A New, Empirically Established Hypochondriasis Diagnosis
Abstract
OBJECTIVE: The narrow ICD-10 and DSM-IV definition of hypochondriasis makes it rarely used yet does not prevent extensive diagnosis overlap. This study identified a distinct hypochondriasis symptom cluster and defined diagnostic criteria. METHOD: Consecutive patients (N=1,785) consulting primary care physicians for new illness were screened for somatization, anxiety, depression, and alcohol abuse. A stratified subgroup of 701 patients were interviewed with the Schedules for Clinical Assessment in Neuropsychiatry and questions addressing common hypochondriasis symptoms. Symptom patterns were analyzed by latent class analysis. RESULTS: Patients fell into three classes based on six symptoms: preoccupation with the idea of harboring an illness or with bodily function, rumination about illness, suggestibility, unrealistic fear of infection, fascination with medical information, and fear of prescribed medication. All symptoms, particularly rumination, were frequent in one of the classes. Classification allowed definition of new diagnostic criteria for hypochondriasis and division of the cases into “mild” and “severe.” The weighted prevalence of severe cases was 9.5% versus 5.8% for DSM-IV hypochondriasis. Compared with DSM-IV hypochondriasis, this approach produced less overlap with other somatoform disorders, similar overlap with nonsomatoform psychiatric disorders, and similar assessments by primary care physicians. Severe cases of the new hypochondriasis lasted 2 or more years in 54.3% of the subjects and 1 month or less in 27.2%. CONCLUSIONS: These results suggest that rumination about illness plus at least one of five other symptoms form a distinct diagnostic entity performing better than the current DSM-IV hypochondriasis diagnosis. However, these criteria are preliminary, awaiting cross-validation in other subject groups.
Somatoform disorders are among the most prevalent psychiatric disorders. Beside the suffering inflicted on the patients, somatoform disorders impose a considerable financial burden on health care (1–10).
The study of these disorders is, however, hampered by the lack of valid and reliable diagnostic categories (11–15). The individual diagnoses are poorly and arbitrarily defined and thus overlap, while other disorders are so narrowly defined that the diagnoses can hardly be applied clinically, notably in primary care (4, 7, 16–18).
Diagnostic overlap is partly rooted in research methodological practices, such as the propensity of most investigators to single out a particular diagnosis for special study rather than adopting a comprehensive view that facilitates detection of overlap. Furthermore, the empirical foundation of the somatoform diagnoses is poor, as it emanates mainly from a clinical tradition based on observation of patients in severely skewed psychiatric settings, despite the fact that these patients are mainly encountered in general medical settings.
The main focus of this study was the diagnosis of hypochondriasis, the principal diagnostic criteria for which are, according to DSM-IV, a nondelusional preoccupation with fears of harboring a severe physical disease (criterion A), persistence of the preoccupation despite appropriate medical evaluation and reassurance (criterion B), clinically significant distress or interference with functioning (criterion D), and a duration of symptoms of at least 6 months (criterion E) (19, ICD-10). Criteria B and D also apply to several other somatoform disorder diagnoses, and criterion A is frequently seen in patients with other somatoform disorders, implying an overlap problem. Furthermore, Gureje et al. (17) showed that nearly no patients in primary care fulfilled the diagnostic criteria for hypochondriasis and that the major cause for this was criterion B, i.e., it is unusual for patients not to respond to reassurance at all despite appropriate medical evaluation. Criterion E is also problematic because the time limit is arbitrary and it limits the value of the diagnosis in nonpsychiatric settings, particularly primary care, where most patients whose illness lasts more than 6 months are viewed as having chronic disorders (16). Moreover, it is hardly possible to study the effect of early intervention when by definition a diagnosis cannot be made at an early stage. Thus, the current DSM-IV hypochondriasis diagnosis satisfies neither clinical nor nosological diagnostic validity requirements.
The present situation therefore leaves us with an urgent need for empirical nosological studies on hypochondriasis. The studies must draw on appropriate patient populations, state-of-the-art assessment methods, and advanced statistical aids. Such studies should seek both to validate the current hypochondriasis diagnosis and to systematically examine whether inclusion of other symptoms known to be associated with hypochondriasis improves the validity of the diagnostic criteria.
In the present study we aimed to fill this gap by investigating whether a select range of candidate symptoms for a new hypochondriasis diagnosis cluster in certain individuals and by proposing a distinct and discrete nosological disorder entity separable from other somatoform and psychiatric disorders.
Method
The study group included 1,785 consecutive patients of Scandinavian origin (ages 18–65 years) who consulted their primary care physicians during a 3-week period for new medical problems. All participants were covered by the National Health Care Program, which includes 98% of the Danish population; each individual is registered with one primary care physician. A patient can consult only the primary care physician with whom he or she is listed. With a few exceptions, e.g., emergency cases, almost all specialized treatment, including hospital admission, requires referral from the primary care physician.
The Danish Health Care System is almost entirely tax financed, and with a few exceptions, all medical care is free of charge.
The study was a part of a large randomized, controlled trial on the effect of educating primary care physicians about the treatment of somatizing patients and the effect of diagnostic aids. All 430 primary care physicians from the 271 practices in the county of Aarhus were invited to participate in the study, and 38 agreed. There were no statistical differences between the included primary care physicians and those who declined the invitation to participate as to type of practice, length of postgraduate psychiatric training, age, or gender. However, the participating primary care physicians had less experience (mean=10.3 years, SD=7.2) than the nonparticipants (mean=14.1 years, SD=8.5) (likelihood ratio test: χ2=9.0, df=1, p=0.005), and more of them had participated in extended (more than 3 days) courses in communication skills and psychological therapy: 52.8% (19 of 36) versus 39.6% (113 of 285) (likelihood ratio test: χ2=4.0, df=1, p=0.05).
The predefined inclusion and exclusion criteria were met by 2,197 patients, of whom 274 declined the invitation to participate and 138 did not participate for other reasons (forgot their glasses, the secretary was too busy, etc.), leaving 1,785 patients for analysis. The mean age of those declining participation was 42.2 years (SD=13.1) compared with 38.8 (SD=12.9) among the included participants (t=–4.0, df=2046, p<0.001). There was no significant gender difference between the two groups. After complete description of the study to the subjects, written informed consent was obtained.
Study Design and Procedures
A two-phase design was used. First, a screening questionnaire was distributed to all patients in the waiting room. This questionnaire included, among other things, the eight-item version of the Symptom Check List (SCL) (20, 21) assessing anxiety and depression; the seven-item Whiteley index (22), which measures worrying and convictions about illness and somatoform disorders; the somatization subscale of the SCL, which checks for 12 common physical symptoms (23); and the CAGE, which consists of four questions screening for alcohol abuse (24).
After the consultation, the primary care physician filled in a questionnaire on the assessment results and his or her judgment of the patient.
Selection of Patients for Psychiatric Diagnostic Interview
The responses to each item were dichotomized. Patients with a total score of 2 or more on the eight-item SCL, the seven-item Whiteley index, or the CAGE or a score of 4 or more on the SCL somatization subscale were selected for the second phase—a psychiatric diagnostic interview. Furthermore, a random sample of one-ninth of the remaining patients was selected for interviews to produce a stratified subsample consisting of all patients with high scores and one-ninth of those with low scores. The cutoff values were chosen on the basis of a sample size calculation and the performance of the screening scales in a previous study in primary care (20, 25). The aim was to include 400 patients with somatoform disorders in the study while performing no more than 800 psychiatric interviews, which was the maximum capacity of the psychiatric interviewers. We selected 894 patients for interview, but 193 (21.6%) declined the invitation, leaving 701 patients for interview. A comparison of those declining the interview with those who completed the interview (Table 1) shows that the former group contained a higher proportion of men, was younger, and had more missing answers to the questions about sociodemographic variables. Fewer patients in the group declining interview were employed or living with a partner, and fewer had an education beyond basic schooling. They had lower scores on the SCL somatization subscale than did the patients who completed interviews (2003 unpublished study by T. Toft et al.).
Psychiatric Research Interview
The psychiatric interview was conducted as soon as possible after the index contact, in the primary care physician’s office, in the research unit’s office, or in the patient’s own home. The patients’ transportation expenses were reimbursed. For patients who could not be interviewed immediately, the interview did not include the period after the index contact.
The psychiatric interviews were made by means of the Schedules for Clinical Assessment in Neuropsychiatry (SCAN), version 2.1 (26, 27), which is a standardized comprehensive interview endorsed by the World Health Organization (WHO) that covers all types of mental disorders. It is a semistructured interview, and its use requires an interviewer who has received psychiatric training. The interview lasts between 30 minutes, in cases of no health problems, and several hours, in cases of more massive psychopathology (the maximum in this study was 7 hours). In this study the interviewers were free to explore aspects they did not find fully clarified by the interview, e.g., by reviewing medical records. However, they were not allowed to contact the primary care physicians.
In the literature a range of cognitive and emotional symptoms, beside those specified in DSM-IV (and ICD-10), are commonly reported in patients with hypochondriasis (19, 28–30):
| 1. | Worrying about or preoccupation with fears of harboring a severe physical disease (DSM-IV and ICD-10 criterion A). | ||||
| 2. | Bodily preoccupation, i.e., an absorption with the body and its functioning, e.g., body excretion, physiological function, sensations, appearance, and body performance. | ||||
| 3. | Obsessive rumination with intrusive thoughts and ideas and fears of harboring an illness that cannot be stopped or can be stopped only with great difficulty. | ||||
| 4. | Suggestibility or autosuggestibility: responding with alarm to the slightest hint of illness; alarm may arise from reading about a disease, knowing someone who becomes sick, etc. | ||||
| 5. | Extensive fascination with medical information: reading medical books or journals, reading about medical subjects in an encyclopedia, watching television programs about health or medicine, being interested in news about health, etc. | ||||
| 6. | Unrealistic fear of being infected or contaminated by something touched or eaten, by a person met, etc. | ||||
| 7. | Pathological, excessive health-preserving behavior, i.e., eating special food, extensive exercise, or overdoing other things to keep fit. | ||||
| 8. | Focusing primarily on causality: the patient wants an explanation for the symptoms and is more concerned about the meaning of the symptoms than the distress they cause. | ||||
| 9. | Fear of taking prescribed medication. | ||||
These and other candidate symptoms included in the diagnostic research criteria for different somatoform diagnoses were added to the SCAN interview section on physical health. The new questions were integrated in such a way that they appeared to be a natural part of the interview, and the definition of each new symptom was added to the glossary, which is a part of the SCAN interview. Each of the symptoms is rated 0 (“absent”), 1 (“mild to modest preoccupation but no significant distress or impairment”), or 2 (“excessive preoccupation involving severe daily troubles or numerous consultations or self-medication”). In the analysis the symptom ratings 1 and 2 were collapsed. “The duration of hypochondriacal preoccupation” (months) caused by any of the rated symptoms and “interference with everyday activity because of these problems” are additionally rated as separate items in the SCAN. The modified version with definitions of all the symptoms included in this article is available from the authors on request.
The SCAN interviews were conducted by six psychiatric physicians (including T.T.) who were all highly skilled in psychopathological assessment, intensively trained in using the SCAN interview, and certified at the WHO center in Copenhagen. They had all received psychiatric residency training and had at least 2 years of medical and surgical residency experience. During the study they met at least once a week to discuss cases and how to interpret and rate dubious responses and symptoms that seemed to fall between the numeric ratings, and they were free to consult more senior doctors.
Patients scheduled for Thursdays at 1:00 p.m. were asked to give permission for the interview to be videotaped. The videotaped interviews of the eight patients who accepted were rated by all the interviewers, and these ratings showed a high interrater agreement on the presence or absence of any psychiatric diagnosis (kappa=0.86) as well as on the somatoform diagnostic category (kappa=0.82) (unpublished 2003 article by Toft et al.). The interviewers were blinded to the patients’ responses on the screening questionnaires.
Data Analysis
The SCAN interviews were used for computerized DSM-IV psychiatric diagnoses with reference to the “present state” (current mental disorder) and “lifetime before” (the patient’s psychiatric history). In this article we present only the data on current mental disorder. The section on physical health containing information on the somatoform disorders and related diagnoses was processed separately in order to make the diagnoses fit the DSM-IV criteria and to analyze the added symptoms.
We processed the data in STATA (31) and SPSS (32), and for the latent class analysis we used WINMIRA (33) and Mplus(34).
Group comparisons were made by chi-square tests for categorical data, and the Mann-Whitney U test or Kruskal-Wallis test was used for nonnormal continuous data. We estimated prevalence by weighted logistic regression with the observed fraction of second-phase patients as sample weights (35). To assess the equality of prevalences in subgroups, likelihood ratio tests were performed.
The model selection in latent class analysis was based on different information criteria, with the sample-size-adjusted Baye’s information criterion (SS BIC) as the primary criterion (34).
In order to assess the goodness of fit of the final selected model, the Pearson chi-square fit statistic and an empirical Pearson chi-square fit statistic were computed.
Two-sided p values are reported.
Ethics
All biomedical studies in Denmark must be approved by the local Science Ethics Committee, which is subject to the laws and regulations laid down by the Danish government. We obtained approval from the Science Ethics Committee of Aarhus County.
All the participating patients received written and oral information and gave written informed consent.
Results
Diagnostic Classes
The nine candidate symptoms for a new hypochondriasis diagnosis were tested in a latent class statistical model with the number of classes varying between two and six. The model with the smallest SS BIC was chosen as optimal, but it did not have a meaningful interpretation. We assessed SS BIC as we excluded one symptom at a time. We excluded “pathological, excessive health-preserving behavior” and “focusing primarily on causality,” and an interpretable three-class model emerged. However, the high intercorrelation (rs=0.37, N=701, p<0.001) and marked prevalence in either somatoform disorders class of the symptoms “worrying/preoccupation” and “bodily preoccupation” made it expedient to collapse the two symptoms into one item. The final model, displayed in Table 2, thus includes six symptom items. This model’s goodness of fit is acceptable (Pearson χ2=50.9, df=50, p=0.19, empirical p=0.20). It is seen that 14.6% of the interviewed patients fell into latent class 1, in which positive responses to most items were prevalent. The symptom “rumination” was highly predictive for this class: only three of the patients reporting this symptom did not fall into this class. None of these three patients reported any of the other six symptoms. This group should therefore be classified as patients with hypochondriasis. Class 2 comprised 34.8% of the patients, and most of the investigated symptoms were prevalent in this class except for “rumination” and “fear of being infected.” Class 3 included 50.6% of the patients, and few reported any of the explored symptoms. The prevalences of the symptoms in the hypochondriasis class (class 1) were similar to or higher than those among the patients fulfilling the diagnostic criteria for DSM-IV hypochondriasis; the most marked difference was for “rumination” (Table 2).
The key symptom (criterion A) of DSM-IV hypochondriasis, “preoccupation with fears of having…a serious disease,” is thus frequent in both class 1 and class 2, and the poor specificity of the symptom is furthermore highlighted by the fact that 84.6% of the 26 patients with a somatization disorder diagnosis and 58.4% of the 77 patients with pain disorder also had the symptom.
All patients in the hypochondriasis class (class 1) reported two or more symptoms, and 45.1% reported four or more symptoms. The patients in the two other classes and those with DSM-IV hypochondriasis reported fewer symptoms. Only 13.0% of the patients in class 3 (patients with nonsomatoform illness) reported any of the six symptoms (Table 2).
Clinical Diagnosis of Hypochondriasis
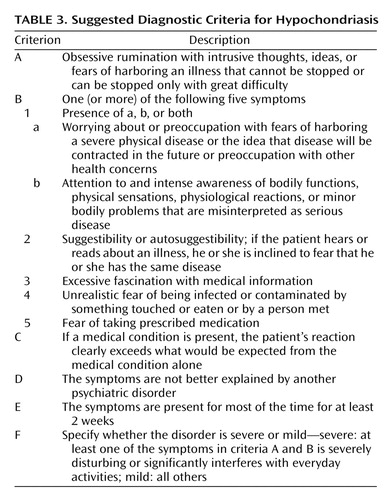
We manually reviewed the patterns of the latent class results to turn the statistical information derived from analysis of the hypochondriasis class into operational diagnostic criteria for clinical use and to establish a new set of diagnostic criteria for hypochondriasis (Table 3). The only difference between the hypochondriasis class (class 1) and the diagnostic criteria displayed in Table 3 is item E, i.e., the symptoms should be present for at least 2 weeks. This criterion was added from a clinical point of view to avoid diagnosing the most transient cases. We also introduced a severity item, item F, making it possible to distinguish between mild and severe cases. Patients with severe and mild cases did not display significantly different numbers of symptoms. In the remaining part of this article, we will report data on the latent classes subdivided into severe cases, i.e., in which the patient states that at least one of the symptoms listed in Table 2 is severe or distressing or states that any of the somatoform symptoms severely interferes with everyday activities, and into mild cases, i.e., not causing significant impairment or distress.
Associated Symptoms and Characteristics
For 54.3% of the patients with severe hypochondriasis (class 1), the illness lasted for 2 years or more. It lasted 5 years or more for 42.0% and 10 years or more for 24.7%. Its duration was a month or less for about 27.2%, which was about the same duration as for patients fulfilling the DSM-IV criteria (Table 4). The illness lasted a remarkable 2 years or more in 38.1% of the patients with mild class 1 hypochondriasis.
The patients with severe class 1 hypochondriasis had a median age at onset of 25 years; the earliest onset was at age 5, and the latest was at 60. For comparison, the patients with DSM-IV hypochondriasis had a median age at onset of 20 years, with a minimum age of 6 and a maximum of 52. The other groups had higher onset ages, but in some of the groups the number of patients was small, and in the class 3 group more than one-half of the patients were not counted because the patients had no somatoform symptoms, making it impossible to register onset age.
Table 4 also lists a range of symptoms commonly reported in different somatoform disorders.
“The preoccupation persists despite appropriate medical evaluation and reassurance” is criterion B of the DSM-IV criteria for hypochondriasis and was found in about one-half of the patients with severe class 1 hypochondriasis. However, the symptom was also frequent in those with mild class 1 hypochondriasis and in patients in the class 2 group (other somatoform disorders). In addition, the symptom was frequent among the 26 patients with somatization disorder (73.1%) and the 77 patients with pain disorder (24.7%) (data not shown in Table 4). Of the patients with severe class 1 hypochondriasis, 42.0% were found to use a “psychosocial communication style,” i.e., the patients focused on the psychosocial consequences of their illness and the restrictions to their lives rather than on the symptoms’ implications for their health. This symptom was, however, also frequent in the other groups with severe forms of illness. Except for doctor shopping, about one-third or more of the patients in the severe class 1 and class 2 groups and in the DSM-IV hypochondriasis group had each of the listed symptoms, showing that the symptoms are prevalent in somatoform disorders but none seems to be distinctively associated with one category in particular.
Except for the mild class 2 and class 3 categories, the average patient in each class presented multiple medically unexplained symptoms from many organ systems, and the DSM-IV hypochondriasis group had the most (Table 4).
Comorbidity
A modest overlap or comorbidity between severe class 1 hypochondriasis and the other somatoform disorders was reflected in the fact that about one-tenth to one-third of the patients with severe class 1 hypochondriasis also fulfilled the criteria for one of the diagnoses listed in Table 5. For all somatoform disorder diagnoses, the overlap was higher among the patients with DSM-IV hypochondriasis, and for undifferentiated somatoform disorder it was considerably higher. Only one patient fulfilled the diagnostic criteria for conversion disorder, which were therefore excluded from Table 5. The category of somatoform disorder not otherwise specified is an exclusion diagnosis and was therefore also left out. Only 30.9% of the patients with severe class 1 hypochondriasis and 16.9% of those with severe class 2 disorders fulfilled the diagnostic criteria for DSM-IV hypochondriasis (Table 5). On the other hand, 83.1% of the DSM-IV hypochondriasis patients had severe class 1 or class 2 disorders.
Patients with severe class 1 hypochondriasis and those with DSM-IV hypochondriasis had similar rates of comorbidity with nonsomatoform psychiatric disorders: 49% in each group (Table 5). The interviewers judged depression to be predominant in three of the 14 patients meeting the diagnostic criteria for both major depression and severe class 1 hypochondriasis and in three of the nine patients with DSM-IV hypochondriasis and depression.
Only three patients fulfilled the criteria for obsessive-compulsive disorder (OCD), and none of these fell into class 1 or class 2, whereas one of them had DSM-IV hypochondriasis.
Primary Care Physician Assessments
The primary care physicians, not knowing the patients’ diagnoses, judged that 40.0% of the patients with severe class 1 hypochondriasis had a low care-seeking threshold (Table 6). They also found that 62.0% were more preoccupied with bodily sensations or illness than would be expected and that 71.3% were overly fearing illness or worrying about illness, of whom 45.0% could not be reassured or could only with difficulty be reassured that their worrying was biomedically unfounded. In 75.9% of the patients with severe class 1 hypochondriasis, the primary care physicians reported that the patient frequently consulted them because of medically unexplained functional symptoms. The rates at which the primary care physicians attributed these characteristics to patients were highest for patients with severe class 1 hypochondriasis in all instances, but even patients with mild class 1 hypochondriasis had comparatively high rates. High rates were also recorded for some of the other groups but not for patients with mild cases of class 3 disorders. The rates for the patients with severe class 1 hypochondriasis were similar to those for the DSM-IV hypochondriasis patients. Since “the preoccupation persists despite appropriate medical evaluation and reassurance” is included in the DSM-IV diagnostic criteria but not among the class 1 symptoms, it is remarkable that the primary care physicians found it difficult to reassure the same fraction of class 1 and DSM-IV hypochondriasis patients.
Prevalence
Table 7 displays the weighted prevalences corrected for the biases introduced by the stratified patient sampling. The prevalence of severe class 1 hypochondriasis was 9.5%, compared with 5.8% for DSM-IV hypochondriasis without exclusion of comorbid diagnoses and 4.7% (95% CI=2.9%–7.6%) with the full DSM-IV criteria.
Severe other somatoform disorders (class 2) were significantly more prevalent in the patients who were 40–49 years old than in the other age groups, and the patients with severe nonsomatoform disorders (class 3) were significantly older than patients in the other classes. Inversely, patients with mild class 1 hypochondriasis were significantly younger than the other patients. There were no statistically significant differences as to age or gender among the other classes or in DSM-IV hypochondriasis.
Discussion
Robins and Guze (36) and later Kendell (37) listed a range of strategies for establishing the validity of clinical syndromes; the first is to identify and describe the syndrome by “clinical intuition” or by cluster analysis, and the second is to demonstrate boundaries or “point of rarity” between related syndromes by statistical methods. The current DSM-IV hypochondriasis diagnosis rests mainly on “clinical intuition” and tradition, and it is not supported by substantial empirical evidence. To our knowledge, no studies have established a “point of rarity” between the DSM-IV hypochondriasis diagnosis and other somatoform disorder diagnoses, and we did not find support for this in the current study either, as the key symptoms included in the DSM-IV diagnostic criteria (criteria A and B) were also common among patients with other somatoform disorder diagnoses. In this study we included a range of symptoms reported to be common or typical for hypochondriasis (19, 28, 29). We used latent class analysis, a robust statistical method that from a statistical point of view produces a rather clearcut result, establishing a “point of rarity” between classes. Six of the nine symptoms explored fitted satisfactorily into a latent class model with three classes: a hypochondriasis class (class 1), a class of “other somatoform disorders” (class 2), and a class of nonsomatizing patients (class 3). However, even class 3 included some patients with medically unexplained symptoms, and further studies are needed to establish whether this class is truly a nonsomatizing group or a somatoform disorder subgroup without cognitive or emotional symptoms. The suggested diagnostic criteria have to be viewed as preliminary, as the criteria, among other validation procedures, have to be cross-validated in another group of subjects.
From a methodological point of view, the major strength of this study lies in its empirical foundation, in particular its inclusion of a large number of patients gathered in a nonspecialized medical setting. Further strengths include almost complete absence of selection bias, owing to the fact that Danish health care is free of charge, and use of a standardized psychiatric interview, the SCAN, which is state of the art and probably the most advanced and comprehensive diagnostic tool for psychopathology and psychiatric diagnostics available today (26, 27). The interview section on physical issues comprises questions about all types of somatoform symptoms and hence allows simultaneous study of all known types of somatoform disorders. The interviewers were all highly skilled in psychopathology assessment and intensively trained in using the SCAN interview. The candidate symptoms we added to the SCAN interview were feasible and reliable according to the interviewers.
We expected “bodily preoccupation” to be a distinct hypochondriasis symptom as bodily symptom amplification has been suggested to be a basic mechanism in hypochondriasis (38, 39), but like “preoccupation with…disease,” it was just as frequent among class 2 patients as among patients with hypochondriasis, and furthermore, the symptoms were frequent among other DSM-IV somatoform disorders. With the addition of “extensive fascination with medical information,” the three symptoms may collectively be viewed as common symptoms of somatoform disorders in general. According to our findings, the missing discriminatory power of these symptoms may therefore be the explanation for the overlap between DSM-IV hypochondriasis and other somatoform disorder diagnoses in the current classification system, as the symptom “preoccupation with…disease” is the key symptom (criterion A) in the DSM-IV diagnostic criteria for hypochondriasis.
“Obsessive rumination” proved to have a strong power to discriminate between the patients with hypochondriasis and other patients, and “fear of being infected or contaminated” also appeared to be quite distinctive. These two symptoms outperformed the other symptoms in establishing class 1 hypochondriasis, which raises the question of whether hypochondriasis should be viewed as an OCD spectrum disorder, i.e., “OCD bodily type,” or alternatively, a specific illness phobia. This question cannot be addressed on the basis of this study. None of the three patients with OCD found in this study had class 1 hypochondriasis, and other symptoms atypical for OCD were also common among the patients with class 1 hypochondriasis. It has been suggested that the hypochondriasis diagnosis be moved from the somatoform disorder category to the anxiety disorder category as a “health anxiety disorder,” thus replacing the stigmatizing hypochondriasis label. Despite possible support for this view, it calls for caution regarding premature conclusions; we should keep in mind the discussion in the 1960s and 1970s about whether hypochondriasis should be viewed as a depressive disorder because hypochondriacal worrying is also common in depressive disorders (40). Instead, a more neutral replacement may be considered, for example the term “valetudin disorder,” which originates from the Greek word valetudo, meaning “the state of health” (41).
The criteria for class 1 hypochondriasis enjoyed high statistical, clinical, and “face” validity, even compared with the assessments of primary care physicians, but confirmation from daily clinical practice is, of course, needed. It is remarkable that the primary care physicians’ assessments of the patients with severe class 1 hypochondriasis were similar to those for the patients with DSM-IV hypochondriasis despite the fact that class 1 hypochondriasis was about twice as prevalent as DSM-IV hypochondriasis. This may indicate that the class 1 criteria do not pick up more clinically insignificant cases than the DSM-IV diagnosis. Furthermore, it indicates that the DSM-IV hypochondriasis cases not included in the class 1 category in fact may be other somatoform disorders and that they ought to be classified in other subcategories. The class 1 hypochondriasis diagnosis also enjoys the advantage of not being an exclusion diagnosis, i.e., not requiring exclusion of a medical explanation of physical symptoms. It relies solely on positive diagnostic criteria in the form of cognitive and emotional symptoms, hence matching the diagnostic principles of other psychiatric diagnoses. The present study does not allow us to establish whether the full syndrome may emerge as a reaction to a newly diagnosed severe physical disease, as it was conducted in a primary care setting, where the number of such cases was low. We do, however, expect such psychological reactions to be only transient. In patients with the full syndrome, the psychological reaction would probably be clinically significant and encourage intervention, even if the patient also had a severe physical disease.
The class 1 hypochondriasis diagnosis had some comorbidity with other somatoform disorders, but its overlap was smaller than that for DSM-IV hypochondriasis and smaller than that reported in other studies (17, 42, 43). The magnitude of the overlap between class 1 hypochondriasis and other somatoform disorders was comparable to the overlap between depressive disorder and anxiety disorder (data not reported). The overlap may not necessarily be due to inappropriate diagnostics or overlap of diagnostic criteria; it might also be due to the patients’ suffering from two distinctly independent disorders.
The overlap of DSM-IV hypochondriasis and severe class 1 hypochondriasis was only modest; about one-half of the DSM-IV hypochondriasis cases fell into class 1. Another half fell into class 2, other somatoform disorders. This seems to highlight the poor discriminatory power of the current DSM-IV hypochondriasis diagnosis, as these patients could be split into two distinct groups by latent class analyses of six symptoms. The use of an exploratory approach requires imposition of a minimum of analytical restrictions, and the DSM-IV hierarchical exclusion rules were therefore not used for patients meeting the criteria for more than one diagnosis. Use of the full DSM-IV hypochondriasis criteria, however, made little change (data not reported).
The prevalence of severe class 1 hypochondriasis reached 9.5%, which testifies to its high prevalence among primary care patients. The prevalence of DSM-IV hypochondriasis based on the full criteria (i.e., including the exclusion criteria) was 4.7%, which is higher than in most other studies in primary care, in which prevalence rates have been 0.0%–6.3% (17, 44).
One of the strengths of the present study lies in its use of a more extensive diagnostic procedure (i.e., the SCAN interview) than was used in other studies and the use of experienced psychiatric interviewers. We included only “incident” cases, i.e., those of patients presenting with new health problems, thus excluding some patients with chronic physical diseases. In accordance with most other studies, we found no gender or age difference in the prevalence of hypochondriasis (17, 44, 45). About 10% of the primary care physicians in the county participated in the study. This may raise the possibility that a practice selection bias limits the generalizability of the prevalence figures. However, the participating primary care physicians seem to be remarkably representative of the overall population of primary care physicians in the county on most of the variables on which they were compared.
This study focused mainly on class 1 hypochondriasis, but class 2, nonhypochondriasis somatoform disorders, may be just as interesting. This calls for a more profound and focused exploration of the nonhypochondriasis diagnostic categories, which is outside the limits of this article, but we plan to conduct such separate analyses.
The hypochondriasis diagnosis as defined in ICD-10 and DSM-IV has shown to be so restrictive that few patients in primary care fulfill the diagnostic criteria (17). Gureje et al. (17) showed that one of the major problems is the symptom “the preoccupation persists despite appropriate medical evaluation and reassurance”(i.e., criterion B), and Barsky et al. (16) have pointed to the problem of the 6-month time limit (criterion E). The diagnostic criteria suggested in this study do not include these two symptoms and therefore overcome these shortcomings of the current DSM-IV hypochondriasis diagnosis. To replace the duration criterion of 6 months, however, from a purely clinical and not statistical point of view, we suggest the adoption of a severity criterion, i.e., that the symptoms must cause significant distress or impairment in order to be considered clinically significant. However, the patients with “mild” cases (i.e., those with no significant impairment or distress) may still be clinically relevant, especially in a primary care setting. The symptom durations were identical among patients with functional impairment or distress and patients without it, and the latter group also presented multiple medically unexplained symptoms. We may therefore speculate whether the “mild” cases are a type of latent or subclinical hypochondriasis with a high risk of evolving into the manifest clinical syndrome under stressful conditions. Further studies will elucidate the potential implications of the mild syndrome for health care utilization and health-related quality of life and may, if the results are affirmative, warrant inclusion of the mild diagnostic category in the diagnostic classification system as suggested here.
A third point in the validation process, according to Kendell (37), is to perform follow-up studies to establish a distinct course or outcome. This was not undertaken in the present study, but the included patients are being followed. However, as the symptoms had lasted for a long period in a high fraction of the patients with class 1 hypochondriasis, the present data indicate that the symptoms pursue a distinct course and that the diagnosis remains stable. Kendell (37) proposed three more strategies: 1) therapeutic trials to establish a distinct treatment response, 2) family studies establishing that the syndrome “breeds true,” and 3) demonstration of the association with some more fundamental abnormalities, i.e., anatomical, biochemical, or molecular. Such validation studies, as well as cross-validation studies in other subjects, have still to be planned.
Acknowledgments
This study is a part of the Functional Illness in Primary Care study, conducted by the Research Group for Functional Illness in Primary Care. The research group includes the following institutions: the Research Unit for Functional Disorders, Psychosomatics and CL Psychiatry, Aarhus University Hospital; the Research Unit for General Medicine, University of Aarhus; the Department of Ethnography and Social Anthropology, University of Aarhus; and the Department of Psychology, University of Aarhus.
 |
 |
 |
 |
 |
 |
 |
Received Sept. 5, 2002; revision received Oct. 29, 2003; accepted Nov. 5, 2003. From the Research Unit for Functional Disorders, Psychosomatics and CL Psychiatry, Aarhus University Hospital; and the Research Unit for General Medicine, University of Aarhus. Address reprint requests to Dr. Fink, Research Unit for Functional Disorders, Aarhus University Hospital, DK-8000 Aarhus C, Denmark; [email protected] (e-mail). Supported by grants from the Danish Medical Research Council (grant 2028-00-0007) and the Quality Improvement Committee for General Practice in Aarhus County. The authors thank the participating interviewers and primary care physicians.
1. Ewald H, Rogne T, Ewald K, Fink P: Somatization in patients newly admitted to a neurological department. Acta Psychiatr Scand 1989; 89:174–179Crossref, Google Scholar
2. Fink P: The use of hospitalizations by persistent somatizing patients. Psychol Med 1992; 22:173–180Crossref, Medline, Google Scholar
3. Hansen MS, Fink P, Frydenberg M, Oxhoj M, Sondergaard L, Munk-Jørgensen P: Mental disorders among internal medical inpatients: prevalence, detection, and treatment status. J Psychosom Res 2001; 50:199–204Crossref, Medline, Google Scholar
4. Kirmayer LJ, Robbins JM: Three forms of somatization in primary care: prevalence, co-occurrence, and sociodemographic characteristics. J Nerv Ment Dis 1991; 179:647–655Crossref, Medline, Google Scholar
5. Gureje O, Simon GE, Ustun TB, Goldberg DP: Somatization in cross-cultural perspective: a World Health Organization study in primary care. Am J Psychiatry 1997; 154:989–995Link, Google Scholar
6. Fink P: Surgery and medical treatment in persistent somatizing patients. J Psychosom Res 1992; 36:439–447Crossref, Medline, Google Scholar
7. Fink P, Sorensen L, Engberg M, Holm M, Munk-Jørgensen P: Somatization in primary care: prevalence, health care utilization, and general practitioner recognition. Psychosomatics 1999; 40:330–338Crossref, Medline, Google Scholar
8. Escobar JI, Golding JM, Hough RL, Karno M, Burnam MA, Wells KB: Somatization in the community: relationship to disability and use of services. Am J Public Health 1987; 77:837–840Crossref, Medline, Google Scholar
9. Barsky AJ, Ettner SL, Horsky J, Bates DW: Resource utilization of patients with hypochondriacal health anxiety and somatization. Med Care 2001; 39:705–715Crossref, Medline, Google Scholar
10. Simon GE: Psychiatric disorder and functional somatic symptoms as predictors of health care use. Psychiatr Med 1992; 10:49–59Medline, Google Scholar
11. Bass C, Murphy MR: Somatization disorder: critique of the concept and suggestions for future research, in Somatization: Physical Symptoms and Psychological Illness. Edited by Bass C. Oxford, UK, Blackwell Scientific Publications, 1990, pp 301–332Google Scholar
12. Murphy MR: Classification of the somatoform disorders. Ibid, pp 10–39Google Scholar
13. Fink P: Somatization—beyond symptom count. J Psychosom Res 1996; 40:7–10Crossref, Medline, Google Scholar
14. Rief W, Heuser J, Mayrhuber E, Stelzer I, Hiller W, Fichter MM: The classification of multiple somatoform symptoms. J Nerv Ment Dis 1996; 184:680–687Crossref, Medline, Google Scholar
15. Mayou R: Somatoform disorders and medically unexplained symptoms, in New Oxford Textbook of Psychiatry, vol 2. Edited by Gelder MG, López-Ibor JJ, Andreasen NC. New York, Oxford University Press, 2000, pp 1073–1076Google Scholar
16. Barsky AJ, Wyshak G, Klerman GL: Transient hypochondriasis. Arch Gen Psychiatry 1990; 47:746–752Crossref, Medline, Google Scholar
17. Gureje O, Ustun TB, Simon GE: The syndrome of hypochondriasis: a cross-national study in primary care. Psychol Med 1997; 27:1001–1010Crossref, Medline, Google Scholar
18. Fink P: Somatization disorder and related disorders, in New Oxford Textbook of Psychiatry. Edited by Gelder MG, López-Ibor JJ, Andreasen NC. New York, Oxford University Press, 2000, pp 1080–1088Google Scholar
19. Barsky AJ, Wyshak G, Klerman GL: Hypochondriasis: an evaluation of the DSM-III criteria in medical outpatients. Arch Gen Psychiatry 1986; 43:493–500Crossref, Medline, Google Scholar
20. Fink P, Jensen J, Borgquist L, Brevik JI, Dalgard OS, Sandager I, Engberg M, Hansson L, Holm M, Nordström G, Stefansson CG, Sørensen L, Munk-Jørgensen P: Psychiatric morbidity in primary public health care: a Nordic multicenter investigation, part I: method and prevalence of psychiatric morbidity. Acta Psychiatr Scand 1995; 92:409–418Crossref, Medline, Google Scholar
21. Fink P, Ørnbøl E, Hansen MS, Sondergaard L, De Jonge P: Detecting mental disorders in general hospitals by the SCL-8 scale. J Psychosom Res 2004; 56:371–375Crossref, Medline, Google Scholar
22. Fink P, Ewald H, Jensen J, Sorensen L, Engberg M, Holm M, Munk-Jørgensen P: Screening for somatization and hypochondriasis in primary care and neurological in-patients: a seven-item scale for hypochondriasis and somatization. J Psychosom Res 1999; 46:261–273Crossref, Medline, Google Scholar
23. Derogatis LR, Cleary PA: Confirmation of the dimensional structure of the SCL-90: a study in construct validation. J Clin Psychol 1977; 33:981–989Crossref, Google Scholar
24. Ewing JA: Detecting alcoholism: the CAGE questionnaire. JAMA 1984; 252:1905–1907Crossref, Medline, Google Scholar
25. Munk-Jørgensen P, Fink P, Brevik JI, Dalgard OS, Engberg M, Hansson L, Holm M, Joukamaa M, Karlsson H, Lehtinen V, Nettelbladt P, Stefansson C, Sørensen L, Jensen J, Borgquist L, Sandager I, Nordström G: Psychiatric morbidity in primary public health care, a multicentre investigation, part II: hidden morbidity and choice of treatment. Acta Psychiatr Scand 1997; 95:6–12Crossref, Medline, Google Scholar
26. SCAN: Schedules for Clinical Assessment in Neuropsychiatry, version 2.1. Geneva, World Health Organization, Division of Mental Health, 1998Google Scholar
27. Eaton WW, Neufeld K, Chen LS, Cai G: A comparison of self-report and clinical diagnostic interviews for depression: Diagnostic Interview Schedule and Schedules for Clinical Assessment in Neuropsychiatry in the Baltimore Epidemiologic Catchment Area follow-up. Arch Gen Psychiatry 2000; 57:217–222Crossref, Medline, Google Scholar
28. Barsky AJ, Ahern DK, Bailey ED, Saintfort R, Liu EB, Peekna HM: Hypochondriacal patients’ appraisal of health and physical risks. Am J Psychiatry 2001; 158:783–787Link, Google Scholar
29. Rief W, Hiller W, Margraf J: Cognitive aspects of hypochondriasis and the somatization syndrome. J Abnorm Psychol 1998; 107:587–595Crossref, Medline, Google Scholar
30. Noyes RJ: Hypochondriasis, in New Oxford Textbook of Psychiatry, vol 2. Edited by Gelder MG, López-Ibor JJ, Andreasen NC. New York, Oxford University Press, 2000, pp 1098–1106Google Scholar
31. Stata Reference Manual: Release 5.0. College Station, Tex, Stata Corp, 1997Google Scholar
32. SPSS 10.0 for Windows 10.0.7, standard version. Chicago, SPSS, 2000Google Scholar
33. Davier VJM: WINMIRA: A Windows 3.x Program for Analysis With the Rasch Model, With Latent Class Analysis, and With the Mixed Rasch Model. Kiel, Germany, Institute for Science Education (IPN), 1994Google Scholar
34. Muthén LK, Muthén BO: Mplus: The Comprehensive Modeling Program for Applied Researchers—User’s Guide 1.0. Los Angeles, Muthén & Muthén, 2000Google Scholar
35. Dunn G, Pickles A, Tansella M, Vazquez-Barquero JL: Two-phase epidemiological surveys in psychiatric research. Br J Psychiatry 1999; 174:95–100Crossref, Medline, Google Scholar
36. Robins E, Guze SB: Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry 1970; 126:983–987Link, Google Scholar
37. Kendell RE: Clinical validity. Psychol Med 1989; 19:45–55Crossref, Medline, Google Scholar
38. Barsky AJ: Patients who amplify bodily sensations. Ann Intern Med 1979; 91:63–70Crossref, Medline, Google Scholar
39. Barsky AJ, Wyshak G, Klerman GL: The somatosensory amplification scale and its relationship to hypochondriasis. J Psychiatr Res 1990; 24:323–334Crossref, Medline, Google Scholar
40. Kenyon FE: Hypochondriacal states. Br J Psychiatry 1976; 129:1–14Crossref, Medline, Google Scholar
41. Sims A: Disorder of the awareness of the body, in Symptoms in the Mind: An Introduction to Descriptive Psychopathology. London, Baillière Tindall, 1988, pp 171–196Google Scholar
42. Noyes R Jr, Kathol RG, Fisher MM, Phillips BM, Suelzer MT, Woodman CL: Psychiatric comorbidity among patients with hypochondriasis. Gen Hosp Psychiatry 1994; 16:78–87Crossref, Medline, Google Scholar
43. Barsky AJ, Wyshak G, Klerman GL: Psychiatric comorbidity in DSM-III-R hypochondriasis. Arch Gen Psychiatry 1992; 49:101–108Crossref, Medline, Google Scholar
44. Barsky AJ, Wyshak G, Klerman GL, Latham KS: The prevalence of hypochondriasis in medical outpatients. Soc Psychiatry Psychiatr Epidemiol 1990; 25:89–94Medline, Google Scholar
45. Barsky AJ, Frank CB, Cleary PD, Wyshak G, Klerman GL: The relation between hypochondriasis and age. Am J Psychiatry 1991; 148:923–928Link, Google Scholar



