In This Issue
Addiction Biology Suggests How to Block Relapse
Among the most insidious characteristics of drug addiction is the recurring desire to take drugs, even after many years of abstinence. Repeated drug use, genetic predisposition, and environmental associations lead to long-lasting changes in brain functioning. These alterations include the neural pathways for attaching importance to drug-related stimuli and for responding to those stimuli. Kalivas and Volkow (p. 1403) describe the brain structures and neurotransmitters involved in responding to drug-taking cues, and they identify points in the dysregulated neurotransmission where pharmacologic interventions could be fruitful. Transmission of glutamate from the prefrontal cortex to the nucleus accumbens is inhibited in withdrawn addicts ordinarily, but responds excessively to drug-related stimuli. Dampening this excitatory transmission might reduce the emotional salience of these stimuli and thereby lessen relapse. Research on methods to accomplish this has targeted both presynaptic and postsynaptic mechanisms.
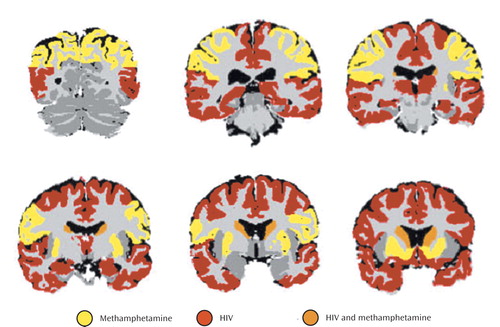
Do Brain Effects of HIV and Meth Cancel Each Other Out?
Alas, no. Jernigan et al. (p. 1461) did find that people infected with the human immunodeficiency virus (HIV) had several brain structures with lower than normal volumes and that people recovering from methamphetamine dependence had some especially large volumes. However, these brain regions were mostly not the same ones, and so people with both conditions showed additive, not compensatory, effects. The brain changes from the two conditions were differentiated by comparing dually affected patients, patients with HIV only, patients with methamphetamine dependence only, and healthy subjects. The effects on cortical structures of HIV and methamphetamine dependence, separately or together, were associated with impaired cognitive ability. Methamphetamine’s effects were more pronounced in younger subjects. The brain alterations in these dually affected people are of concern because of the growing numbers of methamphetamine abusers infected with HIV.
Marijuana: Gateway to Relapse
Marijuana has been called a “gateway” drug because its consumption often precedes use of other illegal drugs. That term may also apply to marijuana’s role in relapse after withdrawal from other illicit substances. Aharonovich et al. (p. 1507) evaluated the outcomes of people who received hospital treatment for dependence on alcohol, cocaine, or heroin. In the following year, abstinence for 26 weeks among people treated for alcohol or cocaine dependence was strongly associated with a lower rate of cannabis use. Patients who used cannabis were three times as likely to relapse after extended abstinence from cocaine and nearly five times as likely to relapse after abstinence from alcohol. Cannabis use did not affect the outcome of patients treated for heroin dependence. Therefore, in patients treated for alcohol or cocaine use disorders, use of cannabis may signal vulnerability to resumed use of the primary substance.
Mechanisms of Alcohol Craving
Avoiding relapse is a major challenge for people who have weathered detoxification from substances of abuse. How much drug craving contributes to relapse has been debated. Heinz et al. (p. 1515) found that measurements of craving were significantly correlated with alcohol intake over 6 months following inpatient treatment for alcohol dependence. Since drug craving appears to be related to dopamine neurotransmission, the capacity for dopamine synthesis and the availability of D2 and D3 dopamine receptors were also determined. Dopamine synthesis capacity in the bilateral putamen did not differ between alcoholic and healthy men but did correlate inversely with craving severity. Craving severity was also negatively correlated with the ratio of production capacity to the local availability of D2 and D3 receptors in the putamen and adjacent ventral striatum. This series of neural, psychological, and behavioral findings outlines a possible pathway from dopamine neurotransmission to alcoholic relapse.
A Paradox of Alcoholism Screening
Routine screening of medical patients for alcohol-related problems has been suggested, but this would be costly and might reveal only a few people with alcohol use disorders. The U.S. Department of Veterans Affairs (VA) calls for annual alcohol screening. Desai et al. (p. 1521) collected data on 15,580 VA patients without identified alcohol use disorders. Screening was performed for 74.2% of these patients, 4.2% had positive screening results, and 1.7% ultimately were diagnosed with alcohol use disorders. Several risk factors for alcohol use disorders—lower age, unmarried status, disability, psychiatric disorder, multiple medical conditions—were related to a lower frequency of alcohol screening. The likelihood of screening was also lower at academically affiliated medical centers, and follow-up of a positive result was less likely at the largest facilities. Although this screening identified relatively few people with alcohol use disorders, targeting high-risk patients and removing barriers to follow-up might increase this number.
Images in Psychiatry
Vladimir Bekhterev, 1857–1927 (p. 1506)