Identifying Dieters Who Will Develop an Eating Disorder: A Prospective, Population-Based Study
Abstract
OBJECTIVE: The aims of the study were to identify the characteristics of the dieters most at risk of subsequently developing an eating disorder and to evaluate the feasibility of using a brief questionnaire to identify such dieters in advance. METHOD: A general population cohort of 2,992 young women who were dieting was identified. On four occasions over the subsequent 2 years, this cohort was sent a questionnaire concerning eating habits and attitudes. Participants whose responses suggested that they had developed an eating disorder were interviewed to establish their true case status. The baseline questionnaires of those who did and did not subsequently develop an eating disorder were compared to identify features that predicted future case status. RESULTS: One hundred four of the dieters developed an eating disorder of clinical severity during the 2 years of follow-up. Their baseline questionnaire scores differed in many respects from those who had not developed an eating disorder. Items associated with developing an eating disorder were selected by using three different statistical methods. A simple case-predicting instrument based on one of five items scoring above an optimal cut point had a sensitivity of 71% and a specificity of 72% (overall efficiency of 72%). CONCLUSIONS: Dieters who will develop an eating disorder within the next 2 years have distinctive features. It is feasible to identify them in advance with reasonable efficiency with a brief questionnaire. This questionnaire could be incorporated into routine health assessments, thereby identifying those at high risk.
Eating disorders are a major source of physical and psychosocial morbidity among young women (1–3). It would be valuable to be to able detect those at most risk of developing an eating disorder, either to prevent the disorder from developing or to be able to start treatment early. Because clinical experience and research evidence have indicated that eating disorders commonly begin with behavior that resembles normal dieting (1, 4, 5), young women who are dieting constitute an important high-risk group, although only a small minority will develop an eating disorder (6, 7).
The overall aim of the present study was to develop a means of identifying young female dieters most at risk of subsequently developing an eating disorder. There were two specific aims: to determine whether there are features that predict the development of an eating disorder and to evaluate the feasibility of using a brief questionnaire to identify those at most risk.
Method
Design
A cohort of young women who were dieting but did not have an eating disorder were asked to complete a validated measure of eating disorders features. These women were then recontacted on four occasions 6 months apart and asked to complete additional copies of the same measure. At each occasion, the women whose responses suggested that they had developed an eating disorder were interviewed to confirm their diagnostic status. The initial questionnaires of the participants who had and had not developed an eating disorder were compared to identify whether there were features that predicted the subsequent development of an eating disorder and, if so, whether they could be used to construct an efficient case-predicting instrument.
Participants and Procedures
Practically all of the British population is registered with a local family physician (8). The names and addresses of the great majority of the local population are therefore to be found on family physicians’ lists. A good way of obtaining a general population study group is to contact the people on these lists. This procedure was used in the present study, the sampling frame being the patient registers of 44 family practices located in urban and rural parts of central England. The names and addresses of 17,144 women, ages 16 to 23 years inclusive, were obtained in this manner. A letter was sent to each, inviting her to take part in the study and enclosing a baseline self-report questionnaire with a stamped, self-addressed envelope. Ten thousand seventy-seven of these questionnaires (58.8%) were returned.
It is difficult to identify the true response rate in a study using this recruitment method because family physicians’ registers are invariably overinclusive, particularly with regard to this age group. This is because the registers include the names of people who have subsequently moved away but have not yet informed their physicians. Therefore, we could not conclude that nonresponse was indicative of the participants, having received the questionnaire and chosen not to take part. For this reason, we undertook a detailed pilot study using two other family practice case registers: one urban and one rural (9). This involved attempting to trace all potential participants to estimate the true response rate when one uses this recruitment method. Three of the 583 potential participants (0.5%) could not be traced, and 243 (42%) were found to have moved away. Therefore, of the 583 people listed on these two registers, only 340 (58.3%) at most still lived at the address listed. This finding suggests that the response rate in the present study is likely to have been substantially higher than the apparent figure of 58.8%.
The questionnaires of the 10,077 respondents were coded to identify those who were currently dieting. This was done by selecting those whose scores were in the top tertile on a measure of dietary restraint embedded within the questionnaire and then excluding those who reported either a current or past eating disorder or a medical condition or treatment known to affect eating habits or weight (e.g., thyroid disease, pregnancy, steroid medication). In this way, we identified 2,992 young women who were currently dieting but did not have an eating disorder or any of the other exclusion criteria.
These women formed the cohort that was followed up on four occasions over 2 years. This involved sending them more copies of the questionnaire at 6-month intervals and, if their responses suggested that they might have developed an eating disorder, asking if we might interview them. Those who agreed were then assessed (usually in their homes) with the Eating Disorder Examination interview (10). At each stage in this process, the participants were informed that they could withdraw from the study if they wished, and written informed consent was obtained from all of those who were interviewed. The study was approved by the relevant human subjects committee for each locality.
Measures
Eating Disorder Examination
The Eating Disorder Examination interview (10) was used to make diagnoses of eating disorders. The Eating Disorder Examination is widely regarded as the optimal instrument for this purpose (11–13). As part of the assessment, the participants were weighed by using calibrated portable scales, and their height was measured (thereby allowing their body mass index to be calculated: kg/m2). With this information, it was possible to apply operational definitions of the DSM-IV diagnoses of anorexia nervosa and bulimia nervosa based on the Eating Disorder Examination (10). Diagnosis of the other DSM-IV eating disorder category, eating disorder not otherwise specified, was made by two experienced clinicians (C.G.F. and Z.C.) after they were briefed in detail about the participant’s clinical state. The participants were given this diagnosis if they did not meet the diagnostic criteria for anorexia nervosa or bulimia nervosa yet clearly had an eating disorder comparable in severity to those seen among patients receiving treatment at eating disorder clinics. These judgments were made independently and blind to the participants’ identities and follow-up points. There were few disagreements between the two clinicians’ judgments, and these invariably concerned cases of threshold severity. Each was resolved upon discussion, a rule being not to make a diagnosis of eating disorder not otherwise specified if either clinician remained uncertain about the participant’s case status. The same procedure has been used in previous studies of eating disorders and their course (14, 15).
Eating Disorder Examination Questionnaire
The Eating Disorder Examination Questionnaire (16) is a self-report version of the Eating Disorder Examination interview. It has a 4-week time period, and it assesses the features of eating disorders. Four subscales may be derived from the instrument, together with a global score. The dietary restraint subscale was used in the present study as the measure of dieting. This subscale has five items comprising the following questions:
| 1. | Have you been deliberately trying to limit the amount of food that you eat to influence your shape or weight (whether or not you have succeeded)? | ||||
| 2. | Have you gone for long periods of time (8 waking hours or more) without eating anything at all in order to influence your shape or weight? | ||||
| 3. | Have you tried to exclude from your diet any foods that you like in order to influence your shape or weight (whether or not you have succeeded)? | ||||
| 4. | Have you tried to follow definite rules regarding your eating (for example, a calorie limit) in order to influence your shape or weight (whether or not you have succeeded)? | ||||
| 5. | Have you had a definite desire to have an empty stomach with the aim of influencing your shape or weight? | ||||
Each item refers to the past 28 days and is rated from 0 to 6 where 0=no days, 1=1–5 days, 2=6–12 days, 3=13–15 days, 4=16–22 days, 5=23–27 days, and 6=every day. In common with the other subscales (and the global score), the dietary restraint subscale score is the mean of the items rated.
Performance on the Eating Disorder Examination Questionnaire has been extensively studied, both in isolation and in comparison with the Eating Disorder Examination interview ((16–24). The findings indicate that in many respects the Eating Disorder Examination Questionnaire is a reasonable substitute for the Eating Disorder Examination interview. This is particularly true of the dietary restraint subscale. Questions were added to the Eating Disorder Examination Questionnaire concerning the exclusion criteria just noted.
Statistical Methods
Those who did and did not develop an eating disorder during the follow-up period were initially compared in terms of their score on the global subscale of the Eating Disorder Examination Questionnaire with an independent-sample t test to calculate statistical significance and Cohen’s effect size (d) to estimate its relative magnitude (small=0.2, medium=0.5, large=0.8). To identify whether there were specific features that predicted the development of an eating disorder, the baseline responses on the Eating Disorder Examination Questionnaire of the dieters who later developed an eating disorder were compared with the responses of those who did not. Chi-square statistics were used to determine the statistical significance of any apparent differences between individual items. Then, by using the items from the Eating Disorder Examination Questionnaire that were significantly (p<0.05) associated with future case status, three quasi-independent exploratory multiple variable analyses were performed: Cox proportional hazards regression, linear discriminant function, and signal detection analysis. The former two analyses were performed within SPSS (version 12.0) (SPSS, Chicago) and Stata/SE (version 8.2) (Stata Corp., College Station, Tex.), and both used forward stepwise selection of covariates. The signal detection analysis was performed with ROC4 (Mental Illness Research Educational and Clinical Center, Stanford, Conn.; ROC4 is available for download at http://mirecc.stanford.edu at no cost). The Cox regression and linear discriminant function results were similar for both undichotomized and dichotomized predictor variables (cut off at the optimal cut point); the latter are presented for simplicity and for consistency with the results from the signal detection analysis.
Cox proportional hazards regression analysis
This analysis was performed to determine which features were independently predictive of time to the development of an eating disorder. The results are presented as hazard ratios with 95% confidence intervals (CIs). Both graphical methods and the use of Schoenfeld residual plots (25) indicated that the proportional hazards assumption was reasonable.
Linear discriminant function analysis
This analysis was performed to identify, through the creation of a discriminant function, which features best discriminated future cases from future noncases. Unstandardized and standardized discriminant function coefficients are presented. The most efficient threshold on the function score in terms of sensitivity and specificity was identified with the use of values assigned to the costs of false positives versus false negatives and with the use of a variety of prior probabilities, including a default of 50:50 (and with a 70:30 case versus noncase ratio selected a priori as likely to generate the most useful instrument).
Signal detection analysis
This analysis was used to determine, through creation of a decision tree, the most sensitive and specific algorithm to identify future cases. Signal detection analysis is a form of recursive partitioning that considers at each step all possible predictors (at every possible cut point), with the optimum predictor and optimal cut point chosen in terms of their sensitivity and specificity. Thus, the subjects with missing data were excluded on a node-by-variable basis. The cut point was set in advance because no optimal predictor was associated with an outcome at p<0.01. The merits of signal detection analysis were summarized by Agras and colleagues (26). The analyses were performed with varying emphases on sensitivity versus specificity when 50:50 was the default. Because the avoidance of false negatives (i.e., increased sensitivity) was viewed as the priority, 70:30 was selected a priori as likely to generate the most useful instrument.
Results
Development of Eating Disorders Over Follow-Up
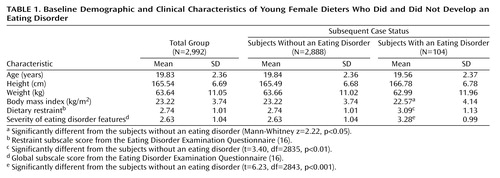
The baseline characteristics of the 2,992 young female dieters are shown in Table 1. The response rates at each follow-up point were 76%, 68%, 63%, and 60%, respectively. The amount of missing data was modest, with the great majority of items from the Eating Disorder Examination Questionnaire completed by over 97% of the participants. Those who complied with follow-up had a lower baseline global score on the Eating Disorder Examination Questionnaire than those who did not (mean=2.50, SD=1.00, versus mean=2.74, SD=1.07, respectively) (t=6.24, df=2430.5, p<0.001) (mean difference=0.24, 95% confidence interval [CI]=0.17–0.32, effect size=0.23).
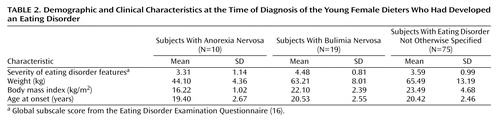
Over the follow-up, the Eating Disorder Examination Questionnaire responses of 457 participants suggested that they might have developed an eating disorder. These participants were therefore asked if they would be willing to be interviewed. Three hundred ninety-two (85.8%) agreed, of whom 104 (26.5%, 3.5% of the total study group) (95% CI=2.8%–4.2%) were found to have a DSM-IV eating disorder on the Eating Disorder Examination. Nearly forty percent (39.5%) of the cases developed within the first 6 months of follow-up, with the remainder developing at a slowly decreasing rate across the remaining 18 months (23%, 20%, and 17%, respectively). The eating disorder diagnoses of the 104 subjects were as follows: 10 with anorexia nervosa (9.6%), 19 with bulimia nervosa (18.3%), and 75 with eating disorder not otherwise specified (72.1%). Table 1 shows the baseline characteristics of those who did and did not subsequently develop an eating disorder, and Table 2 shows the characteristics of the 104 subjects with eating disorders.
An item-by-item comparison of the baseline responses on the Eating Disorder Examination Questionnaire of the participants who developed an eating disorder with those who did not revealed that the former group had significantly (p<0.05) higher scores on most of the items on the Eating Disorder Examination Questionnaire (31 of 44, 70.4%), as well as a higher overall score. A large number of items on the Eating Disorder Examination Questionnaire were therefore available for inclusion in a case-predicting questionnaire.
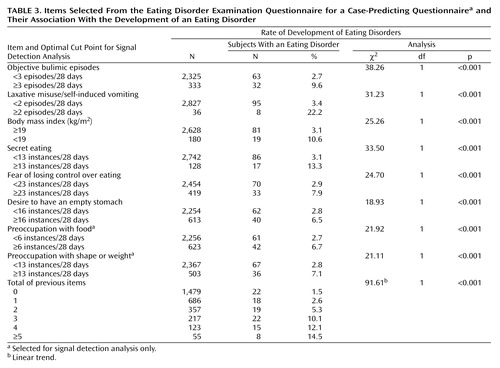
Development of a Case-Predicting Questionnaire
The results across all three statistical methods were consistent, with the same five items from the Eating Disorder Examination Questionnaire plus body mass index selected for inclusion in the potential case-finding questionnaire (Table 3). Two additional items from the Eating Disorder Examination Questionnaire were selected with the signal detection method. Increasing numbers of scores above each item’s optimal cut point were associated with an increased likelihood of developing an eating disorder. A simple screening instrument based on the presence of one single item scoring above its cut point had a sensitivity of 79% and a specificity of 52%, whereas one based on two items had a sensitivity of 62% and specificity of 76% (overall efficiency=75%).
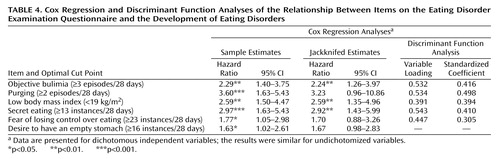
With Cox regression analysis, high scores on five items from the Eating Disorder Examination Questionnaire plus low body mass index were identified as predictive of the time for developing an eating disorder (Table 4). Jackknife validity analysis (27) indicated little bias in the model. With linear discriminant function analysis, high scores on four items from the Eating Disorder Examination Questionnaire plus low body mass index discriminated between future case and noncase status. A simple screening instrument based on one of these five items having a score above the optimal cut point had a sensitivity of 71% and a specificity of 72% (overall efficiency=72%). Similarly, decision rules and specification of prior probabilities (70:30 as optimum for sensitivity versus specificity) selected a test (threshold=0) that would correctly identify 71% of future cases (sensitivity=70.7%, 95% CI=61.0%–80.5%) with a 28% rate of false positives (specificity=72.8%, 95% CI=71.0%–74.6%). Its overall efficiency was 72.1% (95% CI=70.4%–73.8%), and its likelihood ratio was 2.54. Jackknife “leave one out” cross-validation (27) indicated that the performance of the test was excellent, with the values of the sensitivity and specificity being unchanged.
On signal detection analysis, with a 70:30 emphasis on sensitivity versus specificity, seven items from the Eating Disorder Examination Questionnaire plus body mass index were selected. The item providing the best cut point was the frequency of self-reported binge eating, followed by eating in secret, low body mass index (<19), preoccupation with food and eating, desire to have an empty stomach, frequency of purging, fear of losing control over eating, and preoccupation with shape or weight. Use of the resulting decision tree (available upon request from the first author) correctly identified 70% of future cases (sensitivity=69.5%, 95% CI=60.2%–78.8%), with a 25% rate of false positives (specificity=75.1%, 95% CI=73.4%–76.8%). Its overall efficiency was 74.9% (95% CI=73.3%–76.6%), and its likelihood ratio was 2.79. Bootstrap validation (27) confirmed the robustness of the decision tree because, although none of the trees was exactly the same (as would be expected from the way the trees are constructed), they incorporated broadly similar items with similar cut points. Moreover, the trees had comparable levels of sensitivity and specificity.
Finally, interactions between the predictor variables and age were investigated. No factor was found to have a significant interaction with age in the Cox regression model, nor did age feature in the signal detection analysis.
Discussion
The two aims of the present study were to identify the characteristics of the dieters most at risk of subsequently developing an eating disorder and to evaluate the feasibility of using a brief questionnaire to identify such dieters in advance. This necessitated recruiting a large community-based group of young women, identifying a subgroup who were currently dieting, and then following up on them at repeated intervals to see who had developed an eating disorder and who had not. These steps were accomplished, and both aims were achieved. It should be noted that the dieters were identified on the basis of a high score on a measure of dietary restraint—that is, a measure of attempting to restrict food intake—rather than a measure of actual dietary restriction. There is limited evidence that the two are separable (28). Both dietary restraint and dietary restriction are thought likely to increase the risk of developing an eating disorder through cognitive and physiological mechanisms, respectively.
As expected, only a small proportion of the dieters developed an eating disorder, and most were cases of eating disorder not otherwise specified. This high proportion of subjects with eating disorder not otherwise specified relative to subjects with anorexia nervosa and bulimia nervosa parallels the distribution of the three diagnoses in most clinical settings (29). Not surprisingly, the dieters who developed an eating disorder had more disturbed eating habits and attitudes at recruitment than those who did not, as reflected in their higher scores on the global subscale of the Eating Disorder Examination Questionnaire. Also unsurprising is the fact that several of the features that best discriminated future cases from future noncases were features that are seen in people with eating disorders, albeit at a more severe level. Other ominous features were less predictable: namely, eating in secret; preoccupation with food, eating, shape, or weight; fear of losing control over eating; and wanting to have a completely empty stomach.
There was substantial overlap in the items on the Eating Disorder Examination Questionnaire selected by the three different statistical methods. The efficiencies of the instruments derived from the discriminant function and the decision tree analyses were similar and the same as those from a simple case-predicting instrument derived from one of five items scoring above the optimal cut point (sensitivity=71%, specificity=72%). Both methods would involve completing a brief questionnaire that would identify about 70% of future cases.
The strengths of the present study include the size of the cohort, which resulted in a sufficiently large number of dieters being studied for 104 cases of eating disorder cases to develop; the method of recruitment, which circumvented certain of the selection biases that would have resulted had we advertised for dieters; and the 2-year follow-up, which provided sufficient time for many cases to develop. Other strengths include the use of clinical methods and thresholds to define case status and the fact that the core measure, the Eating Disorder Examination Questionnaire, has been well validated and is known to be acceptable to the relevant population. The relatively high rates of response are also of note.
A limitation of the study is its reliance on a measure of eating habits and attitudes to predict future case status instead of also testing the performance of other variables. We decided to focus on eating habits and attitudes for three largely pragmatic reasons. First, given current knowledge about risk factors for eating disorders (5), we thought that eating habits and attitudes were likely to be better predictors of developing an eating disorder than other variables. Second, we thought that young women who are dieting would be more willing to answer questions about their eating habits than questions about other aspects of their lives. Third, we were concerned about overburdening our participants with questions, given that they had little reason to participate. The addition of other variables might have enhanced our ability to predict future case status. Another limitation is the age and gender of the group because it did not include participants under 16 years old or men. Although an attempt has already been made to develop an instrument for use with younger teenagers (30), the relative rarity of eating disorders among men precludes them from a study of this type. A third limitation is that the participants were followed up for just 2 years, so some later-onset cases will have been missed. Fourth, the fact that those who did not comply with follow-up had higher scores on the Eating Disorder Examination than those who did may have influenced the findings. Finally, because all of our analyses were necessarily exploratory, the desirability of replication must be stressed, although in this instance, opportunities may be limited given the scale required of the research project.
In conclusion, this study has shown that young female dieters who will develop an eating disorder within the next 2 years have distinctive features and that it is potentially feasible to identify them in advance. The case-predicting questionnaire required is brief and easy to complete and score, and its content is acceptable to young women. It could therefore be incorporated into routine health assessments. Women scoring positively could be flagged, with this information made available to inform subsequent consultations. In addition, these women could be the focus of preventive interventions (31, 32). The findings may also be of relevance to young women considering embarking on weight-loss programs because the combination of dietary restraint and the features identified in the present study would confer a higher risk of developing an eating disorder. It could be argued that such women should be informed of this risk and perhaps advised against embarking on such programs. If they chose to go ahead, it would seem wise for them to do so cautiously and perhaps with some external monitoring.
 |
 |
 |
 |
Received Feb. 9, 2004; revisions received July 9 and Sept. 12, 2004; accepted Oct. 1, 2004. From the Department of Psychiatry, Warneford Hospital, Oxford University. Address correspondence and reprint requests to Dr. Fairburn, Department of Psychiatry, Warneford Hospital, Oxford University, Oxford OX3 7JX, U.K.; [email protected] (e-mail). Funded by a program grant from the Wellcome Trust (046386). Dr. Fairburn is supported by a Principal Research Fellowship from the Wellcome Trust. The authors thank Faith Barbour, Mara Catling, Guffi Chohdri, Marianne O’Connor, Carolyn Parkes, Angela Tremayne, and Gary Trent for their help with the study; the general practitioners who gave us access to their patient registers; and the participants themselves.
1. Fairburn CG, Harrison PJ: Eating disorders. Lancet 2003; 361:407–416Crossref, Medline, Google Scholar
2. Hoek HW, van Hoeken D, Katzman MA: Epidemiology and cultural aspects of eating disorders: a review, in Eating Disorders. Edited by Maj M, Halmi K, Lopez-Ibor JJ, Sartorius N. Chichester, UK, John Wiley & Sons, 2003, pp 75–104Google Scholar
3. Crow SJ, Peterson CB: The economic and social burden of eating disorders: a review. Ibid, pp 383–396Google Scholar
4. Hsu LKG: Eating Disorders. New York, Guilford, 1990Google Scholar
5. Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS: Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull 2004; 130:19–65Crossref, Medline, Google Scholar
6. Patton GC, Johnson-Sabine E, Wood K, Mann AH, Wakeling A: Abnormal eating attitudes in London schoolgirls: a prospective epidemiological study: outcome at twelve month follow-up. Psychol Med 1990; 20:383–394Crossref, Medline, Google Scholar
7. Patton GC, Selzer R, Coffey C, Carlin JB, Wolfe R: Onset of adolescent eating disorders: population based cohort study over 3 years. Br Med J 1999; 318:765–768Crossref, Medline, Google Scholar
8. Compendium of Health Statistics. London, Office of Health Economics, 1987Google Scholar
9. Beglin SJ: Eating Disorders in Young Adult Women (doctoral thesis). Oxford, UK, University of Oxford, 1990Google Scholar
10. Fairburn CG, Cooper Z: The Eating Disorder Examination, 12th ed, in Binge Eating: Nature, Assessment and Treatment. Edited by Fairburn CG, Wilson GT. New York, Guilford, 1993, pp 317–360Google Scholar
11. Garner DM: Measurement of eating disorder psychopathology, in Eating Disorders and Obesity: A Comprehensive Handbook. Edited by Fairburn CG, Brownell KD. New York, Guilford, 2002, pp 141–146Google Scholar
12. Grilo CM: The assessment and treatment of binge eating disorder. J Practical Psychiatry and Behavioral Health 1998; 4:191–201Crossref, Google Scholar
13. Wilson GT: Assessment of binge eating, in Binge Eating: Nature, Assessment and Treatment. Edited by Fairburn CG, Wilson GT. New York, Guilford, 1993, pp 227–249Google Scholar
14. Fairburn CG, Norman PA, Welch SL, O’Connor ME, Doll HA, Peveler RC: A prospective study of outcome in bulimia nervosa and the long-term effects of three psychological treatments. Arch Gen Psychiatry 1995; 52:304–312Crossref, Medline, Google Scholar
15. Fairburn CG, Cooper Z, Doll HA, Norman P, O’Connor M: The natural course of bulimia nervosa and binge eating disorder in young women. Arch Gen Psychiatry 2000; 57:659–665Crossref, Medline, Google Scholar
16. Fairburn CG, Beglin SJ: Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord 1994; 16:363–370Medline, Google Scholar
17. Black CMD, Wilson GT: Assessment of eating disorders: interview versus questionnaire. Int J Eat Disord 1996; 20:43–50Crossref, Medline, Google Scholar
18. Wilfley DE, Schwartz MB, Spurrell EB, Fairburn CG: Assessing the specific psychopathology of binge eating disorder patients: interview or self-report? Behav Res Ther 1997; 35:1151–1159Crossref, Medline, Google Scholar
19. Luce KH, Crowther JH: The reliability of the Eating Disorder Examination self-report questionnaire version (EDE-Q). Int J Eat Disord 1999; 25:349–351Crossref, Medline, Google Scholar
20. Kalarchian MA, Wilson GT, Brolin RE, Bradley L: Assessment of eating disorders in bariatric surgery candidates: self-report questionnaire versus interview. Int J Eat Disord 2000; 28:465–469Crossref, Medline, Google Scholar
21. Rizvi SL, Peterson CB, Crow SJ, Agras WS: Test-retest reliability of the Eating Disorder Examination. Int J Eat Disord 2000; 28:311–316Crossref, Medline, Google Scholar
22. Grilo CM, Masheb RM, Wilson GT: A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. J Consult Clin Psychol 2001; 69:317–322Crossref, Medline, Google Scholar
23. Carter JC, Aime AA, Mills JS: Assessment of bulimia nervosa: a comparison of interview and self-report questionnaire methods. Int J Eat Disord 2001; 30:187–192Crossref, Medline, Google Scholar
24. Passi VA, Bryson SW, Lock J: Assessment of eating disorders in adolescents with anorexia nervosa: self-report questionnaire versus interview. Int J Eat Disord 2003; 33:45–54Crossref, Medline, Google Scholar
25. Schoenfeld D: Partial residuals for the proportional hazards regression model. Biometrika 1982; 69:239–241Crossref, Google Scholar
26. Agras WS, Crow SJ, Halmi KA, Mitchell JE, Wilson GT, Kraemer HC: Outcome predictors for the cognitive behavior treatment of bulimia nervosa: data from a multisite study. Am J Psychiatry 2000; 157:1302–1308Link, Google Scholar
27. Jonathan P, Krzanowski WJ, McCarthy WV: On the use of cross-validation to assess performance in multivariate prediction. Statistics and Computing 2000; 10:209–229Crossref, Google Scholar
28. Stice E, Fisher M, Lowe MR: Are dietary restraint scales valid measures of acute dietary restriction? unobtrusive observational data suggest not. Psychol Assess 2004; 16:51–59Crossref, Medline, Google Scholar
29. Fairburn CG, Bohn K: Eating disorder NOS (EDNOS): an example of the troublesome “not otherwise specified” (NOS) category in DSM-IV. Behav Res Ther 2005; 43:691–701Crossref, Medline, Google Scholar
30. McKnight Investigators: Risk factors for the onset of eating disorders in adolescent girls: results of the McKnight Longitudinal Risk Factor Study. Am J Psychiatry 2003; 160:248–254; correction, 160:1024Link, Google Scholar
31. Piran N, Levine MP, Steiner-Adair C: Preventing Eating Disorders. Philadelphia, Brunner/Mazel, 1999Google Scholar
32. Vandereycken W, Noordenbos G: The Prevention of Eating Disorders. London, Athlone, 1998Google Scholar



