Is Low Dietary Intake of Omega-3 Fatty Acids Associated With Depression?
Abstract
OBJECTIVE: This study examined the association between the dietary intake of omega-3 fatty acids and low mood, major depression, and suicide. METHOD: A total of 29,133 men ages 50 to 69 years participated in a population-based trial in Finland. The intake of fatty acids and fish consumption were calculated from a diet history questionnaire. Self-reported depressed mood was recorded three times annually, data on hospital treatments due to a major depressive disorder were derived from the National Hospital Discharge Register, and suicides were identified from death certificates. RESULTS: There were no associations between the dietary intake of omega-3 fatty acids or fish consumption and depressed mood, major depressive episodes, or suicide. CONCLUSIONS: Dietary intake of omega-3 fatty acids showed no association with low mood level.
Omega-3 fatty acids are essential long-chain polyunsaturated fatty acids that are concentrated in the CNS, retina, and testes in humans. Alpha-linolenic acid is present in plants and is needed for the synthesis of eicosapentaenoic and docosahexaenoic acids that are received directly from marine sources.
There is some evidence that omega-3 fatty acids are linked to depression (1). Studies have reported reduced levels of omega-3 fatty acids in plasma and cell membranes from depressed patients (2–4). One double-blind, placebo-controlled trial (5) has shown that omega-3 supplements improve the short-term clinical course of patients with bipolar disorder.
Our aim was to study the association between the dietary intake of omega-3 fatty acids and low mood, depression, and suicide. Consumption of fish rich in long-chain omega-3 fatty acids, specifically, was assessed.
Method
This study was based on a cohort (N=29,133) from a randomized, double-blind, placebo-controlled primary prevention trial—the ATBC study (6). The study participants were recruited from the total male population of 50 to 69 years of age that was residing in southwestern Finland in 1985 (N=290,406). The review boards of the participating institutions approved the study. All subjects gave written informed consent before random assignment.
Diet and alcohol consumption were assessed through a validated food-use questionnaire to measure the habitual dietary intake over the previous year. The reproducibility of this method was 0.6 to 0.7, and the validity was 0.6 to 0.7 for most nutrients (7). The dietary intake of omega-3 fatty acids at baseline was calculated. The study endpoints were self-reported depressed mood, hospital treatment for a major depressive disorder, and death from suicide. The subjects reported feelings of anxiety and depression experienced in the 4 months since their previous study visit (three times annually) during the trial, ranging from 5 to 8 years in duration (median=6). Data on hospital treatment due to depressive disorder were derived from the National Hospital Discharge Register, which covers inpatient admissions to all medical and psychiatric hospitals in Finland. The follow-up of survival extended to Dec. 31, 1994. Data regarding deaths were derived from the Central Population Register, and the cause of death was reviewed from death certificates. Details of the assessment have been described elsewhere (8).
Both placebo and intervention groups were included in the analysis. Cox’s proportional hazards regression models were used to estimate the relationships between baseline dietary intake of omega-3 fatty acids, categorized in tertiles, and the first measures of low mood level. Potential risk factors for both major depressive disorder and suicide (age, body mass index, energy intake, serum total cholesterol level, high-density lipoprotein cholesterol level, consumption of alcohol, education, marriage, self-reported depression, self-reported anxiety, and smoking) were entered into the models as covariates. Dietary factors were adjusted for energy intake in the models (9). A test for trend was calculated.
Results
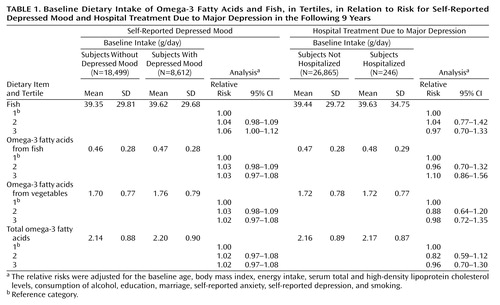
There was no significant association of fish consumption or intake of omega-3 fatty acids with any of the study endpoints (Table 1). A small, marginally elevated risk of self-reported depression was suggested in the highest tertile of fish consumption compared to the lowest tertile. A trend test showed the significance of fish consumption for self-reported depressed mood (z=2.09, df=1, p<0.04).
Discussion
Dietary intake of omega-3 fatty acids showed no association to low mood level and related outcomes. We linked the dietary intake of omega-3 fatty acids to the three-level assessment of low mood, as a symptom (self-report), and as pathology (disorder or suicide) in a population. A validated method to quantitative long-term diet was used. Even so, the present findings may not be generalized beyond our study population or to older male smokers.
Our findings conflict with the results of a controlled trial that suggested that fish omega-3 fatty acids might improve the short-term course of bipolar disorder (5). The dose of omega-3 fatty acids in that trial (9.6 g/day), however, exceeded the dietary intake level of our study (total intake of 2.2 g/day or 0.47 g/day from fish).
The average intake of omega-3 fatty acids tends to be rather similar in most of the Western countries. For example, the average intake of omega-3 fatty acids was 1.2 g/day in the United States (10). Therefore, the overall amount of omega-3 fatty acids in the diet of our population (2.2 g/day) is higher but still in line with that of other industrialized populations.
In addition, we compared the intake of omega-3 fatty acids of the highest decile and the lowest decile with that of the middle tertile. It is unlikely that there is a ceiling effect, since the intake does vary between the individuals and was rather low in those of the lowest decile. Whether omega-3 fatty acids raise mood and whether the necessary intake can be received from a certain diet are important questions that must await further studies.
 |
Received Nov. 28, 2002; revisions received June 3 and Aug. 5, 2003; accepted August 23, 2003. From the Department of Mental Health and Alcohol Research and the Department of Epidemiology and Health Promotion, National Public Health Institute; and the Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Md. Address reprint requests to Dr. Hakkarainen, Department of Mental Health and Alcohol Research, National Public Health Institute, Mannerheimintie 166, FIN-00300 Helsinki, Finland; [email protected] (e-mail).
1. Freeman MP: Omega-3 fatty acids in psychiatry: a review. Ann Clin Psychiatry 2000; 12:159–165Crossref, Medline, Google Scholar
2. Edwards R, Peet M, Shay J, Horrobin D: Omega-3 polyunsaturated fatty acid levels in the diet and in red blood cell membranes of depressed patients. J Affect Disord 1998; 48:149–155Crossref, Medline, Google Scholar
3. Maes M, Christophe A, Delanghe J, Altamura C, Neels H, Meltzer HY: Lowered omega3 polyunsaturated fatty acids in serum phospholipids and cholesteryl esters of depressed patients. Psychiatry Res 1999; 85:275–291Crossref, Medline, Google Scholar
4. Peet M, Murphy B, Shay J, Horrobin D: Depletion of omega-3 fatty acid levels in red blood cell membranes of depressive patients. Biol Psychiatry 1998; 43:315–319Crossref, Medline, Google Scholar
5. Stoll AL, Severus WE, Freeman MP, Rueter S, Zboyan HA, Diamond E, Cress KK, Marangell LB: Omega 3 fatty acids in bipolar disorder: a preliminary double-blind, placebo-controlled trial. Arch Gen Psychiatry 1999; 56:407–412Crossref, Medline, Google Scholar
6. ATBC Cancer Prevention Study Group: The alpha-tocopherol, beta-carotene lung cancer prevention study: design, methods, participant characteristics, and compliance. Ann Epidemiol 1994; 4:1–10Medline, Google Scholar
7. Pietinen P, Hartman AM, Haapa E, Rasanen L, Haapakoski J, Palmgren J, Albanes D, Virtamo J, Huttunen JK: Reproducibility and validity of dietary assessment instruments, I: a self-administered food use questionnaire with a portion size picture booklet. Am J Epidemiol 1988; 128:655–666Crossref, Medline, Google Scholar
8. Partonen T, Haukka J, Virtamo J, Taylor PR, Lönnqvist J: Association of low serum total cholesterol with major depression and suicide. Br J Psychiatry 1999; 175:259–262Crossref, Medline, Google Scholar
9. Willet W: Nutritional Epidemiology. New York, Oxford University Press, 1990Google Scholar
10. Suzuki S, Platz EA, Kawachi I, Willett WC, Giovannucci E: Intakes of energy and macronutrients and the risk of benign prostatic hyperplasia. Am J Clin Nutr 2002; 75:689–697Crossref, Medline, Google Scholar



