovery were obtained when a more rigorous test was conducted. Instead of examining the absence of symptoms among individuals who met the standard “lifetime unclustered” pathological gambling diagnostic criteria, the focus was shifted to the subset of individuals who had a history of “prior to past year clustered” DSM-IV pathological gambling. Of the 185 participants with a lifetime history of DSM-IV pathological gambling, 159 (86.0%) had five or more symptoms occurring prior to the past 12 months, and of these, 141 (90.2%) reported that some of these symptoms had occurred together within the same 12-month period. Thus, 78.0% (141 of 185) of those with the standard “lifetime unclustered” pathological gambling diagnosis qualified for the narrower “prior to past year clustered” pathological gambling diagnosis. Sixty-two percent (76 of 122; the number of episodes was unknown for 19 individuals) of these participants reported that they had experienced only one episode of pathological gambling in their lifetime, 11% (16 of 122) had two episodes, and 27% (30 of 122) had three or more episodes (mean number of episodes=2.8, range=1–32). Eighty percent (107 of 131; the duration of the longest episode was unknown for 10 individuals) reported that the duration of their longest episode of pathological gambling was 1 year or less, 12% (16 of 131) reported that their longest episode of pathological gambling lasted 1.5 to 5 years, and 8% (eight of 131) reported that their longest episode of pathological gambling lasted 9 or more years (mean duration=2.4 years, range=1 month to 50 years); the most common duration, reported by 45% (63 of 131) of these participants, was 1 year. The most common course of pathological gambling, characterizing 61% (74 of 120) of those with a prior history of clustered pathological gambling, was a single episode lasting 1 year or less. Of the 141 individuals with a prior history of clustered DSM-IV pathological gambling, 87 (66.6%) did not meet the diagnostic criteria for DSM-IV pathological gambling, and 57 (38.7%) had zero pathological gambling symptoms within the past 12 months. Among the participants who had experienced clustered periods of pathological gambling but did not endorse any past-year pathological gambling symptoms, the average number of years they had been completely symptom-free was 7.7 (range=1–36); 54% (29 of 57) had been symptom-free for 5 or more years.
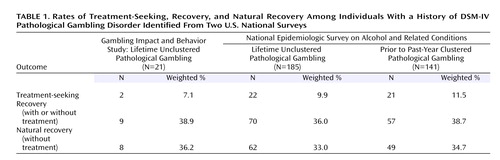
A summary of the rates of treatment-seeking, recovery, and natural recovery for DSM-IV pathological gambling obtained from the GIBS and the NESARC is presented in Table 1.
Natural Recovery and Treatment-Seeking in Problem Gambling
The rates of recovery for subthreshold levels of gambling problems—that is, problem gambling—were similar to those observed for DSM-IV pathological gambling. Problem gambling was defined as endorsing three or four symptoms of DSM-IV pathological gambling. Thirty participants in the GIBS (1.3%) (13 women, 39.7%) had a lifetime history of problem gambling. Of these, 15 (46.3%) had zero pathological gambling symptoms within the past 12 months. Three hundred thirty-two participants in the NESARC (0.8%) (122 women, 29.8%) had a lifetime history of problem gambling. Of these, 129 (39.1%) had zero pathological gambling symptoms within the past 12 months. There were no instances of treatment-seeking in the GIBS among those who had subthreshold levels of gambling problems (i.e., fewer than five lifetime pathological gambling symptoms). Treatment-seeking was not assessed for the participants with subthreshold levels of gambling problems in the NESARC survey.
Discussion
In two large national U.S. surveys, 36%–39% of the individuals with a lifetime history of DSM-IV pathological gambling did not experience any gambling-related problems in the past year. Only 7%–12% of those with a history of DSM-IV pathological gambling had sought either formal treatment or attended meetings of Gamblers Anonymous, and therefore, the vast majority of these recoveries were attained without treatment. In other words, 33%–36% of the individuals with pathological gambling disorder were characterized by natural recovery. These basic findings were replicated across two independent studies, the GIBS and the NESARC, and by using two different methods for estimating natural recovery within the NESARC study. Somewhat surprisingly, the recovery rates for problem gambling were not substantially higher than those observed for pathological gambling.
Drawing inferences about recovery from pathological gambling from a retrospective cross-sectional survey is not without limitations. For example, in retrospective cross-sectional surveys, those who are currently asymptomatic may be less likely to report previous problems, which would lead to an undercount of recovered cases (5). In addition, it is difficult to know, in longitudinal as well as cross-sectional surveys, for how long an individual should be symptom-free to be considered fully “recovered.” Not enough is yet known about the natural history of pathological gambling to know the extent to which someone who has been symptom-free for a full year will continue to be symptom-free and to represent a stable recovery. In the NESARC, over half of those with a past history of pathological gambling identified as symptom-free in the past year had been symptom-free for 5 or more years, suggesting that many of the individuals identified as being recovered represented stable recoveries.
Clues from natural recovery can potentially inform formal approaches for treating pathological gambling. For example, one obvious question is whether those who have overcome their gambling problems on their own did so by completely abstaining from any gambling or whether they were able to continue to gamble without problems. In a review of 26 studies of natural recovery from alcohol-related problems, 40% of recoveries, on average, involved low-risk drinking rather than abstinence from alcohol (23). Far fewer studies have focused on characteristics of recovery from pathological gambling. A single study of 43 media-recruited individuals who had a history of pathological gambling and had recovered from their problems (23 without formal treatment) found that most had the goal of quitting rather than reducing their gambling (24). In supplementary analyses of the GIBS in the present study, 31% (N=3) of those who had recovered from pathological gambling reported some gambling involvement in the past year, which raises the possibility that for some individuals with pathological gambling in the community, low-risk gambling might not be inconsistent with recovery from gambling problems (25).
The rates of treatment-seeking for pathological gambling were extremely low. Although pathological gambling appears to be a self-limiting disorder for many individuals, there still may be a gap between the number of people needing and the number receiving treatment for their gambling problems. This low rate of treatment-seeking is likely due to external barriers to obtaining help as well as personal factors. For example, in a study of 106 media-recruited individuals with a history of pathological gambling (43 recovered, 63 not recovered) in a large metropolitan area of Canada, the most commonly endorsed reasons for not seeking treatment were the following: wanting to handle their problems on their own, feeling that treatment was unnecessary, embarrassment/pride, stigma, and ignorance of treatment or availability (24). The recommendation made to the U.S. Congress by the National Gambling Impact Study Commission to require all gambling operations to conspicuously post and disseminate information about where to obtain treatment for gambling problems (26) will likely remove some of the external barriers to seeking treatment for pathological gambling.
The finding that roughly one-third of individuals with a history of pathological gambling recover from their problems suggests that pathological gambling does not always follow a chronic or persisting course. Other supporting evidence comes from supplementary analyses of the NESARC showing that in only a minority (N=24, 20%) of cases did episodes of co-occurring symptoms last for longer than 1 year. Neither does pathological gambling usually follow a typical relapsing or episodic course. In only a minority (27%) of cases were there more than two episodes of co-occurring symptoms of pathological gambling. The course of pathological gambling is probably best described as variable; the course of pathological gambling in some individuals was chronic, whereas in others, it was episodic. Surprisingly, the most common course of pathological gambling was a single episode of about 1 year’s duration. Perhaps the following description introduced into the fourth revision of the DSM for alcohol use disorders also applies to pathological gambling:
Clinicians often have the erroneous impression that alcohol dependence and abuse are intractable disorders based on the fact that those who present for treatment typically have a history of many years of severe alcohol-related problems. However, these most severe cases represent only a small proportion of individuals with alcohol dependence or abuse, and the typical person with an alcohol use disorder has a much more promising prognosis. (DSM-IV)
For many relatively rare psychiatric disorders, it is reasonable to turn to treatment-based samples for research participants, and until recently, this was the approach used for most of the research on pathological gambling disorder. Consequently, most of our knowledge about pathological gambling, including the cumulative knowledge represented in DSM, has been based on observations of patients in treatment. The results of this study suggest that such samples are probably not ideal for some research purposes because samples consisting of pathological gambling patients are an unrepresentative minority of individuals with pathological gambling in the community. However, the relatively low lifetime prevalence of diagnosable pathological gambling disorder of less than 1% makes it extremely challenging to assemble a representative sample of individuals with pathological gambling in the community. The group of 185 individuals with a history of DSM-IV pathological gambling identified in the NESARC study probably represents the largest such sample ever assembled and offers a rare glimpse into the characteristics of pathological gambling as it occurs in the community. Similar to the shift in modern psychiatry brought about several decades ago by the emerging results of large community-based epidemiological surveys, such as the ECA study, results of large epidemiological surveys, such as the NESARC, that are now including thorough assessments of pathological gambling, may eventually overturn some of the established wisdom about pathological gambling disorder.
 |
Received Feb. 10, 2005; revision received May 8, 2005; accepted Sept. 20, 2005. From the Department of Psychological Sciences, University of Missouri–Columbia. Address correspondence and reprint requests to Dr. Slutske, Department of Psychological Sciences, University of Missouri–Columbia, 210 McAlester Hall, Columbia, MO 65211; [email protected] (e-mail).Supported in part by NIH grant MH-66206. The Gambling Impact and Behavior Study was conducted by the National Opinion Research Center at the University of Chicago and was funded by the National Gambling Impact Study Commission (created by an act of Congress in 1997) with supplemental support from the U.S. Treasury Department, NIMH, and the National Institute on Drug Abuse. The National Epidemiologic Survey on Alcohol and Related Conditions was conducted by the Laboratory of Epidemiology and Biometry, Division of Intramural Clinical and Biological Research, National Institute on Alcohol Abuse and Alcoholism, and was funded by the National Institute on Alcohol Abuse and Alcoholism, with supplemental support from the National Institute on Drug Abuse.
1. Slutske WS, Jackson KM, Sher KJ: The natural history of problem gambling from age 18 to 29. J Abnorm Psychol 2003; 112:263–274Crossref, Medline, Google Scholar
2. Abbott MW, Williams MM, Volberg RA: A prospective study of problem and regular nonproblem gamblers living in the community. Subst Use Misuse 2004; 39:855–884Crossref, Medline, Google Scholar
3. Winters KC, Stinchfield RD, Botzet A, Slutske WS: Pathways of youth gambling problem severity. Psychol Addict Behav 2005; 19:104–107Crossref, Medline, Google Scholar
4. Hodgins DC, Wynne H, Makarchuk K: Pathways to recovery from gambling problems: follow-up from a general population survey. J Gambl Stud 1999; 15:93–104Crossref, Google Scholar
5. Robins LN, Locke BZ, Regier DA: An overview of psychiatric disorders in America, in Psychiatric Disorders in America: the Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991, pp 328-366Google Scholar
6. Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK: The de facto US mental and addictive disorders service system: Epidemiologic Catchment Area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry 1993; 50:85–94Crossref, Medline, Google Scholar
7. Potenza MN, Steinberg MA, McLaughlin SD, Wu R, Rounsaville BJ, O’Malley SS: Gender-related differences in the characteristics of problem gamblers using a gambling helpline. Am J Psychiatry 2001; 158:1500–1505Link, Google Scholar
8. National Gambling Impact Study Commission: Gambling Impact and Behavior Study, 1997-1999: United States: ICPSR Version (computer file). Ann Arbor, Mich, Interuniversity Consortium for Political and Social Research, 2002Google Scholar
9. 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions (computer file). Washington, DC, National Institute on Alcohol Abuse and Alcoholism, 2004Google Scholar
10. Toce-Gerstein M, Gerstein DR, Volberg RA: A hierarchy of gambling disorders in the community. Addiction 2003; 98:1661–1672Crossref, Medline, Google Scholar
11. Lynch WJ, Maciejewski PK, Potenza MN: Psychiatric correlates of gambling in adolescents and young adults grouped by age at gambling onset. Arch Gen Psychiatry 2004; 61:1116–1122Crossref, Medline, Google Scholar
12. Petry NM, Stinson FS, Grant BF: Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 2005; 66:564–574Crossref, Medline, Google Scholar
13. Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP: The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug Alcohol Depend 2004; 74:223–234Crossref, Medline, Google Scholar
14. Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP: Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the US: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004; 61:361–368Crossref, Medline, Google Scholar
15. Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA: Nicotine dependence and psychiatric disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 2004; 61:1107–1115Crossref, Medline, Google Scholar
16. NORC Gambling Impact and Behavior Study. http://www.norc.uchicago.edu/new/gambling.htmGoogle Scholar
17. National Institute on Alcohol Abuse and Alcoholism: National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). http://niaaa.census.gov/Google Scholar
18. Gerstein D, Volberg R, Harwood H, Christiansen E, et al: Gambling Impact and Behavior Study: Report to the National Gambling Impact Study Commission. Chicago, National Opinion Research Center at the University of Chicago, April 1, 1999. http://www.norc.uchicago.edu/new/gamb-fin.htmGoogle Scholar
19. Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R: The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend 2003; 71:7–16Crossref, Medline, Google Scholar
20. Stinchfield R: Reliability, validity, and classification accuracy of a measure of DSM-IV diagnostic criteria for pathological gambling. Am J Psychiatry 2003; 160:180–182Link, Google Scholar
21. Shaffer HJ, Hall MN, Vander Bilt J: Estimating the Prevalence of Disordered Gambling Behavior in the United States and Canada: A Meta-Analysis. Boston, Harvard Medical School Division on Addictions, 1997Google Scholar
22. Petry NM: Pathological Gambling: Etiology, Comorbidity, and Treatment. Washington, DC, American Psychological Association, 2005Google Scholar
23. Sobell LC, Ellingstad TP, Sobell MB: Natural recovery from alcohol and drug problems: methodological review of the research and suggestions for future directions. Addiction 2000; 95:749–764Crossref, Medline, Google Scholar
24. Hodgins DC, El-Guebaly N: Natural and treatment-assisted recovery from gambling problems: a comparison of resolved and active gamblers. Addiction 2000; 95:777–789Crossref, Medline, Google Scholar
25. Ladouceur R: Controlled gambling for pathological gamblers. J Gambl Stud 2005; 21:51–59Google Scholar
26. National Gambling Impact Study Commission Final Report. http://govinfo.library.unt.edu/ngisc/reports/fullrpt.htmlGoogle Scholar



