Racial Differences in Paranoid Ideation and Psychoses in an Older Urban Population
Abstract
OBJECTIVE: This study examined whether there are racial differences in the prevalence of paranoid ideation and psychotic symptoms in persons age ≥55 in an urban community. METHOD: Using 1990 census data for Brooklyn, N.Y., the authors attempted to interview all cognitively intact persons age ≥55 in randomly selected blocks. The final group consisted of 206 whites and 821 blacks. The authors used George’s Social Antecedent Model for analyzing 21 independent and three dependent variables: paranoid ideation, psychotic symptoms, and psychotic symptoms/paranoid ideation. The group was weighted by race and gender. To control for intrablock clustering effects without replacement sampling, the authors used SUDAAN for data analysis. RESULTS: A significant difference in psychotic symptoms or paranoid ideation was found between blacks and whites (24% versus 10%) that was attenuated but not eliminated with logistic regression analyses. Blacks with psychotic symptoms or paranoid ideation, especially Caribbeans, had significantly lower receipt of mental health services and lower perceived service needs. With logistic regression, psychotic symptoms and paranoid ideation were associated with four variables among blacks and whites, although only one was significant in both groups. CONCLUSIONS: Racial differences in psychotic symptoms and paranoid ideation persist even after control for various clinical, social, and attitudinal effects. Among blacks, response to stressors may be expressed through increased paranoid ideation and psychotic symptoms. Stronger beliefs in spiritualism increase this expression in both races. The high prevalence of psychotic symptoms or paranoid ideation among this aging urban population, especially blacks, highlights a potential public health issue.
Despite evidence that the prevalence of psychotic symptoms and paranoid ideation in older community-dwelling adults is not uncommon—i.e., rates of up to 10% have been reported, depending on sample characteristics and selection criteria (1–6)—data in the United States have been limited to three studies in the past 20 years, all of which focused exclusively on paranoid ideation (4–6). Two were general community studies conducted in rural and urban areas in North Carolina (4, 5), and the third involved a sample of African Americans recruited from senior centers in New Orleans (6). This paucity of data is unfortunate since psychotic and paranoid symptoms in older persons without cognitive impairment have been linked to the development of dementia, higher mortality, impaired functional ability, depression, visual and hearing impairments, and poor physical health (1–6).
In the United States, among all age groups, racial differences in paranoid symptoms have been noted, with blacks having a significantly greater prevalence than whites (7). This finding takes on added clinical importance because older blacks are among the most rapidly expanding population subgroups. Moreover, the older black population, particularly in urban areas, has become more diverse as a result of immigration from the Caribbean, i.e., the number of Caribbeans nationwide is estimated to be over two million (8). Hence, factors that influence symptom prevalence among urban blacks may be different from factors reported in other geographic areas. Indeed, Blazer and colleagues (5) speculated that paranoid symptoms in older blacks might represent an appropriate response to a hostile environment rather than a psychopathic trait. However, their study did not separately examine older blacks, which might have clarified whether different elements played a role in the etiology of their symptoms. In the study of elderly African Americans in New Orleans (6), the sample was derived from senior centers, so it is unclear how representative the findings were of older blacks in general. Moreover, the authors did not indicate whether African Caribbeans were included in their sample. Thus, there are compelling reasons to examine psychotic and paranoid symptoms in other geographic regions of the United States that include a culturally diverse group of older black adults.
In order to examine the factors that predict psychoses and paranoid ideation in aging persons, we employed a modified version of George’s social antecedent model of psychiatric disorders in older adults (9). She postulated six stages of risk factors, with later stages hypothesized to be increasingly proximate precursors of psychiatric disorders. The first three stages consist of demographic factors (e.g., race, gender, and ethnicity), early events and achievements (e.g., education and early traumatic events), and later events and achievements (e.g., financial status, later traumatic events). The fourth and fifth stages consist of social integration and support and various vulnerability factors (e.g., chronic stressors such as physical illness, alcoholism, and mental distress). The sixth stage consists of provoking agents (e.g., acute life events) and coping strategies (e.g., beliefs and behaviors). Thus, the model has the potential to test the concurrent effects of social and clinical variables.
With this model, we addressed two questions:
| 1. | With control for other variables in the model, are there any racial differences in the prevalence of paranoid ideation and psychotic symptoms in a community sample of persons ages 55 and over? | ||||
| 2. | Are there any differences between the older black and older white groups in the factors associated with paranoid ideation and psychotic symptoms? | ||||
Method
Sample
With the Wessex Census Summary Tape File 3 for Kings County (Brooklyn, N.Y.), we extracted black and white persons 55 years of age and over. To conserve costs, block groups that had fewer than 10% blacks or 10% whites were eliminated from the black and white files, respectively. We randomly selected, without replacement, block groups as the primary sampling unit.
Based on 1990 census totals, the estimation of approximate populations by race and gender was performed with sampling weights. The sampling weights were computed as the reciprocal of the selection probabilities for each observation. Our study design called for interviewing a minimum of 200 persons in each of four ethnic groups: Caucasians, African Americans, African Caribbeans from English-speaking islands, and African Caribbeans from French-speaking islands. Data collection took place from 1996 to 1999.
An effort was made to interview all persons in a selected block group by knocking on doors. To enhance response rates, subjects from the selected block group were also recruited at senior centers and churches and through personal references; 30% of the sample was recruited through these means. The overall response rate was 77% of those contacted. Persons with significant cognitive impairment—i.e., scores of 4 or less on the Mental Status Questionnaire (10)—were excluded from the overall study. The final community sample consisted of 878 blacks and 219 Caucasians. However, for the present analyses, we excluded persons with possible dementia, according to the criteria of Zarit et al. (11), i.e., those with scores <8 on the Mental Status Questionnaire. Therefore, the current study included 1,027 persons, 206 Caucasians and 821 blacks, of whom 282 were African Americans, 288 were African Caribbeans from English-speaking islands, 248 were African Caribbeans from French-speaking islands, and three could not be classified. The weighted totals were 429,089 persons, of whom 118,668 were black and 310,421 were Caucasians; the weighted totals by gender were 172,787 men and 256,302 women.
After providing a complete description of the study to the subjects, we obtained written informed consent. The institutional review board of the State University of New York Downstate Medical Center approved the study.
Instruments and Variables
The literature had indicated that psychotic and paranoid symptoms in later life may be associated with physical illness, cognitive deficits, impaired vision and hearing, difficulties in daily functioning, depression, environmental stressors, diminished social support, increased age, gender (male), race (black), and immigrant status (1–6). These findings also suggested that coping strategies and beliefs or attitudinal systems might mediate the effects of some of these factors, although none of the earlier studies had specifically examined these variables. We used a modified version of George’s theoretical model (10) as the scaffolding in which to incorporate the relevant variables previously noted in the literature, along with several additional coping and attitudinal variables that we postulated as being important.
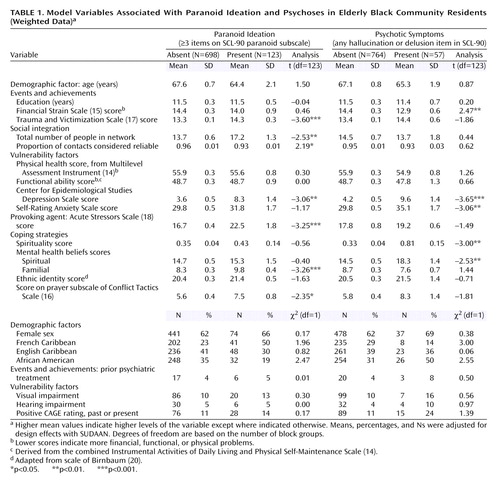
We operationalized 21 dependent and three independent variables (Table 1) that were derived with the following instruments and methods:
| 1. | The Self-Rating Anxiety Scale (12) | ||||
| 2. | The Center for Epidemiological Studies Depression Scale (CES-D Scale) (13) | ||||
| 3. | A physical illness score that represented the sum of seven health care items and 13 illness categories derived from the Multilevel Assessment Inventory Physical Health Status (lower scores indicate worse health) (14) | ||||
| 4. | A functional impairment rating derived from combining the Instrumental Activities of Daily Living and Physical Self-Maintenance Scale (14) (lower scores indicate more impairment) | ||||
| 5. | The Financial Strain Scale (15), for which lower scores denote more strain | ||||
| 6. | The Conflict Tactics Scale (16), which was modified for this study and then subdivided into seven subscales (prayer, calm discussion, keeping feelings inside, hitting, shoving, hurting, or using a weapon) by using principal components analysis with varimax rotation The Trauma and Victimization Scale (17), which examined 18 lifetime traumatic events (e.g., physical abuse, sexual assault, physical assault, and witnessing violence) | ||||
| 7. | The Acute Stressors Scale (18), which examined 11 life events that may have occurred in the past month | ||||
| 8. | The Network Analysis Profile (19), which generated variables concerning network size, intimacy, reliability of contacts, advice giving, and material support | ||||
| 9. | The Ethnic Identity Scale, a seven-item scale adapted from Birnbaum’s scale (20) that examines affinity for one’s ethnic group and perceived prejudice | ||||
| 10. | The CAGE Questionnaire (21), for which a positive item response in the past or present was used as an indicator for possible alcohol problems | ||||
| 11. | The Mental Health Beliefs Scale, a 93-item scale developed using community focus groups, which was divided into six belief subscales about the causes and cure of mental illness (spiritual, religious, stress, family heredity and rearing effects, environmental, empathy or understanding) by using principal components analysis with varimax rotation | ||||
| 12. | The SCL-90 (22) | ||||
With respect to the latter, we used all six items from the paranoid subscale, the four most severe items from the 10-item psychoticism subscale dealing with auditory hallucinations and delusions (e.g., others can control or read one’s thoughts; thoughts are not one’s own), and two supplementary items about visual and olfactory hallucinations. “Spirituality” was assessed by assigning a score of 1 if the respondent saw a spiritualist, purchased items from a religious shop, or believed in casting spells; respondents received a score of 2 if they endorsed at least two of these items. Using items from CES-D Scale, the Self-Rating Anxiety Scale, and supplemental items about suicidality, we determined the level of major depression, based on DSM-IV symptom criteria. We also included items regarding the use of and perceived need for psychiatric services.
The internal consistencies (Cronbach’s alphas) for the scales were the following: Self-Rating Anxiety Scale, 0.95; CES-D Scale, 0.85; functional impairment, 0.72; Financial Strain Scale, 0.88; Conflict Tactics Scale, 0.84; Trauma and Victimization Scale, 0.68; Acute Stressors Scale, 0.77; Mental Health Beliefs Scale, 0.87; Ethnic Identity Scale, 0.68; and the SCL-90 paranoid ideation subscale, 0.70. Alphas above 0.60 are considered acceptable (23).
Three dependent variables were created:
| 1. | Paranoid ideation was considered present if the respondent endorsed three or more items on the paranoid subscale of the SCL-90. We used a conservative cutoff point that was approximately two standard deviations above the mean scale score for psychiatric outpatients in the original report on the SCL-90 by Derogatis and coworkers (22). | ||||
| 2. | Psychotic symptoms were considered present if the respondent endorsed any of the six items dealing with hallucinations or psychotic delusions on the SCL-90 or among the supplementary items. | ||||
| 3. | Psychotic symptoms or paranoid ideation was considered present if the respondent scored positive on either the paranoid ideation or psychotic symptoms variables described. | ||||
For Haitian respondents, the questionnaire was translated into Creole and then back-translated according to the methods described by Flaherty and colleagues (24). Interviewers were trained with audiotapes and videotapes, and they were generally matched to respondents from similar ethnic backgrounds. Interrater reliability with intraclass correlations ranged from 0.86 to 1.00 for the scales in this sample. The interviewers were periodically monitored with audiotapes.
Data Analysis
In order to control for intrablock clustering effects and for “without replacement” sampling, data analysis was performed by using SUDAAN 7.5.4 (25). The unit of analysis was the individual. All analyses were conducted by using sampling weights. Initially, we conducted bivariate analyses to examine the relationship between independent and dependent variables; t tests and chi-square analyses were used for continuous and categorical independent variables, respectively. With respect to the selection of independent variables, for instruments that generated potentially more than one variable, we conducted preliminary t tests and selected one or more variables from the measure that had substantial association (p<0.10) with any of the dependent variables (preliminary analyses not shown). For the final analyses, we included demographic variables such as gender, age, race, and education, as well as ethnicity for the analyses of the black groups, i.e., African American, French African Caribbean, English African Caribbean (note that only the first two ethnic groups were included as dummy variables in logistic regression analyses). Next, each of the dependent variables was examined separately by race by using logistic regression. Because of concerns regarding problems of multicollinearity, we did not enter anxiety symptoms into the logistic regression analyses because of its strong correlation with depressive symptoms (r=0.76). We selected depressive symptoms rather than anxiety symptoms because the variable yielded a more powerful model. Finally, because of the low number of whites reporting psychoses alone (N=9), we did not examine this variable when we looked separately at the white sample, but we examined it in combination with paranoid ideation.
Results
Prevalence of Symptoms and Treatment
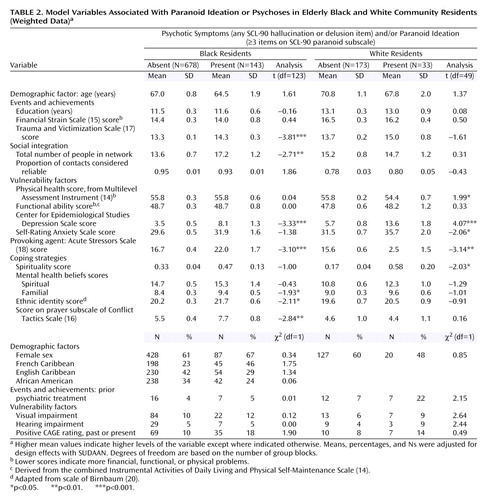
Overall, after adjustment for design effects with the SUDAAN program, 13% of the sample reported paranoid ideation, 3% reported psychotic symptoms, and 14% reported paranoid ideation and/or psychotic symptoms. However, there were substantial racial differences. Blacks were more than twice as likely to experience paranoid ideation (21% versus 9%) (χ2=23.61, df=1, p<0.001), three times more likely to report psychotic symptoms (7% versus 2%) (χ2=17.59, df=1, p<0.001), and twice as likely to experience psychotic symptoms and/or paranoid ideation (24% versus 10%) (χ2=27.27, df=1, p<0.001). Within the black groups, there were appreciable but statistically nonsignificant differences in symptoms (Table 1 and Table 2). Thirteen percent of blacks born in the United States had paranoid ideation, 11% had psychotic symptoms, and 18% had psychotic symptoms and/or paranoid ideation. Thirty-seven percent of black French Caribbeans had paranoid ideation, 4% had psychotic symptoms, and 38% had psychotic symptoms and/or paranoid ideation. Seventeen percent of black English Caribbeans had paranoid ideation, 7% had psychotic symptoms, and 18% had psychotic symptoms and/or paranoid ideation. For the entire sample, when we conducted logistic regression analyses with the independent variables listed in Table 1 (excluding the ethnic subgroups within the black population), we found attenuated but significant racial differences for psychotic symptoms and/or paranoid ideation (χ2=7.09, df=1, p<0.01), paranoid ideation (χ2=5.27, df=1, p<0.05), and psychotic symptoms (χ2=4.94, df=1, p<0.05), although the low number of older whites with psychotic symptoms (N=9) may have distorted the last finding.
The overall percentages that had ever received psychiatric treatment in the past year were 15%, 22%, and 14% for the groups with paranoid ideation, psychotic symptoms, and psychotic symptoms and/or paranoid ideation, respectively. There were several interracial and intraracial differences in the receipt of mental health services as well as its perceived need. In the group with psychotic symptoms and/or paranoid ideation, 22% of the whites and 5% of the blacks reported a history of psychiatric treatment (χ2=3.12, df=1, p=0.02), and among blacks, 14% of the African Americans but only 1.5% of the African Caribbeans had received mental health treatment (χ2=2.31, df=1, p=0.13). With respect to the perceived need for treatment, 7% of the blacks versus 15% of the whites in the group with psychotic symptoms and/or paranoid ideation desired treatment (χ2=0.92, df=1, p=0.34); however, among blacks, 25% of the African Americans but only 1% of the African Caribbeans perceived a need for treatment (χ2=4.07, df=1, p=0.05).
Because of the possibility that paranoid ideation or psychoses might be primarily reflecting clinical depression, we examined the relationships between psychotic symptoms and/or paranoid ideation with major depressive disorder, according to DSM-IV symptom criteria. Among persons without any of these symptoms, 1.5% had a major depressive disorder, whereas 13% of the persons with psychotic symptoms and/or paranoid ideation (χ2=5.72, df=1, p=0.02) had a major depressive disorder. Moreover, when we further examined depressive symptoms using the CES-D Scale cutoff score of ≥16 for clinical depression, we found that 35% of the persons with psychotic symptoms and/or paranoid ideation versus 6% without psychotic symptoms and/or paranoid ideation exceeded the cutoff score (χ2=11.28, df=1, p<0.001).
Factors Affecting Symptoms in Blacks and Whites
With our theoretical model, in the black sample, we found that seven variables (lifetime trauma, belief in familial causes of mental illness, use of prayer to cope, larger social network, fewer persons on whom individuals could rely, higher CES-D Scale scores, and acute stressors) were significantly associated with paranoid ideation (Table 1). Five variables (use of or belief in spirituality, belief that spirits can cause mental illness, higher CES-D Scale scores, higher Self-Rating Anxiety Scale scores, and financial strain) were significantly associated with psychotic symptoms (Table 1), and seven variables (lifetime trauma, belief in familial causes of mental illness, use of prayer to cope, larger social networks, higher CES-D Scale scores, acute stressors, and greater ethnic identity) were significantly associated with the combined variable, psychotic symptoms and/or paranoid ideation (Table 2). In the white sample, we found five variables (use or belief in spiritualists, higher CES-D Scale scores, higher Self-Rating Anxiety Scale scores, acute stressors, and greater physical illness) were significantly associated with the combined variable, psychotic symptoms and/or paranoid ideation (Table 2).
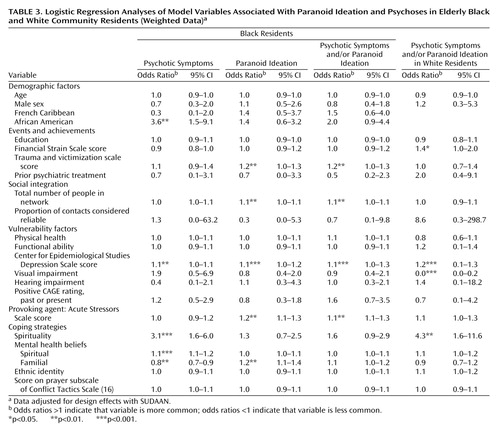
In logistic regression analysis, among blacks, five variables (depressive symptoms, acute stressors, lifetime trauma, larger social networks, and belief in familial causes of mental illness) were significantly associated with paranoid ideation (Table 3). Five variables (being born in the United States, having depressive symptoms, use of or belief in spiritualists, belief that spirits cause mental illness, diminished belief in familial causes of mental illness) were significantly associated with psychotic symptoms, and four variables (having depressive symptoms, having acute stressors, having lifetime trauma, and larger social networks) were significantly associated with the combined variable, psychotic symptoms and/or paranoid ideation. In looking at the white subsample, four variables (impaired vision, depressive symptoms, use of or belief in spiritualists, and financial strain) were associated with the combined variable, psychotic symptoms and/or paranoid ideation. For the groups with psychotic symptoms and/or paranoid ideation, when we replaced the CES-D Scale scores with the Self-Rating Anxiety Scale scores in the logistic regression model, the Self-Rating Anxiety Scale scores achieved significance in the black sample (χ2=7.34, df=1, p=0.01), whereas they did not attain significance in the white sample (χ2=0.13, df=1, p=0.92). With respect to the model used in this study, chi-squares for the black and white samples were significant (χ2=235.03, df=22, p<0.001, and χ2=55.84, df=20, p<0.001, respectively).
Discussion
Our study of a cognitively intact multiracial sample of older adults in Brooklyn, N.Y., revealed levels of symptoms, especially among the black groups, that were substantially higher than have been reported elsewhere (1–6), although the levels were comparable to the levels of psychotic symptoms reported among a younger and predominantly Hispanic sample of primary care patients (mean age=53 years) in Northern Manhattan (26). Overall, in our study, roughly one in seven persons ages 55 and older experienced paranoid ideation or psychotic symptoms. However, nearly one-fourth of the older blacks expressed paranoid ideation or psychotic symptoms, which was significantly greater than for the whites. Among the older whites, roughly one-tenth reported such symptoms, which was consistent with the prevalence rates in the literature. Even after appropriate design effects were taken into account, the inclusion of a Caribbean-born population that reflected the demographics of Brooklyn primarily accounted for the higher levels of symptoms than had been reported previously in older black samples. Indeed, the prevalence of paranoid ideation among older blacks born in the United States was only slightly higher than among older whites (13% versus 9%), whereas the levels among French Caribbeans were four times that of white persons.
What are the implications of these findings? First, the absence of a significant association between measures of functional impairment and paranoid ideation or psychotic symptoms suggests that these symptoms were not substantially affecting daily living. On the other hand, we found evidence that paranoid ideation or psychotic symptoms were associated with emotional dysfunction. For example, both older whites and blacks with paranoid ideation or psychoses had significantly more depressive symptoms and a greater prevalence of major depression than persons without such symptoms, i.e., 13% of the persons with paranoid ideation or psychoses had major depression versus 1.5% of the persons without depression. Also, among blacks, our analysis indicated that persons with psychotic symptoms and/or paranoid ideation had significantly more anxiety symptoms.
The strong relationship between depression and paranoid ideation and psychoses raises questions as to whether the latter are manifestations of depressive illness. Slightly over one-third of persons with psychotic symptoms and/or paranoid ideation met CES-D Scale criterion for clinical depression. Blazer and colleagues’ study of older adults in North Carolina (5) found that depressive symptoms were significant predictors of paranoid symptoms at a 3-year follow-up. Unfortunately, these authors did not examine to what extent paranoid ideation predicted subsequent depression. It is plausible that causality is bidirectional, with paranoid ideation and psychoses inducing depressive symptoms and vice versa. Longitudinal data are needed to tease apart these relationships.
Only 14% of the sample with psychotic symptoms and/or paranoid ideation had ever received psychiatric treatment, and even among those with both depression and psychotic symptoms and/or paranoid ideation, only 24% had received treatment. This suggests that more services are required. However, this conclusion must be tempered by the fact that only 11% of these persons thought that they required mental health services. Furthermore, there were racial disparities in the desire for treatment among persons with psychotic symptoms and/or paranoid ideation, with twice as many whites as blacks believing that they required services. This lack of interest in mental health services may reflect the acceptability of some level of these symptoms, especially given the weak association with functional impairments. This appears to be particularly likely among older African Caribbeans, whose use of and perceived need for mental health services were substantially lower than that of whites and African Americans.
For example, among older Caribbean immigrants, especially French Caribbeans from Haiti, the lingering effects of colonialism and the various types of political oppression, coupled with magical thinking and widespread belief in witchcraft and voodoo, may allow for greater cultural acceptance of paranoid ideation and modest levels of psychoses (27, 28). Moreover, whereas older blacks born in the United States have become increasingly more willing to use mental health services (7), older Caribbeans have been found to have negative views of mental health workers, and they still prefer to use their families, churches, or self-healing to deal with mental distress (27).
George’s model (9) was significant for both racial groups, and it helped uncover a variety of factors that heretofore had not been implicated in the etiology of psychoses and paranoid ideation in older persons. Most notably, particularly among blacks, acute stressors, lifetime traumatic events, beliefs about causes of mental illness, and belief in or use of spiritualists were found to be associated with paranoid ideation or psychotic symptoms. The fact that acute stressors and lifetime traumatic events were significant for blacks but not whites suggests that among older blacks, paranoid ideation and psychotic symptoms may be either manifestations of distress or ways of coping with adverse events. The associations with spiritual beliefs and practices raise questions as to whether psychotic symptoms reflect belief systems rather than abnormal psychiatric symptoms. Conversely, persons with such symptoms may be more apt to turn to spiritualism. Because our cross-sectional data cannot answer this question, an exploration of health beliefs and behaviors concerning spiritualism should be included in future studies.
Four variables—depressive symptoms, financial strain, visual impairment, and social contacts—that had been implicated in earlier studies (1–6) were significant in this study. However, whereas depressive symptoms were associated with paranoid ideation and psychoses in both racial groups, visual impairment and financial strain were only significant among whites, and network size was significant only for blacks. Moreover, the direction of the latter was contrary to expectations in that persons with paranoid ideation and psychoses had larger social networks. The larger networks among those with symptoms further reinforce our contention that these symptoms in the absence of functional impairment are socially acceptable in the black community. They also indicate that individuals with these symptoms remain sociable and are able to engage others. Racial differences in financial strain may reflect the fact that the black elderly population has uniformly low income so that there was little gradient in financial strain. It is not clear as to why there were racial differences in the effects of visual impairment; however, this variable has not been consistently implicated in other studies (3–5), and in our study, the variable is based on self-reports of impairment rather than on clinical assessments.
Our data further underscored the heterogeneity of the older black community. In multivariate analyses, African Americans showed a significantly higher proportion of psychotic symptoms, but they showed significantly lower levels of psychotic symptoms and/or paranoid ideation versus the Caribbean-born blacks, which primarily reflects the high levels of psychotic symptoms and/or paranoid ideation among French African Caribbeans. Thus, even after accounting for various clinical, social, and belief factors within the black community, intragroup symptom differences remained that could not be explained by our model but presumably reflected psychosocial elements that were not elicited in this study. Such underlying elements are further suggested by the fact that there were substantial intragroup differences with respect to perceived need for psychiatric treatment among those with psychotic symptoms and/or paranoid ideation. The model was also not completely successful in accounting for black-white differences in psychotic symptoms, paranoid ideation, and psychotic symptoms and/or paranoid ideation, which were attenuated but did not disappear once all the social, attitudinal, and clinical variables were examined concurrently.
The high prevalence of paranoid ideation and psychoses among this urban population of older adults, especially among blacks, points to a potential public health issue. While these symptoms are not associated with appreciable functional impairment, they are significantly associated with increased depression (in both blacks and whites) and anxiety (in blacks). Moreover, paranoid ideation and psychoses have been reported previously to be associated with higher mortality, poor physical health, and cognitive decline. Appropriate caution should be used in interpreting our findings since this study was confined to one urban setting and used cross-sectional data. Further exploration of these issues in other urban settings with longitudinal analyses can help clarify the impact of paranoid ideation and psychoses on the well-being of elders living in the community.
 |
 |
 |
Presented in part at the 156th annual meeting of the American Psychiatric Association, San Francisco, May 17–22, 2003. Received May 29, 2003; revision received Sept. 15, 2003; accepted Sept. 18, 2003. From SUNY Downstate Medical Center; Long Island University, Brooklyn, N.Y.; and New York University, New York. Address reprint requests to Dr. Cohen, Division of Geriatric Psychiatry, SUNY Downstate Medical Center, Box 1203, 450 Clarkson Ave., Brooklyn, NY 11203; [email protected] (e-mail). The authors thank Jeanne Teresi, Ph.D., Community Research Applications, Carol Lefkowitz, and Barbara Singh for their assistance. Supported by NIMH grant MH-53453.
1. Ostling S, Skoog L: Psychotic symptoms and paranoid ideation in a nondemented population-based sample of the very old. Arch Gen Psychiatry 2002; 59:53–59Crossref, Medline, Google Scholar
2. Forsell Y, Henderson AS: Epidemiology of paranoid symptoms in an elderly population. Br J Psychiatry 1996; 172:429–432Crossref, Google Scholar
3. Henderson AS, Korten AE, Levings C, Jorm AF, Christensen H, Jacomb PA, Rodgers B: Psychotic symptoms in the elderly: a prospective study in a population sample. Int J Geriatr Psychiatry 1998; 13:484–492Crossref, Medline, Google Scholar
4. Christenson R, Blazer D: Epidemiology of persecutory ideation in an elderly population in the community. Am J Psychiatry 1984; 141:1088–1091Link, Google Scholar
5. Blazer DG, Hays JC, Salive ME: Factors associated with paranoid symptoms in a community sample of older adults. Gerontologist 1996; 36:70–75Crossref, Medline, Google Scholar
6. Bazargan M, Bazargan S, King L: Paranoid ideation among elderly African American persons. Gerontologist 2001; 41:366–373Crossref, Medline, Google Scholar
7. Griffith EEH, Baker FM: Psychiatric care of African Americans, in Culture, Ethnicity, and Mental Illness. Edited by Gaw AC. Washington, DC, American Psychiatric Press, 1993, pp 147–173Google Scholar
8. Pierre-Pierre G: West Indians adding clout to the ballot box. New York Times, Sept 6, 1993, pp 17, 19Google Scholar
9. George LK: Social and economic factors, in Geriatric Psychiatry. Edited by Busse EW, Blazer DG. Washington, DC, American Psychiatric Press, 1989, pp 203–234Google Scholar
10. Kahn RL, Goldfarb AI, Pollack M, Peck A: Brief objective measures for the determination of mental status in the aged. Am J Psychiatry 1960; 117:326–328Link, Google Scholar
11. Zarit SH, Miller NE, Kahn RL: Brain functioning, intellectual impairment and education in the aged. J Am Geriatr Soc 1978; 26:58–67Crossref, Medline, Google Scholar
12. Zung WWK: A rating instrument for anxiety disorders. Psychosomatics 1971; 12:371–379Crossref, Medline, Google Scholar
13. Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. J Applied Psychol Measurement 1977; 1:385–401Crossref, Google Scholar
14. Lawton MP, Moss M, Fulcomer M, Kleban MH: A research and service-oriented Multilevel Assessment Instrument. J Gerontol 1982; 37:91–99Crossref, Medline, Google Scholar
15. Pearlin LI, Lieberman MA, Mehaghan EG, Mullen JT: The stress process. J Health Soc Behav 1981; 22:337–356Crossref, Medline, Google Scholar
16. Strauss MA: Measuring intrafamily conflict and violence: the Conflict Tactics (CT) Scales. J Marriage Fam 1979; 41:75–88Crossref, Google Scholar
17. Cohen CI, Ramirez M, Teresi J, Sokolovsky J: Predictors of becoming redomiciled among older homeless women. Gerontologist 1997; 37:67–74Crossref, Medline, Google Scholar
18. Chatters LM: Health disability and its consequences for subjective stress, in Aging in Black America. Edited by Jackson JS, Chatters LM, Taylor RJ. Newbury Park, Calif, Sage Publications, 1993Google Scholar
19. Sokolovsky J, Cohen CI: Toward a resolution of methodological dilemmas in network mapping. Schizophr Bull 1981; 7:109–116Crossref, Medline, Google Scholar
20. Birnbaum A: Measuring Level of Ethnic Identity: A Comparison of Two New Scales (unpublished doctoral dissertation). New Brunswick, NJ, Rutgers University, Graduate School of Applied and Professional Psychology, 1991Google Scholar
21. Ewing JA: Detecting alcoholism: the CAGE questionnaire. JAMA 1984; 252:1905–1907Crossref, Medline, Google Scholar
22. Derogatis LR, Lipman RS, Covi L: SCL-90: an outpatient psychiatric rating scale—preliminary report. Psychopharmacol Bull 1973; 9:13–28Medline, Google Scholar
23. Nunally JC: Psychometric Theory. New York, McGraw-Hill, 1967Google Scholar
24. Flaherty JA, Gaviria FM, Pathak, D, Mitchell T, Wintrob R, Richman JA, Birz S: Developing instruments for cross-cultural psychiatric research. J Nerv Ment Dis 1988; 176:257–263Medline, Google Scholar
25. Bruce M, Seeman T, Merrill S, Blazer D: The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. Am J Public Health 1994; 84:1796–1799Crossref, Medline, Google Scholar
26. Olfson M, Lewis-Fernández R, Weissman MM, Feder A, Gameroff MJ, Pilowsky D, Fuentes M: Psychotic symptoms in an urban general medicine practice. Am J Psychiatry 2002; 159:1412–1419Link, Google Scholar
27. Gopaul-McNicol S-A: Working With West Indian Families. New York, Guilford, 1993Google Scholar
28. Bibb A, Casimir GJ: Haitian families, in Ethnicity and Family Therapy, 2nd ed. Edited by McGoldrick M, Giordano J, Pearce JK. New York, Guilford, 1996, pp 97–111Google Scholar



