Improving Access to Geriatric Mental Health Services: A Randomized Trial Comparing Treatment Engagement With Integrated Versus Enhanced Referral Care for Depression, Anxiety, and At-Risk Alcohol Use
Abstract
OBJECTIVE: The authors sought to determine whether integrated mental health services or enhanced referral to specialty mental health clinics results in greater engagement in mental health/substance abuse services by older primary care patients. METHOD: This multisite randomized trial included 10 sites consisting of primary care and specialty mental health/substance abuse clinics. Primary care patients 65 years old or older (N=24,930) were screened. The final study group consisted of 2,022 patients (mean age=73.5 years; 26% female; 48% ethnic minority) with depression (N=1,390), anxiety (N=70), at-risk alcohol use (N=414), or dual diagnosis (N=148) who were randomly assigned to integrated care (mental health and substance abuse providers co-located in primary care; N=999) or enhanced referral to specialty mental health/substance abuse clinics (i.e., facilitated scheduling, transportation, payment; N=1,023). RESULTS: Seventy-one percent of patients engaged in treatment in the integrated model compared with 49% in the enhanced referral model. Integrated care was associated with more mental health and substance abuse visits per patient (mean=3.04) relative to enhanced referral (mean=1.91). Overall, greater engagement was predicted by integrated care and higher mental distress. For depression, greater engagement was predicted by integrated care and more severe depression. For at-risk alcohol users, greater engagement was predicted by integrated care and more severe problem drinking. For all conditions, greater engagement was associated with closer proximity of mental health/substance abuse services to primary care. CONCLUSIONS: Older primary care patients are more likely to accept collaborative mental health treatment within primary care than in mental health/substance abuse clinics. These results suggest that integrated service arrangements improve access to mental health and substance abuse services for older adults who underuse these services.
Despite poor health outcomes and increased health care costs associated with psychiatric disorders in older adults (1, 2), mental health services are underutilized, and access to assessment and treatment by specialty mental health providers is poor (3, 4). Fewer than 3% of older adults report seeing a mental health professional for treatment, a rate lower than that of any other adult age group (5). Instead, older adults tend to seek mental health treatment in primary care, a system stressed by the demands of complex medical disorders and severe time constraints (6). One approach to overcoming barriers to mental health consultation and treatment services involves improving the system of referral to specialty mental health clinics. Enhancements include selecting mental health clinics with services tailored to older persons, providing transportation and third-party payment coverage, and minimizing time from referral to visit with the specialty mental health provider (4, 7, 8). An alternative approach consists of improving access through co-location of services and collaboration between mental health and primary care providers (9). Integrated, collaborative care management has been shown to improve outcomes for older adults with depression relative to usual care by the primary care provider (10).
However, no study has compared an integrated mental health/substance abuse services model to that of enhanced referral to specialty mental health/substance abuse clinics in improving access for older adults. Furthermore, no study has evaluated treatment engagement in these competing models for a broader array of common disorders, including depression, anxiety disorders, and at-risk alcohol use. This article reports the initial results of the Primary Care Research in Substance Abuse and Mental Health for the Elderly study, a randomized clinical trial comparing an enhanced referral model with integrated mental health/substance abuse services in primary care. Specific questions addressed include the following:
| 1. | Which service delivery model results in greater engagement in mental health/substance abuse services by older primary care patients with depression, anxiety disorders, or at-risk alcohol use? | ||||
| 2. | Are specific demographic characteristics, diagnoses, or severity of symptoms associated with greater engagement in either model? | ||||
Method
The study was a multisite randomized trial comparing integrated and enhanced referral models of mental health care for older persons with depression, anxiety, or at-risk alcohol consumption. The integrated model provided mental health/substance abuse services in the primary care clinic by a mental health provider. The enhanced referral model provided mental health/substance abuse services in a specialty setting that was physically separate and designated as a mental health/substance abuse clinic. A comprehensive account of the study methods is provided in a companion paper (11).
Subjects
A total of 24,930 primary care patients age 65 and older were screened for a mental health disorder or at-risk drinking between March 2000 and October 2001 (Figure 1). A positive screen was defined as significant psychological distress on the General Health Questionnaire (12), a positive response to suicidal ideation questions modified from the PRIME-MD (13), or at-risk alcohol consumption based on quantity/frequency criteria (14) of more than seven drinks/week or more than two binge episodes in the past 3 months consisting of more than three drinks on a single occasion. Primary care providers also directly referred 776 patients to the study, representing 3.1% of the total sample screened.
Patients who had received mental health/substance abuse treatment in the preceding 3 months and patients with severe cognitive impairment (≥16 on the Brief Orientation Memory Concentration Test [15]) were excluded. Primary care providers were given the opportunity to withdraw patients with positive screens for medical reasons; this occurred in fewer than 1% of patients eligible for baseline assessment. In the first stage of screening, incomplete data or cognitive impairment eliminated 1,102 patients, and 17,398 had negative screen results. Of the remaining 6,430 patients with positive screens, 3,225 elected not to proceed to a baseline assessment interview. Compared with those who consented, those who refused baseline assessment were more likely to be male (84.9% versus 74.7%) (χ2=105.8, df=1, p<0.001) and Caucasian (72.2% versus 60.3%) (χ2=104.9, df=1, p<0.001); have a lower mean General Health Questionnaire score (mean=3.5 [SD=3.1] versus 4.3 [SD=3.1]) (z=11.2, p<0.001), indicating less severe distress; and more reported drinks per week (mean=6.0 [SD=11.5] versus 5.1 [SD=9.8]) (z=–3.27, p=0.001).
Following the first stage of screening, 3,205 patients completed the baseline assessment for depression, anxiety, and at-risk drinking target conditions to determine eligibility for the study. Presence of target conditions was assessed by using the Mini-International Neuropsychiatric Interview (16), Center for Epidemiological Studies Depression Scale (CES-D Scale) (17), Beck Anxiety Inventory (18), an alcohol quantity/frequency scale, and a detailed medication review. Additional assessments included demographic data, the Paykel Suicide Scale (19), the Short Michigan Alcohol Screening Test—Geriatric Version (20), and the Medical Outcomes Study 36-Item Short Form (21). Patients with a positive assessment on the Mini-International Neuropsychiatric Interview for psychosis, mania, or hypomania were excluded (N=73). Patients with incomplete data (N=118) or no target diagnosis (N=992) were also excluded.
The final study group comprised 2,022 patients who met criteria, gave written informed consent after study procedures were fully explained, and were randomly assigned to receive integrated care (N=999) or enhanced referral care (N=1,023). Patients were recruited from five Department of Veterans Affairs medical centers (N=1,220 [60.3%]), three community health centers (N=535 [26.5%]), and two outpatient hospital networks (N=267 [13.2%]).
There were no significant differences in demographic characteristics between patients randomly assigned to the integrated condition and those assigned to the referral condition. Mean age of the sample was 73.5 years (SD=6.2), and almost three-quarters (N=1,498 [74.1%]) were male. Nearly half of the sample was married (N=972 [48%]), two-fifths had completed less than 12 years of schooling (N=875 [43%]), and one-fifth had limited finances as defined by “difficulty in making ends meet” (N=415 [21%]). Participants had an average of 2.8 close friends and relatives (SD=1.20). Slightly over half of the sample was Caucasian (52.0%); the next most frequent racial group was African American (24.8%), followed by Hispanic Latino (14.8%), Asian (5.6%), and other (2.9%).
There were no between-group differences in medical or psychiatric severity as assessed with the Medical Outcomes Study 36-Item Short Form, CES-D Scale, Beck Anxiety Inventory, drinks per week, or comorbid psychiatric or medical diagnoses. On average, the sample had a mean of 4.7 chronic diseases (SD=2.5) and had substantial physical and mental distress as measured by the Medical Outcomes Study 36-Item Short Form (mean=39.3 [SD=10.6] and 41.9 [SD=12.9], respectively). Over two-thirds of the sample had a primary mental health diagnosis of depression (N=1,390 [69%]), one-fifth met criteria for at-risk drinking (N=414 [20%]), and the remainder were in the dual diagnosis (N=148 [7%]) or anxiety disorder (N=70 [3%]) groups. The diagnostic breakdown of the depression group was major depression (42.5%, N=591), minor depression (17.9%, N=249), dysthymia (5.5%, N=77), depression not otherwise specified (6.1%, N=85), and depression co-occurring with anxiety (27.9%, N=388). The anxiety disorders group consisted of patients with generalized anxiety disorder (75.7%, N=53), anxiety not otherwise specified (18.6%, N=13), and panic disorder (5.7%, N=4). Finally, the dual diagnosis group comprised patients with depression and at-risk drinking (64.2%, N=95); depression, anxiety, and at-risk drinking (29.7%, N=44); and anxiety and at-risk drinking (6.1%, N=9).
Study Intervention
Integrated models met the following minimum criteria for site eligibility: 1) mental health and substance abuse services co-located in the primary care setting (including assessment, care planning, counseling, case management, psychotherapy, and pharmacological treatment), with no distinction in terms of signage or clinic names; 2) mental health and substance abuse services provided by licensed mental health/substance abuse providers (including social workers, psychologists, psychiatric nurses, psychiatrists, and master’s-level counselors); 3) verbal or written communication about the clinical evaluation and treatment plan between the mental health and substance abuse clinician and primary care provider; and 4) an appointment with the mental health and substance abuse provider within 2 to 4 weeks following the primary care provider visit. Patients with at-risk drinking were offered a manualized Brief Alcohol Intervention (22).
The minimum criteria for the enhanced referral model included 1) referral within 2 to 4 weeks of the primary care provider appointment; 2) treatment offered in a separate location by licensed mental health and substance abuse professionals; 3) agreement by the specialty mental health/substance abuse clinics to comply with model requirements, including time to first appointment and coordinated follow-up contacts if the patient failed to make the first scheduled visit; 4) assistance with transportation; and 5) facilitated direct or third-party coverage for the costs of the specialty mental health and substance abuse visit.
As anticipated, the profile of providers differed in the two models. Of the patients in the integrated model with at least one treatment visit, approximately three-fifths (60.1% [N=426]) received care from nonphysician mental health clinicians (psychologist, psychiatric social worker, psychiatric nurse, or other nonphysician provider); 35.3% (N=250) received care from a psychiatrist only or psychiatrist with a mental health clinician; and 4.2% (N=30) were treated by a primary care physician alone or primary care physician with a mental health clinician. In contrast, of the patients in the referral model with at least one treatment visit, approximately three-fifths (59.9% [N=299]) received care from a psychiatrist only or psychiatrist with a mental health clinician; 36.7% (N=183) received care from nonphysician mental health clinicians; and 3.4% (N=17) were treated by a primary care physician alone or primary care physician with a mental health clinician (χ2=71.48, df=2, p<0.001). For patients in the integrated and referral groups who received treatment following an initial evaluation (N=550 and 314, respectively), there were also modest differences in the type of treatment provided: psychotherapy only (51.6% versus 39.2%), medication management only (20.7% versus 18.2%), medication management combined with psychotherapy (21.1% versus 36.3%), and case management/evaluation (6.6% versus 6.4%) (χ2=24.65, df=3, p<0.001).
All patients were given an appointment with a mental health and substance abuse provider. The primary care physician was informed of the appointment and encouraged to support the referral. Both models were required to be in place and functioning for at least 6 months prior to patient enrollment to ensure full implementation. Model fidelity and satisfaction of minimum requirements were confirmed by the study coordinating center before randomization and systematically monitored through a detailed process evaluation for each site and through site visits.
Outcome
The dependent variable of treatment engagement was defined as attendance at an appointment with a mental health/substance abuse provider following randomization at the index primary care visit. For every mental health/substance abuse encounter, a check-off treatment tracking form was completed by the clinician or by research assistants by medical record review over the 6-month period of study follow-up. The coordinating center cross-checked data from the treatment tracking form and study completion form and resolved any discrepancies with site data coordinators.
Analyses
Rates of treatment engagement, overall, by site and by key diagnostic and demographic factors were examined by cross-tabulation and computation of odds ratios, based on an intent-to-treat analysis. Multiple logistic regression was used to examine treatment assignment and diagnostic severity as predictors of engagement. Because study populations and treatment models varied somewhat among study sites, a likelihood ratio test for treatment-by-site interaction was performed; site was controlled in all models.
Results
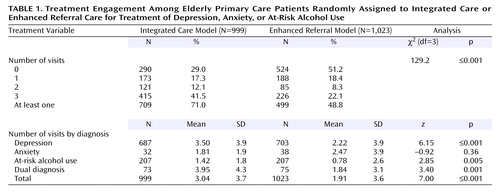
We found a greater rate of treatment engagement among patients randomly assigned to the integrated model (71.0%) than among those assigned to enhanced referral (48.8%), amounting to a 22.2% difference between the two models (odds ratio=2.57, 95% CI=2.14–3.08) (Table 1). Both models had similar proportions of patients with only one mental health/substance abuse visit. However, integrated care patients were more likely to return for subsequent treatment visits: 53.6% had two or more visits compared with 30.4% for the enhanced referral group (χ2=112.27, df=1, p<0.001). Overall, the integrated model was also associated with a greater mean number of visits (3.04) compared with the referral model (1.91) (Table 1). The integrated model was associated with a significantly greater number of visits for depression, at-risk alcohol use, and dual diagnosis but not for anxiety disorders.
Figure 2 displays rates of treatment engagement associated with the physical proximity of mental health/substance abuse services to primary care. Rates of engagement progressively decreased with greater distance between primary care and mental health/substance abuse services for the total sample (χ2=103.15, df=3, p<0.001) and also among the subset of enhanced referral sites (χ2=7.76, df=2, p=0.02). The lowest rate of engagement (44.2%) was found for patients referred for mental health/substance abuse services located 1–10 miles from primary care.
The integrated and referral models also differed with respect to time between the primary care physician appointment and time to the first mental health/substance abuse visit attended by the patient. The integrated model was associated with a greater proportion of first visits occurring 0–14 days from randomization (37.4%) compared with enhanced referral (15.4%) (χ2=126.09, df=1, p<0.001). The proportion of patients with a first visit within 2–4 weeks of the primary care visit was similar in the integrated model (13.3%) and the referral model (11.8%). Likewise, the proportion of patients with a first visit beyond the 4-week target window was similar for patients in the integrated model (19.8%) and the referral model (21.5%).
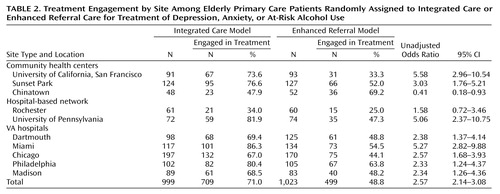
Rates of treatment engagement for each of the 10 study sites are shown in Table 2. Rates of engagement were greater for integrated care in nine of the 10 study sites, with rates ranging up to two times greater than those with enhanced referral. However, in one site (Chinatown), the rate of engagement was greater in the referral model. A test for site-by-treatment interaction was statistically significant (G2=34.07, df=9, p<0.001). When the Chinatown data were set aside, the test for site-by-treatment interaction was no longer statistically significant (G2=12.70, df=8, p=0.15). Thus, we elected to base subsequent analyses of patient-level characteristics predictive of engagement on the data from the nine sites with consistent results. Similar results were obtained in analyses of all 10 sites.
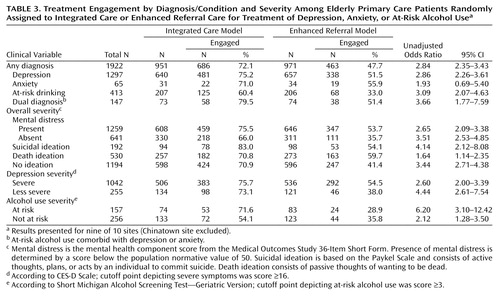
Table 3 shows rates of engagement by diagnostic category and for subgroups defined by symptom severity. All diagnostic groups achieved higher rates of engagement in the integrated model. Over three-quarters (75.2%) of patients with depression engaged in mental health/substance abuse services in the integrated model compared with approximately one-half (51.5%) in the enhanced referral model. Patients with at-risk drinking were nearly twice as likely to engage in the integrated model (60.4%) relative to enhanced referral (33.0%). Among patients with depression, those with more severe symptoms engaged in care more frequently (64.8%) than did those with less severe symptoms (56.5%). However, the differential rate of engagement between the integrated and referral models was greatest for individuals with milder depression. The largest differential effect for patients in the at-risk drinking category was found in those with problem drinking, who were approximately two-and-a-half times more likely to engage in the integrated model (71.6%) relative to referral care (28.9%). Of note, 83.0% of individuals with active suicidal ideation engaged in mental health/substance abuse treatment in the integrated model compared with 54.1% in the enhanced referral model. Rates of engagement were greater for integrated care for all demographic subgroups, as defined by gender, age, ethnicity, marital status, living status, education, and employment status. There were no demographic differences in overall rate of engagement.
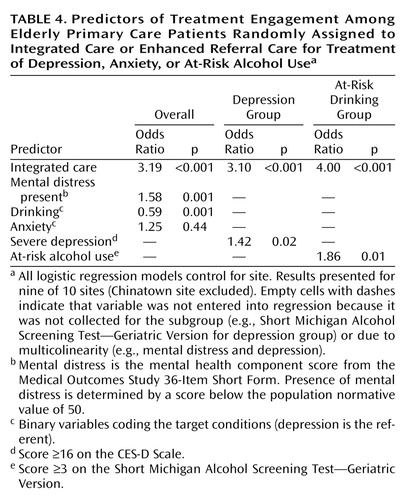
Logistic regression models identifying predictors of engagement are shown in Table 4. Three models are presented, one for all patients combined, another for patients with depression, and another for those with at-risk drinking. For the overall group, assignment to the integrated care model was strongly associated with a greater likelihood of treatment engagement after we controlled for symptom severity. More severe mental distress was also an independent predictor of engagement. The full sample regression model allowed for a comparison of diagnostic groups. Overall, at-risk alcohol users were less likely to engage in care than depression patients. However, a regression model limited to the subgroup with at-risk drinking found two independent factors predictive of engagement: integrated care and more severe problem drinking as measured by the Short Michigan Alcohol Screening Test—Geriatric Version. Among the subgroup with depression, greater engagement was predicted by assignment to the integrated model and by more severe depression as measured by the CES-D Scale. Demographic variables and medical severity were not associated with treatment engagement and thus were not included in regression models.
Additional regression analyses were conducted examining specific interactions of treatment model with diagnosis for the regression including the total patient sample, and separately for the interaction of treatment model with symptom severity for the depression and at-risk alcohol use subgroups. The only interaction approaching significance was between problem drinking severity (Short Michigan Alcohol Screening Test—Geriatric Version) and model assignment (likelihood ratio test: χ2=3.6, p=0.07). Although bivariate analyses indicated that individuals with less severe depression symptoms were less likely to engage in referral care, this interaction was not significant in the multivariate model.
Discussion
This study shows that integrated mental health/substance abuse services in primary care settings result in substantially greater treatment engagement by older patients compared with referral to specialty mental health/substance abuse clinics under enhanced conditions. Despite enhancing the system of referral by ensuring timely appointments, transportation, and payment for services, less than half (49%) of older persons engaged in services in the enhanced referral model compared with over two-thirds of patients (71%) engaging in the integrated model. Superior rates of engagement in the integrated model were found in nine of 10 sites despite significant differences across sites with respect to organization, financing, practice setting, and patient ethnicity. Separate service delivery systems for mental health and general health care have been cited as a major barrier to mental health care for older persons (7). Integrated care has been advocated as a means to enhance communication between providers, reduce stigma and medical expenditures, and avoid artificial separation of medical and psychiatric problems that can result in substandard care (23).
Differential rates of engagement between integrated and enhanced referral models were largely explained by the proportions of patients with two or more mental health/substance abuse visits, underscoring that differences in engagement were associated with substantive care episodes rather than single clinical contacts. In addition, patients assigned to integrated care were more likely to have first appointments within 2 weeks of the primary care visit, demonstrating enhanced access to timely treatment.
An important finding relates to the role of physical proximity of mental health/substance abuse services to primary care in predicting treatment engagement. Greater distance between primary care and mental health/substance abuse services was associated with declining rates of engagement. This relationship was found for the total study sample, including the integrated model in which physical proximity of mental health/substance abuse services in the primary care setting was an attribute of the model. In addition, greater distance was associated with lower rates of engagement when only considering the subgroup of patients in the referral model, in which there was a range of distances between mental health/substance abuse services and the primary care setting. Of note, the one site with greater rates of engagement in the referral model (Chinatown) provided mental health/substance abuse services in the same building as the primary care clinic and had a 30-year relationship of working together in a well-functioning arrangement of receiving and coordinating referrals. Hence, a small distance between mental health and primary care clinics and established patterns of coordination may have favored engagement in the referral model at the Chinatown site. Overall, these findings suggest that integration of mental health and primary health care may be most accurately described along a multidimensional continuum, rather than a dichotomy. In this respect, integration might be appropriately characterized along different dimensions such as the degree of physical proximity, temporal proximity, communication between providers, collaboration in treatment planning, range of available mental health services, and degree of common financing and billing for mental health and medical care.
Logistic regression modeling identified both patient-level and service model factors associated with engagement. For the overall sample, older primary care patients who were more distressed and who did not have at-risk alcohol use were more likely to engage in mental health and substance abuse services. However, among older adults in the at-risk alcohol use subgroup, greater engagement was associated with a higher degree of alcohol-associated problems. Finally, within the depression subgroup, greater engagement was independently associated with more severe depression. Overall, integrated services were the most important determinant of engagement in care for each diagnostic group, suggesting that the model of service delivery is a crucial determinant of use of mental health/substance abuse services by older primary care patients.
Of interest, the integrated model was particularly beneficial in engaging individuals with at-risk alcohol use. The largest difference in rates of engagement was found among those with greater severity of problem drinking. This finding is underscored by a tendency toward a model-by-diagnosis interaction. This suggests that older adults with at-risk alcohol use may be more likely to follow-through with brief alcohol assessment and treatment with a provider who is integrated into the primary care setting than with a referral to a specialty clinic.
A surprisingly high rate of engagement was also found in the integrated model for older adults with active suicidal ideation (83%). Epidemiological studies indicate that older adults have the highest rate of suicide among any age group (24), and 70% of older persons visit their primary care physician within a month of committing suicide (25). These findings suggest that integrated care may be effective in engaging older primary care patients who are at-risk for suicide.
Several caveats are indicated in interpreting the results of this study. First, study participants were limited to those who consented to random assignment; therefore rates of engagement do not necessarily generalize to the entire population of older primary care patients. An analysis of screening data found that individuals who declined participation were more likely to be male and Caucasian, had less severe General Health Questionnaire scores, and had greater alcohol use. At the same time, generalization of the study findings is substantially enhanced by the inclusion of a large, ethnically diverse sample of older adults from a wide range of practice settings. Second, this report compares rates of engagement between treatment models but does not address clinical outcomes associated with these models. Finally, rates of engagement were compared between integrated care and an enhanced system of referral care. Hence, it is likely that our study underestimates the difference in engagement between integrated care and routine systems of referral care that do not include enhancements such as timely appointments, assistance with transportation, and facilitated coverage for the costs of the specialty mental health and substance abuse visit.
Results from this study confirm that older primary care patients are more likely to accept collaborative mental health treatment within primary care settings than in mental health and substance abuse specialty clinics. As older adults have the lowest use of mental health and substance abuse services compared with any other adult age group, this study provides empirical support for health policy reform recommendations aimed at improving access to coordinated psychiatric and medical services by fostering integrative relationships between mental health and primary care sectors (26).
Acknowledgments
The Primary Care Research in Substance Abuse and Mental Health for the Elderly study was conducted with the participation of the following investigators (in alphabetical order): C. Aoyama, P. Arean, S. Bartels, H. Chen, H. Chung, M. Cody, S. Cooley, G. Costantino, U.N.B. Durai, C. Estes, J. Fitzpatrick, B. Goodman, T. Hadley, B. McDonel Herr, T. Howell, I. Katz, J. Kirchner, D. Krahn, S. Levkoff, K. Linkins, M. Llorente, J. Maxwell, J. McIntyre, K. Miles, R. Molokie, M. Nazar, E. Olsen, D. Oslin, T. Oxman, A. Pomerantz, L. Quijano, H. Syropoulos, W. Van Stone, P. Wohlford, C. Zubritsky.
 |
 |
 |
 |
Presented in part at the 16th annual meeting of the American Association for Geriatric Psychiatry, Honolulu, March 1–4, 2003. Received July 15, 2003; revision received Oct. 28, 2003; accepted Oct. 31, 2003. From the Department of Psychiatry, Dartmouth Medical School, Lebanon, N.H.; John Snow, Inc., Boston, Mass.; the Department of Psychiatry, University of Pennsylvania, Philadelphia; Harvard School of Public Health, Boston, Mass.; the Department of Psychiatry, University of California, San Francisco; the Department of Psychiatry, Harvard Medical School, Boston, Mass.; the Philadelphia VA Medical Center, Philadelphia, Pa.; Miami VA Medical Center—Geriatric Research, Education and Clinical Center, Miami, Fla.; University of Miami School of Medicine, Miami Beach, Fla.; Lutheran Medical Center Sunset Park Family Health Center Network, Brooklyn, N.Y.; Baylor College of Medicine, Baylor, Tex.; the Department of Psychiatry and Behavioral Health, Unity Health System, Rochester, N.Y.; and The Lewin Group, Falls Church, Va. Address reprint requests to Dr. Bartels, New Hampshire-Dartmouth Psychiatric Research Center, 2 Whippleplace, Suite 202, Lebanon, NH 03766; [email protected] (e-mail). This initiative was funded by the federal Substance Abuse and Mental Health Services Administration (SAMHSA). SAMHSA has three centers: the Center for Mental Health Services, the Center for Substance Abuse Treatment, and the Center for Substance Abuse Prevention. All three centers were involved in this project, with the Center for Mental Health Services serving as the lead. The Department of Veterans Affairs, the Health Resources Services Administration, and the Centers for Medicare and Medicaid Services provided additional support and collaboration. The authors thank Aricca Dums Van Citters, B.A., for her help in manuscript preparation. This article was written solely from the perspective of the authors and does not necessarily represent the official policy or position of the U.S. Substance Abuse and Mental Health Services Administration, the U.S. Department of Veterans Affairs, the Health Resources Services Administration, the U.S. Department of Health and Human Services, or the federal government.
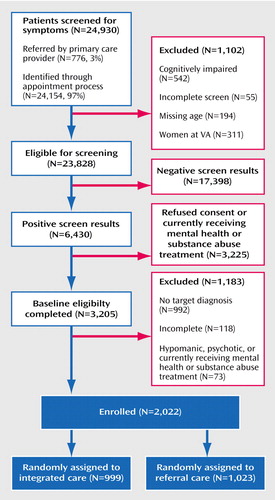
Figure 1. Participant Progression Through the Primary Care Research in Substance Abuse and Mental Health for the Elderly Study
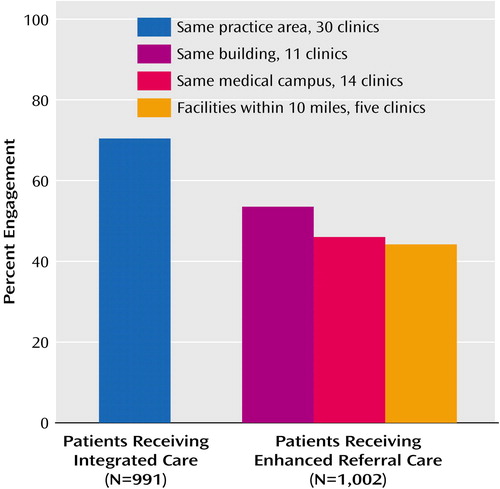
Figure 2. Treatment Engagement by Physical Proximity Between Primary Care and Mental Health/Substance Abuse Clinicsa
aGroup sizes differ slightly from the total because clinic data are missing on 29 patients.
1. Druss BG, Rohrbaugh RM, Rosenheck RA: Depressive symptoms and health costs in older medical patients. Am J Psychiatry 1999; 156:477–479Abstract, Google Scholar
2. Unützer J, Patrick DL, Simon G, Grembowski D, Walker E, Rutter C, Katon W: Depressive symptoms and the cost of health services in HMO patients aged 65 years and older. JAMA 1997; 277:1618–1623Crossref, Medline, Google Scholar
3. Bartels SJ, Horn S, Sharkey P, Levine K: Treatment of depression in older primary care patients in health maintenance organizations. Int J Psychiatry Med 1997; 27:215–231Crossref, Medline, Google Scholar
4. Mental Health: A Report of the Surgeon General. Rockville, Md, US Department of Health and Human Services, 1999Google Scholar
5. Olfson M, Pincus HA: Outpatient mental health care in nonhospital settings: distribution of patients across provider groups. Am J Psychiatry 1996; 153:1353–1356Link, Google Scholar
6. Kaplan MS, Adamek ME, Calderon A: Managing depressed and suicidal geriatric patients: differences among primary care physicians. Gerontologist 1999; 39:417–425Crossref, Medline, Google Scholar
7. Older Adults and Mental Health: Issues and Opportunities. Rockville, Md, US Administration on Aging, 2001Google Scholar
8. Grunebaum M, Luber P, Callahan M, Leon AC, Olfson M, Portera L: Predictors of missed appointments for psychiatric consultations in a primary care clinic. Psychiatr Serv 1996; 47:848–852Link, Google Scholar
9. Katon W, Von Korff M, Lin E, Simon G, Walker E, Bush T, Ludman E: Collaborative management to achieve depression treatment guidelines. J Clin Psychiatry 1997; 58(suppl 1):20–23Google Scholar
10. Unützer J, Katon W, Callahan CM, Williams JW, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Hitchcock Noël P, Lin EHB, Areán PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C: Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002; 288:2836–2845Crossref, Medline, Google Scholar
11. Levkoff S, Chen H, Coakley E, McDonel Herr B, Oslin DW, Katz I, Bartels S, Maxwell J, Olsen E, Miles KM, Costantino G, Ware JH: Design and sample characteristics of the PRISM-E multisite randomized trial to improve behavioral health care for the elderly. J Aging Health 2004; 16:3–27Crossref, Medline, Google Scholar
12. Goldberg D: General Health Questionnaire (GHQ-12). Windsor, UK, National Foundation for Educational Research-Nelson, 1992Google Scholar
13. Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV III, Hahn SR, Brody D, Johnson JG: Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA 1994; 272:1749–1756Crossref, Medline, Google Scholar
14. Sobell LC, Sobell MB, Leo GI, Cancilla A: Reliability of a timeline method: assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. Br J Addict 1988; 83:393–402Crossref, Medline, Google Scholar
15. Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H: Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry 1983; 140:734–739Link, Google Scholar
16. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC: The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59(suppl 20):22–33Google Scholar
17. Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. J Applied Psychol Measurement 1977; 1:385–401Crossref, Google Scholar
18. Beck AT, Epstein N, Brown G, Steer RA: An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988; 56:893–897Crossref, Medline, Google Scholar
19. Paykel ES, Myers JK, Lindenthal JJ, Tanner J: Suicidal feelings in the general population: a prevalence study. Br J Psychiatry 1974; 124:460–469Crossref, Medline, Google Scholar
20. Blow FC: Short Michigan Alcoholism Screening Test—Geriatric Version (SMAST-G). Ann Arbor, University of Michigan Alcohol Research Center, 1991Google Scholar
21. Ware JE Jr, Sherbourne CD: The MOS 36-Item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care 1992; 30:473–483Crossref, Medline, Google Scholar
22. Barry KL, Oslin DW, Blow FC: Prevention and Management of Alcohol Problems in Older Adults. New York, Springer, 2001Google Scholar
23. Mechanic D: Approaches for coordinating primary and specialty care for persons with mental illness. Gen Hosp Psychiatry 1997; 19:395–402Crossref, Medline, Google Scholar
24. Hoyert DL, Kochanke KD, Murphy SL: Deaths: Final data for 1997, in National Vital Statistics Reports: DHHS Publication 99–1120. Hyattsville, Md, National Center for Health Statistics, 1999Google Scholar
25. Conwell Y: Suicide in elderly patients, in Diagnosis and Treatment of Depression in Late Life. Edited by Schneider LS, Reynolds CFI, Lebowitz BD, Friedhoff AJ. Washington, DC, American Psychiatric Press, 1994, pp 397–418Google Scholar
26. Bartels SJ: Improving the United States’ system of care for older adults with mental illness: findings and recommendations for the President’s New Freedom Commission on Mental Health. Am J Geriatr Psychiatry 2003; 11:486–497Crossref, Medline, Google Scholar



