Complicated Grief, Depression, and Anxiety as Distinct Postloss Syndromes: A Confirmatory Factor Analysis Study
Abstract
OBJECTIVE: The authors used confirmatory factor analysis to replicate earlier findings that complicated grief, depression, and anxiety are distinct syndromes. METHOD: Data were derived from 1,321 bereaved individuals. Complicated grief was measured with the Inventory of Traumatic Grief. Depression and anxiety were measured with the SCL-90. RESULTS: A model in which symptoms of complicated grief, depression, and anxiety loaded on separate factors was superior to a one-factor model, revealed good model fit, and was invariant across subgroups. CONCLUSIONS: Previous findings of a distinction among complicated grief, depression, and anxiety were confirmed.
Several studies have shown that symptoms of complicated grief are distinct from symptoms of bereavement-related depression and anxiety (1). A limitation of earlier studies is that they relied on exploratory factor analysis to evaluate the latent structure of postloss symptoms, a method that does not allow for the comparative evaluation of the fit of competing models of the latent structure. Furthermore, earlier studies have hardly addressed whether the distinctiveness of the three symptom clusters holds across subgroups of bereaved individuals.
Using data from Dutch mourners, the current study aimed to extend earlier findings on this topic, using confirmatory rather than exploratory factor analysis. A first prediction was that a three-factor model with symptoms loading on three factors would be more suitable than a one-factor model. A second prediction was that—although mean levels of complicated grief could be expected to differ across particular subgroups—the three-factor structure would be invariant across subgroups.
Method
Data were available from 1,321 individuals originally recruited—along different pathways—for a research program on cognitive variables in complicated grief (2). The first group was recruited through grief counselors, therapists, clergy, and other people who met bereaved individuals through their work-related or voluntary activities. They handed out 1,128 questionnaire packets to mourners, 492 (43.6%) of which were returned. The other participants were recruited through an advertisement on a Dutch Internet site with information about grief. Information generally encompassed references to self-help literature, addresses for support, and stories of visitors. The advertisement explained that the research program was aimed at enhancing knowledge on grief and variables that influence the mourning process and invited people to participate by filling in questionnaires. People could choose to fill in questionnaires through the Internet or send an e-mail with the request to have the questionnaires sent to their homes. Six hundred individuals filled in questionnaires online, and 490 people had questionnaires sent to their homes; 260 (53.1%) of the mailed questionnaires were returned. Questionnaires differed slightly across the three groups, but all included symptom measures of complicated grief, depression, and anxiety. Participants younger than 18 years (N=31) were excluded. The final study group thus comprised 1,321 individuals. Written informed consent was obtained from all participants. Typewritten name and e-mail address in the Internet group (N=600) replaced the handwritten signature of the mailed consent forms.
The mean age of the participants was 43.2 years (SD=14.3). Most were female (N=1,084 [82.1%]), and 573 (43.4%) had lost a spouse, 187 (14.2%) a child, and 561 (42.4%) someone else. Losses occurred on average 32.5 months (SD=42.0) before the survey. Causes were nonviolent in 1,075 (81.4%) of the cases and violent in 246 (18.6%).
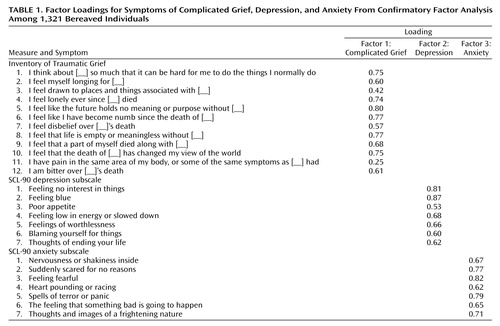
Items for the factors were selected before any model was tested. Theoretical considerations guided choices. Items for the complicated grief factor were taken from the Dutch version of the Inventory of Traumatic Grief (3), a 29-item questionnaire covering all symptoms of the refined consensus criteria for complicated grief and other problematic grief reactions. It is an extended version of the 19-item Inventory of Complicated Grief used in many earlier studies on complicated grief (1). We selected 12 items from the inventory that resembled the four separation distress and eight traumatic distress symptoms of the refined consensus criteria (Table 1). Items for the depression factor were taken from the 16-item depression subscale of the Dutch SCL-90 (4). We selected seven items corresponding closely to DSM-IV criteria of a major depressive episode, excluding items that were not part of these criteria (e.g., “crying easily”) and items that were ambiguous in the light of subjects’ circumstances (e.g., “thoughts of death”). Striving for an equal number of items in the anxiety factor, we selected seven items closely related to anxious states in DSM-IV from the 10-item anxiety subscale of the SCL-90.
AMOS 5.0 (5) was used to conduct confirmatory factor analyses. Goodness of fit was evaluated by using the comparative fit index, the Tucker-Lewis index (values >0.90 indicate good fit), and the root mean square error of approximation (values <0.08 indicate acceptable fit). Chi-square difference tests were used to evaluate the relative fit of competing models.
Results
First, a one-factor model was tested. This model did not fit the data (comparative fit index=0.733, Tucker-Lewis index=0.709, root mean square error of approximation=0.111). Next, a three-factor model was examined with symptoms loading on three distinct but correlated factors. This model fit significantly better than the unitary model (difference χ2=2956.75, df=3, p<0.001). Fit estimates reflected an acceptable model fit (comparative fit index=0.896, Tucker-Lewis index=0.886, root mean square error of approximation=0.069). Modification indexes indicated that correlations existed between the error terms of complicated grief items 5 and 8 and depression items 5 and 6. Because both complicated grief items reflected hopelessness and both depression items reflected negative self-view, we assumed that these correlations reflected nonrandom measurement error stemming from content overlap. Accordingly, we tested the fit of an adjusted three-factor model in which these error terms were allowed to be correlated. This model was a significant improvement over the second model (difference χ2=351.81, df=2, p<0.001) and had good fit estimates (comparative fit index=0.916, Tucker-Lewis index=0.907, root mean square error of approximation=0.063). Table 1 shows its factor loadings. Correlations between factors were 0.78 for complicated grief with depression, 0.58 for complicated grief with anxiety, and 0.78 for depression with anxiety.
Multiple group analyses examined the invariance of this last three-factor model across subgroups. In all analyses, restrictive models were tested with factor loadings, factor variances, and factor covariances, and residuals were constrained to be equal across subgroups. We tested the equivalence of the structure across the three groups included in this study (model 4), men and women (model 5), victims of violent versus nonviolent losses (model 6), mourners more than 1 year versus less than 1 year removed from their loss (model 7), and those who lost a partner, child, or other relative (model 8). All multiple group analyses revealed adequate fit: for model 4, comparative fit index=0.901, Tucker-Lewis index=0.903, root mean square error of approximation=0.037; for model 5, comparative fit index=0.912, Tucker-Lewis index=0.903, root mean square error of approximation=0.044; for model 6, comparative fit index=0.913, Tucker-Lewis index=0.913, root mean square error of approximation=0.043; for model 7, comparative fit index=0.913, Tucker-Lewis index=0.912, root mean square error of approximation=0.043; for model 8, comparative fit index=0.899, Tucker-Lewis index=0.901, root mean square error of approximation=0.037.
That the structure was invariant across groups does not mean that complicated grief levels were equal. The grief scores of victims of violent losses (mean=81.01, SD=21.33) on the Inventory of Traumatic Grief were slightly but significantly higher than those of victims of nonviolent losses (mean=78.15, SD=20.35) (t=–1.97, df=1318, p<0.05). Moreover, the grief scores of bereaved partners (mean=80.18, SD=20.08) and parents (mean=80.62, SD=22.44) were higher than those of other mourners (mean=76.32, SD=20.04) (F=6.10, df=2, 1315, p<0.01). No significant differences were found in grief scores between men (mean=76.37, SD=21.61) and women (mean=79.19, SD=20.29) (t=–1.92, df=1319, p=0.06) or between those less than 1 year (mean=79.87, SD=20.03) and more than 1 year (mean=78.00, SD=20.86) removed from their loss (t=1.60, df=1319, p=0.11).
Discussion
Using confirmatory factor analysis, the current study replicated earlier findings that complicated grief, bereavement-related depression, and anxiety are distinct symptom clusters. A model in which symptoms loaded on three factors was superior to a unitary model and had good fit estimates. Correlations between factors were moderate, indicating that the symptom clusters represent distinguishable but related constructs. The three-factor model was stable across subgroups of bereaved individuals, even though differences in the severity of complicated grief were found between some of those groups.
A weakness of the study is that subjects were drawn from different sources and response rates were relatively low. Therefore, generalizations of the findings should be made cautiously. Moreover, some of the subgroups included in the multiple group analyses were relatively small, which lowered the power of these analyses. Hence, further research on the invariance of the three-factor model is warranted. Nevertheless, these findings resemble those of earlier exploratory studies, most of which included similar items as indicators of the three symptom clusters, and complement the literature contending that complicated grief constitutes a distinct clinical entity.
 |
Received July 22, 2004; revision received Nov. 25, 2004; accepted Feb. 23, 2005. From the Department of Clinical Psychology, Utrecht University. Address reprint requests to Mr. Boelen, Department of Clinical Psychology, Utrecht University, P.O. Box 80140, 3508 TC Utrecht, the Netherlands; [email protected] (e-mail).
1. Lichtenthal WG, Cruess DG, Prigerson HG: A case for establishing complicated grief as a distinct mental disorder in DSM-V. Clin Psychol Rev 2004; 24:637–662Crossref, Medline, Google Scholar
2. Boelen PA, van den Bout J, van den Hout MA: The role of cognitive variables in psychological functioning after the death of a first degree relative. Behav Res Ther 2003; 1123–1136Google Scholar
3. Boelen PA, van den Bout J, de Keijser J, Hoijtink H: Reliability and validity of the Dutch version of the Inventory of Traumatic Grief (ITG). Death Stud 2003; 27:227–247Crossref, Medline, Google Scholar
4. Arrindell WA, Ettema J: [SCL 90: Manual for a Multidimensional Psychopathology Indicator.] Lisse, Switzerland, Swets & Zeitlinger, 2003 (Dutch)Google Scholar
5. Arbuckle JL: AMOS 5.0: Update to the AMOS User’s Guide. Chicago, Smallwaters, 2003Google Scholar



