HIV Testing and Receipt of Test Results Among Homeless Persons With Serious Mental Illness
Abstract
OBJECTIVE: The purpose of this study was to determine the rates and predictors of HIV testing and receipt of results among homeless adults with serious mental illness in the initial 3-month period after contact with a community-based case management program. METHOD: Baseline and follow-up interview data came from clients (N=5,890) in the Access to Community Care and Effective Services and Supports program, an 18-site, 5-year federally sponsored demonstration designed to evaluate the effect of service system integration on outcomes for homeless persons with serious mental illness. RESULTS: Overall, 38.0% of clients were tested for HIV in the 3 months after program entry; of these, 88.8% returned to receive their test results. Likelihood of being tested was independently associated with having been tested before, more severe psychiatric symptoms and drug problems, level of worry about getting AIDS, younger age, less education, minority status, longer-term homelessness, being sexually assaulted, being arrested, and health services utilization. Among those tested, likelihood of receiving the test results was higher among those with a history of prior testing and return for results, a higher frequency of testing, and more years of education and lower among those with drug abuse problems, outpatient medical service utilization, disability, and sexually transmitted disease. Interaction analyses showed that, for men, greater social support increased the likelihood of both HIV testing and receipt of results, while sexual victimization during follow-up decreased the likelihood that men would return for their HIV results. CONCLUSIONS: The majority of homeless clients enrolled in an intensive case management program were not tested for HIV during the 3-month period after program entry. Among those tested, however, nearly 90% reported receiving their results. The findings may enhance the development and targeting of strategies to increase testing and awareness of HIV serostatus among high-risk mentally ill homeless persons.
Human immunodeficiency virus (HIV) testing is a cornerstone in efforts to detect, treat, and prevent HIV infection. With the advent of more effective therapies in recent years, early diagnosis is important in optimizing a treatment plan and forestalling the progression of AIDS and death (1). In addition, earlier awareness of one’s seropositivity may lead to decreased future transmission of the virus, given the long asymptomatic period during which an HIV-infected individual could unknowingly be spreading the virus to others. Even for those whose test results are negative, pre- and posttest counseling sessions provide valuable opportunities for HIV education and risk-reduction counseling. Of course, HIV testing alone is not enough; individuals must also return for their test results. Indeed, of the nearly 2.3 million publicly funded HIV tests that were performed in the United States in 1998, 48% of those tested had no posttest counseling, and some of the highest failure rates were among those most at risk for infection (2).
Compared with the general population, persons who are homeless and chronically mentally ill are at higher risk for HIV infection, reflecting their higher rates of drug use and sexual risk behaviors (3–6). Moreover, numerous studies have demonstrated HIV seroprevalence rates of ≥1% in homeless samples across the country (3, 7–9). Thus, according to Centers for Disease Control and Prevention (CDC) guidelines (1), homeless persons represent a population for whom HIV testing should be routinely recommended. Despite the importance of HIV testing, however, few studies (9–13) have examined factors associated with testing and return for test results in this vulnerable, high-risk population. The current literature in this area is somewhat limited in at least two respects. First, prior research has focused on identifying correlates of past HIV testing behaviors by using cross-sectional data, potentially limiting the interpretation of some associations. Second, previous studies have focused on groups of homeless persons living in specific locales and, therefore, are of limited generalizability.
In the present study, we used prospective data from a large, multisite homeless outreach demonstration project to determine the rates and predictors of HIV testing and receipt of test results among clients in the 3-month period after program entry. By identifying predisposing, enabling, and need factors associated with HIV testing and return for results, the findings of this study are expected to enhance the development and targeting of strategies to increase awareness of HIV serostatus among seriously mentally ill homeless persons.
Method
Data Source and Study Participants
The data for this study come from the Access to Community Care and Effective Services and Supports (ACCESS) program, which has been described in detail previously (14). Launched in 1994 by the federal Center for Mental Health Services, the ACCESS program was an 18-site, 5-year demonstration project designed to evaluate the effect of service systems integration on outcomes for homeless persons with serious mental illness. All sites received funding to establish both specialized outreach teams to make contact with untreated homeless people and intensive case management teams to provide comprehensive services for up to 1 year to approximately 100 new clients each year.
During the 4-year recruitment period, 7,530 individuals were referred to the ACCESS program and screened for eligibility. Of these, 7,229 (96.0%) were found to be eligible (see the summary of the eligibility criteria later in this section) and were invited to participate in the ACCESS demonstration, gave written informed consent, and completed a comprehensive baseline interview. Subjects were reinterviewed at 3 months after program entry. The interviews were conducted by trained interviewers who were not involved in the delivery of clinical services.
Individuals were eligible to participate in the ACCESS program if they were homeless, suffered from severe mental illness, and were not already involved in some form of treatment (15). Homelessness was defined as having spent at least seven of the past 14 nights in a shelter, outdoors, or in a public or abandoned building. Psychiatric eligibility was determined by using a 30-item screening algorithm that assessed symptoms of psychosis, depression, and mania, as well as interviewer-rated overtly disturbed behavior. The screening algorithm, developed for a previous outreach demonstration project for homeless persons with serious mental illness, was validated by using the Structured Clinical Interview for DSM-III-R and demonstrated 91% sensitivity (i.e., it correctly identified 91% of persons with axis I nonsubstance-use psychiatric disorders) (16).
Dependent Variables
The two dichotomous outcome measures for this study were drawn from the 3-month follow-up interview and reflected whether individuals had been tested for HIV during the follow-up period and, if so, whether they received the test results.
Independent Variables
Our selection of potential predictors was guided by Gelberg and colleagues’ Behavioral Model for Vulnerable Populations (17), which posits that health-seeking behavior among vulnerable groups, such as homeless persons, is a function of three categories of variables: predisposing, enabling, and need factors. Predisposing factors are personal characteristics that influence the likelihood of using health services. Enabling factors include the individual, family, and clinical resources that are instrumental in obtaining services. Need factors relate to the conditions and circumstances that provide the impetus for seeking health care. Unless otherwise stated, potential predictor variables were drawn from the baseline interview.
Predisposing factors
We included the following demographic and social structure characteristics: age, gender, marital status, veteran status, race, years of education completed, and duration of the current episode of homelessness. We also included measures of social support, disability, and criminal activity. Level of social support was based on measures of network size and perceived availability of resources (18) and reflected the number of types of people the client could count on for a loan, a ride to an appointment, or help with an emotional crisis (Cronbach’s alpha=0.74); possible scores ranged from 0 to 18. Disability status reflected the client’s self-reported usual pattern of employment over the past 12 months. Data from the 3-month follow-up interview were used to create a dichotomous variable to indicate whether the client had been arrested and charged with one or more of the following major criminal offenses during the past 2 months: parole/probation violations; drug charges; forgery; weapons offense; burglary, larceny, or breaking and entering; robbery; assault; arson; rape; and homicide/manslaughter.
For baseline physical health status, a summary score with a possible range of 0 to 16 was calculated from the following self-report checklist of current medical conditions: diabetes; anemia; high blood pressure; heart disease/stroke; problems with liver; arthritis, rheumatism, or joint problems; chest infection, cold, cough, or bronchitis; pneumonia; problems with seizures; tuberculosis; skin problems; lice, scabies, or other similar infestations; problem walking, lost limb, or other physical limitations; problems with teeth; gynecological problems; and traumatic injuries. It is noteworthy that the presence of a current sexually transmitted disease other than HIV was also assessed at baseline; however, it was not included in the summary score. As described later in this section, having a sexually transmitted disease was considered to be a need factor with respect to HIV testing.
Enabling factors
We included income in the past month as a traditional enabling variable. Using data from the follow-up interview, we also included variables indicating whether clients had received various outpatient and inpatient services during the past 60 days. These service utilization variables were considered to be enabling in that contacts with the health care system represent potential opportunities for HIV risk assessment, education, and referral for testing and counseling.
Another variable that was hypothesized to be potentially enabling was clients’ follow-up assessment of the quality of the relationship, or therapeutic alliance, with their primary clinician (usually, case manager). To measure this variable, we used the Therapeutic Alliance Scale (19). We assigned clients to one of three levels of therapeutic alliance: no primary clinician identified, low alliance with clinician (score below the median of 44), or high alliance with clinician (greater than or equal to the median score) (20).
Need factors
As noted earlier, one of the need variables considered in this study was whether clients had a sexually transmitted disease other than HIV at baseline, given the high rates of coinfection of sexually transmitted diseases and HIV and the presence of shared risk factors (21). We also included a variable indicating whether clients had been sexually assaulted during the 2-month period before the follow-up interview.
Given the association of substance abuse and psychiatric symptoms with HIV risk and risk behaviors, data from baseline and follow-up interviews were used to determine substance abuse and psychiatric symptoms at baseline as well as changes in mental health status. Substance abuse was measured by using two composite scores—one for alcohol and the other for other drugs—from the Addiction Severity Index (22), which includes questions that assess the frequency of use, amount of intake, and problems associated with use. Individual items were weighted and summed (based on the number of questions and the maximum response) so that possible alcohol and drug scores ranged from 0, indicating no problems with the substance, to 1, indicating severe problems with the substance.
To measure psychiatric (mood and psychotic) symptoms, an index was created by averaging standardized scores on three mental health instruments with a total of 26 items: the Addiction Severity Index psychiatric composite problem index (22), the depression scale derived from the National Institute of Mental Health Diagnostic Interview Schedule (23), and the psychotic symptom scale derived from the Psychiatric Epidemiology Research Interview (24) (Cronbach’s alpha=0.75). We also included an objective, interviewer-rated measure of overtly psychotic behavior (25) that was assessed only at baseline (no change in score examined). The 13 items assessing unusual speech, affect, agitation, and responses to internal stimuli and delusions were each coded from 0 (not at all) to 4 (a large extent), yielding a summary score with a possible range of 0 to 52.
Self-perceived need for testing was assessed by asking clients about their level of worry about getting AIDS; responses ranged from 0, indicating “not at all,” to 4, indicating “extremely.” Finally, we included a measure of clients’ HIV testing history. Using baseline responses to questions about whether they had ever been tested for HIV and whether they got the results, we categorized clients into one of three groups: never tested before, tested but did not get results, and tested and got results. (Clients in the latter group were known to be HIV-negative at baseline, since those who reported being HIV-positive at baseline were excluded).
Data Analysis
Simple, univariate statistics were used to describe the study group and to summarize rates of HIV testing and receipt of test results during the 3-month follow-up period after program entry. Parallel bivariate and multivariate analyses were then performed for the two outcome measures. First, bivariate associations of potential predisposing, enabling, and need factors with each of the outcomes were assessed by using chi-square tests for categorical variables and t tests for continuous variables.
Second, multivariate logistic regression modeling was performed to identify independent predictors of HIV testing and receipt of results. We used generalized estimating equation techniques (26) to account for the clustering of clients within program sites. For each outcome, a backward elimination strategy was used to determine the most parsimonious set of predictors; variables that were significant at the 0.05 level were retained in the final models. Because a recent study found some gender differences in correlates of HIV testing and return for results (11) and because the study clients included a substantial number of both men and women, we not only considered all main effects but also evaluated all first-order interaction terms with gender. All analyses were performed by using the SAS System for Windows, Version 8 (SAS Institute, Cary, N.C.).
Results
Study Participants
In total, 7,229 individuals were enrolled in the ACCESS program and completed a baseline interview. Nonmutually exclusive psychiatric diagnoses, based on a clinician’s assessment at the time of referral, included major depression (48.7%), schizophrenia (36.2%), other psychoses (31.4%), personality disorder (22.0%), bipolar disorder (20.3%), and anxiety disorder (18.0%). Rates of substance abuse were also high (42.8% with alcohol abuse and 38.4% with drug abuse).
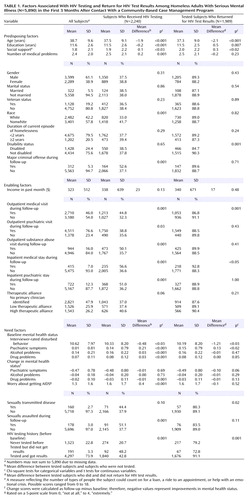
For the purposes of this study, we excluded 237 individuals (3.3%) who reported being HIV-positive at baseline. Of the remaining 6,992 persons, 1,035 (14.8%) were excluded because they did not have a 3-month follow-up interview; an additional 67 (1.0%), although interviewed, were excluded because of missing outcome data. Thus, the final number of participants was 5,890. Compared with clients who were lost to follow-up, those who completed a follow-up interview were significantly more likely to be female (χ2=8.79, df=1, p=0.003) and nonwhite (χ2=12.50, df=1, p=0.001) and to have greater social support (t=4.69, df=6983, p<0.001), medical problems (t=2.46, df=6990, p<0.02), and psychiatric symptoms (t=2.47, df=6765, p<0.02) (data not shown). The characteristics of the study participants are summarized in Table 1.
Rates of HIV Testing and Return for Test Results During Follow-Up
Of the 5,890 clients included in this study, 2,240, or 38.0%, reported being tested for HIV during the 3-month follow-up period. Among those tested, 88.8% (1,989/2,240) reported receiving their test results. Across sites, the rate of testing ranged from 26.6% to 48.1% and the rate of receipt of test results ranged from 69.4% to 99.3%.
Predictors of HIV Testing
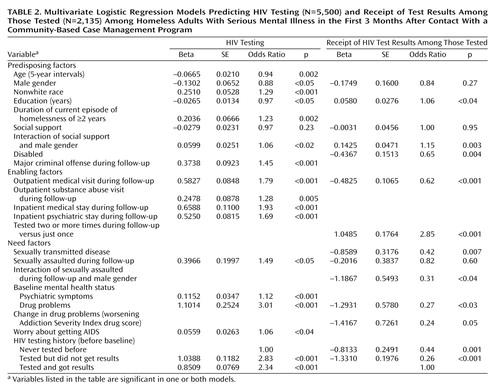
Bivariate associations between all potential predictors and HIV testing are presented in Table 1, and the final logistic regression model is presented in Table 2. As Table 2 shows, the likelihood of being tested for HIV after program entry decreased as both age and educational level increased.
Positive predictors of testing included the following HIV risk-related variables: nonwhite race, longer-term homelessness, being sexually assaulted during follow-up, more severe psychiatric symptoms and drug problems, and self-perceived risk or level of worry about getting AIDS. Among the strongest predictors of HIV testing was clients’ prior testing history; that is, clients who had been tested before, regardless of whether they ever got the results, were significantly more likely to be tested during follow-up than those who had never been tested before. Health services utilization and having been arrested and charged with a major crime during follow-up were also strongly associated with receipt of HIV testing.
Finally, we found a significant interaction between social support and gender. At lower levels of social support, men were less likely than women to be tested for HIV. As the level of social support increased, however, so did the likelihood of being tested, but only among men; the same was not true for women.
Predictors of Receipt of HIV Test Results
Bivariate and multivariate associations between predictor variables and the likelihood of getting one’s HIV test results are presented in Table 1 and Table 2, respectively. As Table 2 shows, receipt of results among those tested was positively associated with level of education and negatively associated with being disabled, outpatient medical service utilization, having a sexually transmitted disease other than HIV, and both drug problems at baseline and worsening drug problems over the course of follow-up.
Frequency of HIV testing during follow-up and prior testing history were also predictive of getting the results. Twenty-one percent (473/2,240) of those tested for HIV during follow-up were tested more than one time, and the odds of getting their results were nearly threefold greater in this group, compared with clients who were tested just once. As for HIV testing history, both first-time test recipients and those who had a history of being tested but not getting the results were significantly less likely to get their HIV results during follow-up than were clients who had a track record of returning for test results.
Moreover, we found two significant gender interaction terms. First, like the odds for HIV testing, the odds of returning for test results were increased by social support among men but not among women. Second, having been sexually assaulted decreased the likelihood that men would return for their HIV test results; the same was not true for women, however.
Discussion
Using prospective data from the ACCESS demonstration, we found that, despite CDC guidelines that high-risk, high-prevalence populations be routinely recommended HIV testing (1), less than 40% of ACCESS clients reported being tested for HIV in the 3 months after program entry. Of those tested, however, 88.8% reported receiving their test results. Using the framework of Gelberg et al. (17), we identified predictors of HIV testing and receipt of results from predisposing, enabling, and need domains in an effort to identify potential target populations for interventions aimed at increasing HIV serostatus awareness.
Previous cross-sectional studies have shown that persons who are at greatest risk for HIV infection due to sociodemographic, sexual, and clinical risk factors are usually the most likely to have been tested (27, 28). Consistent with these findings, we found that significant, independent predictors of HIV testing during follow-up included younger age, less education, nonwhite race, longer-term homelessness, being sexually assaulted during follow-up, higher levels of psychiatric symptoms and drug problems, and greater worry about getting AIDS.
None of these HIV risk-related variables, however, also predicted following through with getting the results among those tested. On the contrary, drug problems (both higher levels at baseline and worsening problems over the follow-up period), as well as being disabled, appeared to be impediments to returning for results. Moreover, whereas being a victim of sexual assault increased the odds of getting tested for HIV, perhaps due to greater contact with emergency health services, sexual victimization was associated with decreased odds of returning for results, particularly among men. Having a sexually transmitted disease other than HIV also was associated with failure to get HIV test results. These latter findings are consistent with studies suggesting that denial and fear may serve as barriers to learning one’s HIV status (28, 29). Taken together, they point to the need for targeted interventions on the part of HIV counselors and mental health providers to increase rates of return for test results among at-risk individuals who, for whatever reason, may be unable or unwilling to get their results. Efforts to develop better coping skills, for example, have been shown to reduce HIV risk behaviors in impoverished populations (30) and may be effective in increasing rates of HIV testing and return for results (10, 11).
Consistent with previous research demonstrating an association between access to care and receipt of HIV testing (31), we found that clients who were linked with outpatient medical and substance abuse services were significantly more likely to be tested than were those who did not receive such services. In addition, we found that inpatient stays and having been arrested and charged with a major crime increased the likelihood of HIV testing. While these latter findings are consistent with studies documenting relatively high rates of “voluntary” testing in hospitals (32) and prisons (33), it is important to note that higher acceptance rates are more likely when informed consent is vague and HIV testing is presented as “routine” rather than as optional (28). Believing that HIV testing is mandatory and bundled with other services, institutionalized persons may be more likely than their noninstitutionalized counterparts to accept testing.
An important predictor of HIV testing and receipt of results during follow-up was clients’ prior experience with HIV testing. Knowing whether clients have been tested previously and, if so, whether they received those earlier results will help clinicians to identify individuals who may benefit from additional and more careful follow-up. In addition, repeated HIV testing during follow-up increased the likelihood of actually getting the results and thus may prove to be a useful strategy in helping to increase HIV serostatus awareness among mentally ill homeless persons, who often live chaotic lives and for whom returning for test results may be a challenge.
This study had some limitations. First, although the baseline participation rate was high, follow-up interviews were missing for 15% of the baseline participants. Because those who were lost to follow-up may have been the least likely to receive needed services, we may have overestimated the rates of HIV testing and receipt of results in this group of clients.
Second, the ACCESS program was not focused on HIV/AIDS and related outcomes; therefore, detailed information was not available on high-risk sexual or substance abuse behaviors. Nevertheless, we were able to examine the effect of a broad array of individual-level predisposing, enabling, and need factors on HIV testing and receipt of results.
Third, the study relied on self-reported data. We were not able to validate responses using external sources, such as medical records. However, others have demonstrated a reasonably high level of validity for self-reported data about HIV testing and results (34).
Finally, given the complex needs of clients and the competing demands on clinicians, it may be argued that the 3-month follow-up period was too short and that if one were to look over a longer period of time, a greater percentage with HIV testing would be found. As a secondary analysis, we looked at available 12-month follow-up data for the study participants and found that an additional 1,123 clients reported being tested for HIV sometime between the two follow-up interviews, resulting in a total percentage tested of 57.1% (3,363/5,890) in the year after program entry. Although the appropriate timing and frequency of testing have not been firmly established (1), these data highlight that a substantial proportion of clients did not receive HIV testing even a year after initial contact with the program and that, among those who were tested, fully two-thirds were tested in the first 3 months after program entry.
In summary, we found a high rate of follow-through in returning for HIV test results among those tested, which likely reflects the fact that the study participants were enrolled in an intensive case management program. In this sense, our findings may overestimate the experience of vulnerable homeless persons contacted through other programs or points of service delivery. Despite the ACCESS program’s emphasis on case management and coordination of care, however, and despite public health guidelines, the majority of clients were in fact not tested for HIV in the 3-month period after program entry, and a substantial proportion were not tested even after 12 months. These findings highlight the need for greater efforts to increase testing and awareness of HIV serostatus among high-risk homeless persons in order to better care for HIV-positive individuals and potentially reduce future transmission of the virus. Activities aimed at educating both clients and mental health providers about HIV may be effective in increasing rates of HIV testing and counseling among homeless persons with serious mental illness.
 |
 |
Received Sept. 17, 2003; revision received Feb. 25, 2004; accepted March 17, 2004. From the Mental Illness Research, Education, and Clinical Center and the Northeast Program Evaluation Center, VA Connecticut Healthcare System; and the Departments of Psychiatry and of Epidemiology and Public Health, Yale University School of Medicine, New Haven, Conn. Address reprint requests to Dr. Desai, VA Connecticut Healthcare System, NEPEC (182), 950 Campbell Ave., West Haven, CT 06516; [email protected] (e-mail). Supported by interagency agreement AM-9512200A between the Center for Mental Health Services and the Department of Veterans Affairs Northeast Program Evaluation Center and through a contract between the Center for Mental Health Services and ROW Sciences, Inc. (now part of Northrop Grumman Corp.) and subcontracts between ROW Sciences, Inc., and the Cecil A. Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill, the University of Maryland, Baltimore, and Policy Research Associates, Delmar, New York.
1. Centers for Disease Control and Prevention (CDC): Revised guidelines for HIV counseling, testing, and referral. MMWR Recomm Rep 2001; 50(RR-19):1–57Google Scholar
2. Centers for Disease Control and Prevention (CDC): HIV Counseling and Testing in Publicly Funded Sites Annual Report, 1997 and 1998. Atlanta, CDC, 2001Google Scholar
3. Allen DM, Lehman JS, Green TA, Lindegren ML, Onorato IM, Forrester W: HIV infection among homeless adults and runaway youth, United States, 1989–1992. AIDS 1994; 8:1593–1598Crossref, Medline, Google Scholar
4. Checkley GE, Thompson SC, Crofts N, Mijch AM, Judd FK: HIV in the mentally ill. Aust NZ J Psychiatry 1996; 30:184–194Crossref, Medline, Google Scholar
5. Susser E, Miller M, Valencia E, Colson P, Roche B, Conover S: Injection drug use and risk of HIV transmission among homeless men with mental illness. Am J Psychiatry 1996; 153:794–798Link, Google Scholar
6. Susser E, Valencia E, Miller M, Tsai W-Y, Meyer-Bahlburg H, Conover S: Sexual behavior of homeless mentally ill men at risk for HIV. Am J Psychiatry 1995; 152:583–587Link, Google Scholar
7. Zolopa AR, Hahn JA, Gorter R, Miranda J, Wlodarczyk D, Peterson J, Pilote L, Moss AR: HIV and tuberculosis infection in San Francisco’s homeless adults: prevalence and risk factors in a representative sample. JAMA 1994; 272:455–461Crossref, Medline, Google Scholar
8. Fournier AM, Tyler R, Iwasko N, LaLota M, Shultz J, Greer PJ: Human immunodeficiency virus among the homeless in Miami: a new direction for the HIV epidemic. Am J Med 1996; 100:582–584; correction, 101:239Crossref, Medline, Google Scholar
9. Herndon B, Asch SM, Kilbourne AM, Wang M, Lee M, Wenzel SL, Andersen R, Gelberg L: Prevalence and predictors of HIV testing among a probability sample of homeless women in Los Angeles County. Public Health Rep 2003; 118:261–269Crossref, Medline, Google Scholar
10. Nyamathi AM, Stein JA, Swanson JM: Personal, cognitive, behavioral, and demographic predictors of HIV testing and STDs in homeless women. J Behav Med 2000; 23:123–147Crossref, Medline, Google Scholar
11. Stein JA, Nyamathi A: Gender differences in behavioural and psychosocial predictors of HIV testing and return for test results in a high-risk population. AIDS Care 2000; 12:343–356Crossref, Medline, Google Scholar
12. Goodman E, Berecochea JE: Predictors of HIV testing among runaway and homeless adolescents. J Adolesc Health 1994; 15:566–572Crossref, Medline, Google Scholar
13. De Rosa CJ, Montgomery SB, Hyde J, Iverson E, Kipke MD: HIV risk behavior and HIV testing: a comparison of rates and associated factors among homeless and runaway adolescents in two cities. AIDS Educ Prev 2001; 13:131–148Crossref, Medline, Google Scholar
14. Randolph F, Blasinsky M, Morrissey JP, Rosenheck RA, Cocozza J, Goldman HH (Access to Community Care and Effective Services and Supports [ACCESS] National Evaluation Team): Overview of the ACCESS program. Psychiatr Serv 2002; 53:945–948Link, Google Scholar
15. Rosenheck R, Lam JA: Individual and community-level variation in intensity and diversity of service utilization by homeless persons with serious mental illness. J Nerv Ment Dis 1997; 185:633–638Crossref, Medline, Google Scholar
16. Shern DL, Tsemberis S, Winarski J, Cope N, Cohen M, Anthony WA: A psychiatric rehabilitation demonstration for individuals who are street dwelling and seriously disabled, in Mentally Ill and Homeless: Special Programs for Special Needs. Edited by Breakey W, Thompson J. Amsterdam, Harwood Academic, 1997, pp 119–147Google Scholar
17. Gelberg L, Andersen RM, Leake BD: The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res 2000; 34:1273–1302Medline, Google Scholar
18. Lam JA, Rosenheck R: Social support and service use among homeless persons with serious mental illness. Int J Soc Psychiatry 1999; 45:13–28Crossref, Medline, Google Scholar
19. Neale MS, Rosenheck RA: Therapeutic alliance and outcome in a VA intensive case management program. Psychiatr Serv 1995; 46:719–721Link, Google Scholar
20. Chinman MJ, Rosenheck R, Lam JA: The case management relationship and outcomes of homeless persons with serious mental illness. Psychiatr Serv 2000; 51:1142–1147Link, Google Scholar
21. Clottey C, Dallabetta G: Sexually transmitted diseases and human immunodeficiency virus: epidemiologic synergy? Infect Dis Clin North Am 1993; 7:753–770Medline, Google Scholar
22. McLellan AT, Luborsky L, Woody GE, O’Brien CP: An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. J Nerv Ment Dis 1980; 168:26–33Crossref, Medline, Google Scholar
23. Robins LN, Helzer JE, Croughan J, Ratcliff KS: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry 1981; 38:381–389Crossref, Medline, Google Scholar
24. Dohrenwend B: Psychiatric Epidemiology Research Interview (PERI). New York, Columbia University, Social Psychiatry Unit, 1982Google Scholar
25. Rosenheck R, Lam JA: Homeless mentally ill clients’ and providers’ perceptions of service needs and clients’ use of services. Psychiatr Serv 1997; 48:381–386Link, Google Scholar
26. Liang K-Y, Zeger SL: Regression analysis for correlated data. Annu Rev Public Health 1993; 14:43–68Crossref, Medline, Google Scholar
27. Berrios DC, Hearst N, Coates TJ, Stall R, Hudes ES, Turner H, Eversley R, Catania J: HIV antibody testing among those at risk for infection: the National AIDS Behavioral Surveys. JAMA 1993; 270:1576–1580Crossref, Medline, Google Scholar
28. Irwin KL, Valdiserri RO, Holmberg SD: The acceptability of voluntary HIV antibody testing in the United States: a decade of lessons learned. AIDS 1996; 10:1707–1717Crossref, Medline, Google Scholar
29. Siegel K, Raveis VH, Gorey E: Barriers and pathways to testing among HIV-infected women. AIDS Educ Prev 1998; 10:114–127Medline, Google Scholar
30. Stein JA, Nyamathi A, Kington R: Change in AIDS risk behaviors among impoverished minority women after a community-based cognitive-behavioral outreach program. J Community Psychol 1997; 25:519–533Crossref, Google Scholar
31. Mosen DM, Wenger NS, Shapiro MF, Andersen RM, Cunningham WE: Is access to medical care associated with receipt of HIV testing and counselling? AIDS Care 1998; 10:617–628Crossref, Medline, Google Scholar
32. Harris RL, Boisaubin EV, Salyer PD, Semands DF: Evaluation of a hospital admission HIV antibody voluntary screening program. Infect Control Hosp Epidemiol 1990; 11:628–634Crossref, Medline, Google Scholar
33. Cotten-Oldenburg NU, Jordan BK, Martin SL, Sadowski LS: Voluntary HIV testing in prison: do women inmates at high risk for HIV accept HIV testing? AIDS Educ Prev 1999; 11:28–37Medline, Google Scholar
34. McCusker J, Stoddard AM, McCarthy E: The validity of self-reported HIV antibody test results. Am J Public Health 1992; 82:567–569Crossref, Medline, Google Scholar



