Axis I Comorbidity in Patients With Borderline Personality Disorder: 6-Year Follow-Up and Prediction of Time to Remission
Abstract
OBJECTIVE: The purpose of this study was to assess the prevalence of axis I disorders among patients with borderline personality disorder over 6 years of prospective follow-up. METHOD: A semistructured interview of demonstrated reliability was used to assess presence or absence of comorbid axis I disorders in 290 patients who met Revised Diagnostic Interview for Borderlines criteria and DSM-III-R criteria for borderline personality disorder and 72 patients who did not meet these criteria but did meet DSM-III-R criteria for another axis II disorder. Over 94% of surviving patients were reinterviewed about their axis I disorders at 2-year, 4-year, and 6-year follow-up periods. RESULTS: Although the patients with borderline personality disorder experienced declining rates of many axis I disorders over time, the rates of these disorders remained high, particularly the rates of mood and anxiety disorders. Patients whose borderline personality disorder remitted over time experienced substantial decline in all comorbid disorders assessed, but those whose borderline personality disorder did not remit over time reported stable rates of comorbid disorders. When the absence of comorbid axis I disorders was used to predict time to remission, the absence of substance use disorders was a far stronger predictor of remission from borderline personality disorder than was the absence of posttraumatic stress disorder, mood disorders, other anxiety disorders, or eating disorders, respectively. CONCLUSIONS: The results of this study suggest that axis I disorders are less common over time in patients with initially severe borderline personality disorder, particularly for patients whose borderline personality disorder remits over time. The findings also suggest that substance use disorders are most closely associated with the failure to achieve remission from borderline personality disorder.
Clinical experience suggests that a high percentage of patients with borderline personality disorder meet criteria for axis I disorders during the course of outpatient treatment or when hospitalized for psychiatric reasons. Numerous cross-sectional studies have documented this clinical impression by finding high rates of co-occurring mood, anxiety, substance use, and eating disorders in outpatients and inpatients with borderline personality disorder (1–5).
Clinicians also believe that the presence of certain co-occurring conditions impedes the symptomatic recovery of patients with borderline personality disorder and interferes with their psychosocial adjustment as well. To date, 17 small-scale, short-term prospective studies of the 1–7-year course of borderline personality disorder have been conducted (6–25). Only five of these studies (10–12, 18, 25) have assessed the presence of any co-occurring axis I disorders at follow-up. These studies have found that mood disorders, particularly unipolar disorders, are common. More specifically, the studies found that 48%–54% of patients with borderline personality disorder met criteria for a mood disorder, with a median figure of 52% (10, 11, 25). The range for major depression was 18%–40%, with a median of 29% (10–12, 18, 25). Dysthymic disorder was diagnosed in 14%–28% of the patients with borderline personality disorder, with a median of 15% (10, 18, 25). Bipolar spectrum disorders were less common; they were found in 7%–15% of patients with borderline personality disorder, with a median of 9% (10, 11, 18).
Substance use disorders were also found to be common among patients with borderline personality disorder at follow-up. Rates ranged from 14% to 56%, with a median co-occurrence of 52% (10, 18, 25). Anxiety disorders and eating disorders were found far less commonly in the one study that assessed their presence (10); in this study, only 7% of patients with borderline personality disorder met criteria for an anxiety disorder and only 15% met criteria for an eating disorder.
Four long-term, large-scale, follow-back studies of criteria-defined patients with borderline personality disorder have also been conducted, with a mean follow-up period of 14–16 years (26–30). One study (28) found that substance abuse and mood disorders were relatively common at follow-up. The second study that assessed any aspect of axis I comorbidity at follow-up found that 22% of patients with borderline personality disorder met DSM-IV criteria for dysthymic disorder at a second follow-up a mean of 27 years after their index admission (30).
The methodological limitations of these earlier studies have been described in detail elsewhere (31). Briefly, these limitations include use of chart review or clinical interviews to diagnose borderline personality disorder, use of only one reassessment after baseline, variable number of years of follow-up in the same study, no comparison group or use of less than optimal comparison subjects, nonblind assessments after baseline, and reliance on small numbers of subjects with high attrition rates. In addition, unstructured clinical interviews were used more often than semistructured diagnostic interviews—a practice that tends to underestimate the presence of co-occurring axis I disorders (32).
To our knowledge, the current study is the first study to systematically assess a full array of axis I disorders at four contiguous 2-year time periods in a well-defined group of patients with borderline personality disorder and comparison subjects with other axis II diagnoses. Our study design is distinguished by the size of the patient groups studied and the rigor with which they were diagnosed. The design is also distinguished by the use of a semistructured interview of demonstrated reliability to assess the presence of axis I disorders at each of the time periods.
Method
The current study is part of a multifaceted longitudinal study of the course of borderline personality disorder—the McLean Study of Adult Development. The methods of this study have been described in detail elsewhere (31). Briefly, all subjects were initially inpatients at McLean Hospital in Belmont, Mass., who were admitted during a 3-year period (1992–1995). Each patient was screened to determine that he or she was between the ages of 18–35; had a known or estimated IQ of 71 or higher; had no history or current symptoms of schizophrenia, schizoaffective disorder, bipolar I disorder, or an organic condition that could cause psychiatric symptoms; and was fluent in English. Subjects with the specified disorders were excluded from the study because of the difficulty in determining long-standing personality patterns in individuals suffering from psychosis, mania, or an organic condition with serious psychological sequelae.
After the study procedures were explained at baseline, written informed consent was obtained from all participating patients. Each patient then met with a master’s-level interviewer who was blind to the patient’s clinical diagnoses. Three semistructured diagnostic interviews were administered: 1) the Structured Clinical Interview for DSM-III-R Axis I Disorders (SCID) (33), 2) the Revised Diagnostic Interview for Borderlines (DIB-R) (34), and 3) the Diagnostic Interview for Personality Disorders (35). Good-to-excellent levels of interrater and test-retest reliability were achieved at baseline for both axis I and axis II disorders (36, 37). For axis I disorders, interrater kappas ranged from 0.69 to 1.00, with a median of 0.88; test-retest kappas ranged from 0.42 to 1.00, with a median of 0.76.
At each follow-up, diagnostic information was obtained by staff members blind to baseline diagnoses using interview methods similar to those used at baseline. After written informed consent was again obtained, our diagnostic battery was readministered (a change version of the SCID, the DIB-R, and the Diagnostic Interview for Personality Disorders). Good-to-excellent interrater reliability was maintained throughout the course of the study for both axis I and axis II diagnoses (36, 37). Both conjoint patient interviews and videotapes from previous interviews were used to maintain high levels of interrater reliability and prevent rater drift throughout the years of follow-up. In terms of the conjoint interviews, axis I kappas ranged from 0.71 to 1.00, with a median of 0.93. For videotaped interviews from earlier follow-up periods, axis I kappas ranged from 0.71 to 1.00, with a median of 0.84.
Data pertaining to axis I disorders were assembled in panel format (i.e., multiple records per patient, with one record for each assessment period for which data were available). Random effects regression modeling methods assessing the role of diagnosis and time and controlling for clinically important baseline covariates (gender, race, age, socioeconomic status, Global Assessment of Functioning Scale [GAF] [DSM-III-R, p. 12] score, and number of treatment modalities) were used in all analyses of axis I data (38). In this modeling work, probit analyses of binary dependent variables (e.g., presence versus absence of major depression) were used. We also investigated the role of remission status among the patients with borderline personality disorder and in these analyses used the following predictor variables: remission versus no remission, time, gender, race, age, socioeconomic status, GAF score, and number of treatment modalities. Interactions between diagnosis and time (and remission status and time) were checked in this modeling. Model fits were checked by examination of partial residual plots. Because of the multiple comparisons involved in the analyses of axis I panel data, Bonferroni-type corrections were applied to the p values for the main effects of diagnosis and time (and remission status and time). Because there were 25 such comparisons, this resulted in an adjusted p value of 0.002 (0.05/25).
We defined time to remission as the follow-up period at which remission was first achieved. Thus, possible values for the time to remission measure were 1, 2, or 3, with time=1 for patients who first achieved remission at the first follow-up period (24 months after baseline), time=2 for those who first achieved remission at the second follow-up period (48 months after baseline), and time=3 for those who first achieved remission at the third follow-up period (72 months after baseline). Because this time measure is discrete, survival analytic methods assuming continuous time (such as Cox proportional hazards regression modeling) could not be used. Instead, we used discrete time-to-event modeling methods, which yield adjusted hazard ratios and 95% confidence periods (39).
Results
The study group included 290 patients who met both DIB-R and DSM-III-R criteria for borderline personality disorder and 72 patients who did not meet either set of criteria for borderline personality disorder but met DSM-III-R criteria for at least one other axis II disorder. Baseline demographic data for these patients have been reported elsewhere (31). Briefly, 77.1% (N=279) of the subjects were female and 87.0% (N=315) were white. The mean age of the subjects was 27 years (SD=6.3), their mean socioeconomic status was 3.3 (SD=1.5) (where 1=highest and 5=lowest), and their mean GAF score was 39.8 (SD=7.8) (indicating major impairment in several areas, such as work or school, family relations, judgment, thinking, or mood). In terms of past treatment, the mean number of treatment modalities preceding index admission was 4.6 (SD=2.1).
At 2-year follow-up, 275 patients with borderline personality disorder and 67 comparison subjects with other axis II disorders were reinterviewed. At 4 years, 269 patients with borderline personality disorder and 64 comparison subjects with other axis II disorders were reinterviewed. At 6 years, 264 patients with borderline personality disorder and 63 comparison subjects with other axis II disorders were reinterviewed. Over 94% of surviving patients were reinterviewed at the three follow-up periods.
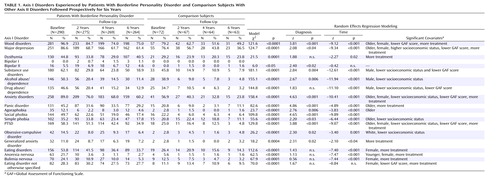
Table 1 shows the comorbid axis I disorders of patients with borderline personality disorder and those with other axis II disorders over 6 years of follow-up. At the stringent Bonferroni-corrected p level of 0.002, a significantly higher percentage of patients with borderline personality disorder than comparison subjects with other axis II disorders met criteria for mood disorders and anxiety disorders—specifically, panic disorder, social phobia, and posttraumatic stress disorder (PTSD). We found no significant between-group differences for substance use disorders, eating disorders, or specific forms of mood disorders.
When all subjects were considered together, the rates of 15 of the 20 axis I disorders studied declined significantly over time. The exceptions were dysthymia, bipolar II disorder, generalized anxiety disorder, and eating disorder not otherwise specified. (So few subjects met criteria for bipolar I disorder that convergence of a model was unsuccessful. Thus, there are no p levels for diagnosis or time for this condition.)
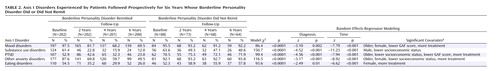
Table 2 shows the rates of selected comorbid axis I disorders experienced by the 202 patients whose borderline personality disorder ever remitted and the 73 patients whose borderline personality disorder never remitted (31). (Remission was defined as no longer meeting study criteria for borderline personality disorder at one or more follow-up periods.) At the stringent Bonferroni-corrected p level of 0.002, we found that a significantly higher percentage of patients whose borderline disorder never remitted than patients whose borderline disorder ever remitted met criteria for all types of axis I disorders studied except eating disorders. When all subjects were considered together, the rates of all types of axis I disorders studied declined significantly over time.
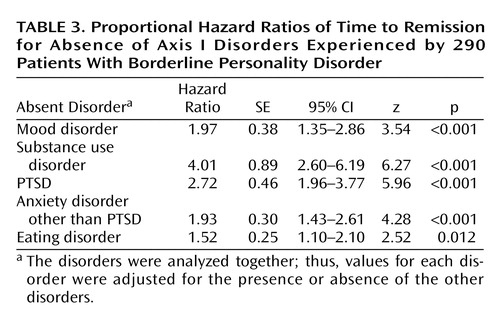
We next assessed time to remission for patients with borderline personality disorder who did not meet criteria for one or more of the following axis I disorders in at least one of the three follow-up periods: a mood disorder, a substance use disorder, PTSD, an anxiety disorder other than PTSD, or an eating disorder. Table 3 shows the hazard ratios for the absence of these disorders, which were analyzed together. As can be seen, the absence of each of these disorders significantly improved a patient’s chances of remission from borderline personality disorder. The absence of substance use disorders shortened time to remission by a factor of 4, absence of PTSD by a factor of about 2.5, absence of mood disorders and other anxiety disorders by a factor of almost 2, and absence of an eating disorder by a factor of 1.5.
Discussion
Three important findings have emerged from the results of this study. The first is that a high percentage of patients with borderline personality disorder continue to suffer from episodes of axis I disorders over time. Even by the time of the third follow-up, 75% of the patients with borderline personality disorder met criteria for a mood disorder, 60% for an anxiety disorder, 34% for an eating disorder, and 19% for a substance use disorder. In terms of specific disorders, 61% met criteria for major depression, 41% for dysthymia, 29% for panic disorder, 35% for PTSD, and 28% for eating disorder not otherwise specified. These rates represent substantial declines from baseline rates, but they also indicate that it is not uncommon for patients with borderline personality disorder to meet criteria for one or more axis I disorders over time.
In another report (40), we documented that a high percentage of these patients with borderline personality disorder continued to participate in both psychotherapy and pharmacotherapy over the course of the study. Even 5–6 years after their index admission, over 70% were in at least weekly individual therapy and taking at least one standing medication. In addition, polypharmacy was still very common. More specifically, at the third follow-up, over 50% of the patients with borderline personality disorder were taking two or more concurrent standing medications, over 35% were taking three or more, about 20% were taking four or more, and more than 10% were taking five or more. In terms of specific medications, 67% of patients with borderline personality disorder were taking an antidepressant during this period, 28% were taking an anxiolytic, 27% were taking an antipsychotic, and 22% were taking a mood stabilizer. Thus, the axis I disorders persisted or recurred despite a high likelihood that they were the object of aggressive treatment efforts.
The second important finding is that the ongoing prevalence of axis I disorders was strongly influenced by remission status from borderline personality disorder. More specifically, among patients whose borderline disorder remitted, the percentage who met criteria for different axis I disorders decreased over time, but the rates of four of the five types of axis I disorder studied remained relatively constant over time for patients whose borderline disorder did not remit. For patients whose borderline disorder remitted, rates of mood disorder decreased from a baseline high of 98% to 70% by the time of the third follow-up. Similar patterns of declining axis I psychopathology were found for substance use disorders (61% to 12%), PTSD (53% to 23%), other anxiety disorders (88% to 50%), and eating disorders (55% to 26%). In contrast, patients whose borderline disorder did not remit had relatively flat patterns of co-occurrence for four of the five types of disorder studied: mood disorders (about 90%), PTSD (about 70%), other anxiety disorders (about 90%), and eating disorders (about 50%). Only substance use disorders declined substantially for patients whose borderline disorder did not remit—from a baseline high of 64% to 41% at 6-year follow-up.
The relationship between remission from borderline personality disorder and the co-occurrence of one or more axis I disorders is unclear. It might be that patients whose borderline personality disorder is likely to remit have less axis I psychopathology initially. However, the baseline rates of all axis I disorders except PTSD were almost identical for patients whose borderline personality disorder did or did not remit. It might be that patients whose borderline personality disorder remits are more responsive to treatment. However, it is important to note that patients whose borderline disorder did not remit were significantly more likely than patients whose borderline disorder remitted to have been in individual therapy and to have been taking standing medications during the course of the study (40). Even during the third follow-up, over 90% of the patients whose borderline disorder did not remit (versus about 65% of those whose disorder remitted) were participating in both of these treatment modalities. It may also be that there is something fundamentally different about the temperament or neurobiology of the two groups of patients.
The third important finding is that the absence of a substance use disorder was a stronger predictor of remission from borderline personality disorder than the absence of any other type of disorder. This finding runs counter to clinical lore, which suggests that borderline personality disorder is most affected by the course of mood disorders or PTSD. However, this finding makes clinical sense because abusing alcohol and/or drugs could easily lead to greater impairment in all four core sectors of borderline psychopathology: decreased mood, heightened distrust, increased impulsivity, and even more turbulent relationships. It is also consistent with the results of earlier studies showing that substance use disorders impede remission from major depression and bipolar disorder (41, 42).
This finding also suggests that substance use disorders co-occurring with borderline personality disorder should be the main focus or at least one of the main foci of treatment, although it is not clear what treatment is most effective. A recent study (43) suggested that dialectical behavior therapy, a psychosocial treatment designed by Linehan specifically for patients with borderline personality disorder, is more effective for women with borderline personality disorder and opioid dependence than a 12-step program plus the supportive strategy of validation.
The most important limitation of the current study is that the entire study group of patients with borderline personality disorder were recruited as very disturbed inpatients. To what extent these results would generalize to never-hospitalized outpatients is unclear. The naturalistic nature of the current study also limits what can be inferred about the effect of treatment on the course of comorbid axis I disorders because hundreds of nonrandomly assigned mental health professionals provided the outpatient care for these patients.
Further studies are needed to determine if the current study’s findings can be replicated. Additionally, new treatments aimed at the special needs of substance-abusing patients with borderline personality disorder who do not respond to dialectical behavior therapy should be developed and their efficacy tested.
Taken together, the results of this study suggest that axis I disorders co-occur over time less commonly with initially severe borderline personality disorder, particularly for borderline disorder that remits over time. The findings also suggest that substance use disorders are the axis I disorders most closely associated with the failure to achieve symptomatic remission from borderline personality disorder.
 |
 |
 |
Received Oct. 9, 2003; revision received Jan. 20, 2004; accepted March 10, 2004. From the Laboratory for the Study for Adult Development, McLean Hospital, and the Department of Psychiatry, Harvard Medical School. Address reprint requests to Dr. Zanarini, McLean Hospital, 115 Mill St., Belmont, MA 02478; [email protected] (e-mail). Supported by NIMH grants MH-47588 and MH-62169.
1. Zanarini MC, Gunderson JG, Frankenburg FR: Axis I phenomenology of borderline personality disorder. Compr Psychiatry 1989; 30:149–156Crossref, Medline, Google Scholar
2. Oldham JM, Skodol AE, Kellman HD, Hyler SE, Doidge N, Rosnick L, Gallaher PE: Comorbidity of axis I and axis II disorders. Am J Psychiatry 1995; 152:571–578Link, Google Scholar
3. Zimmerman M, Mattia JL: Axis I diagnostic comorbidity and borderline personality disorder. Compr Psychiatry 1999; 40:245–252Crossref, Medline, Google Scholar
4. Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, Reynolds V: Axis I comorbidity of borderline personality disorder. Am J Psychiatry 1998; 155:1733–1739Link, Google Scholar
5. McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, Zanarini MC, Stout RL: The Collaborative Longitudinal Personality Disorders Study: baseline Axis I/II and II/II diagnostic co-occurrence. Acta Psychiatr Scand 2000; 102:256–264Crossref, Medline, Google Scholar
6. Grinker RR, Werble W, Drye R: The Borderline Syndrome. New York, Basic Books, 1968Google Scholar
7. Werble B: Second follow-up study of borderline patients. Arch Gen Psychiatry 1970; 23:3–7Crossref, Medline, Google Scholar
8. Gunderson JG, Carpenter WT Jr, Strauss JS: Borderline and schizophrenic patients: a comparative study. Am J Psychiatry 1975; 132:1257–1264Link, Google Scholar
9. Carpenter WT, Gunderson JG: Five year follow-up comparison of borderline and schizophrenic patients. Compr Psychiatry 1977; 18:567–571Crossref, Medline, Google Scholar
10. Pope HG, Jonas JM, Hudson JI, Cohen BM, Gunderson JG: The validity of DSM-III borderline personality disorder. Arch Gen Psychiatry 1983; 40:23–30Crossref, Medline, Google Scholar
11. Akiskal HS, Chen SE, Davis GC, Puzantian VR, Kashgarian M, Bolinger JM: Borderline: an adjective in search of a noun. J Clin Psychiatry 1985; 46:41–48Medline, Google Scholar
12. Barasch A, Frances A, Hurt S, Clarkin J, Cohen S: Stability and distinctness of borderline personality disorder. Am J Psychiatry 1985; 142:1484–1486Link, Google Scholar
13. Perry JC, Cooper SH: Psychodynamics, symptoms, and outcome in borderline and antisocial personality disorders and bipolar type II affective disorder, in The Borderline: Current Empirical Research. Edited by McGlashan TH. Washington, DC, American Psychiatric Press, 1985, pp 19–41Google Scholar
14. Nace EP, Saxon JJ, Shore N: Borderline personality disorder and alcoholism treatment: a one-year follow-up study. J Stud Alcohol 1986; 47:196–200Crossref, Medline, Google Scholar
15. Tucker L, Bauer SF, Wagner S, Harlam D, Sher I: Long-term hospital treatment of borderline patients: a descriptive outcome study. Am J Psychiatry 1987; 144:1443–1448Link, Google Scholar
16. Modestin J, Villiger C: Follow-up study on borderline versus nonborderline personality disorders. Compr Psychiatry 1989; 30:236–244Crossref, Medline, Google Scholar
17. Links PS, Mitton JE, Steiner M: Predicting outcome for borderline personality disorder. Compr Psychiatry 1990; 31:490–498Crossref, Medline, Google Scholar
18. Links PS, Heslegrave RJ, Mitton JE, Van Reekum R, Patrick J: Borderline psychopathology and recurrences of clinical disorders. J Nerv Ment Dis 1995; 183:582–586Crossref, Medline, Google Scholar
19. Mehlum L, Friis S, Irion T, Johns S, Karterud S, Vaglum P, Vaglum S: Personality disorders 2–5 years after treatment: a prospective follow-up study. Acta Psychiatr Scand 1991; 84:72–77Crossref, Medline, Google Scholar
20. Stevenson J, Meares R: An outcome study of psychotherapy for patients with borderline personality disorder. Am J Psychiatry 1992; 149:358–362Link, Google Scholar
21. Linehan MM, Heard HL, Armstrong HF: Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Arch Gen Psychiatry 1993; 50:971–974Crossref, Medline, Google Scholar
22. Sandell R, Alfredsson E, Berg M, Crafoord K, Lagerlof A, Arkel I, Cohn T, Rasch B, Rugolska A: Clinical significance of outcome in long-term follow-up of borderline patients at a day hospital. Acta Psychiatr Scand 1993; 87:405–413Crossref, Medline, Google Scholar
23. Antikainen R, Hintikka J, Lehtonen J, Koponen H, Arstila A: A prospective three-year follow-up study of borderline personality disorder inpatients. Acta Psychiatr Scand 1995; 92:327–335Crossref, Medline, Google Scholar
24. Najavits LM, Gunderson JG: Better than expected: improvements in borderline personality disorder in a 3-year prospective outcome study. Compr Psychiatry 1995; 36:296–302Crossref, Medline, Google Scholar
25. Senol S, Dereboy C, Yuksel N: Borderline disorder in Turkey: a 2- to 4-year follow-up. Soc Psychiatry Psychiatr Epidemiol 1997; 32:109–112Crossref, Medline, Google Scholar
26. Plakun EM, Burkhardt PE, Muller JP: 14-year follow-up of borderline and schizotypal personality disorders. Compr Psychiatry 1985; 26:448–455Crossref, Medline, Google Scholar
27. McGlashan TH: The Chestnut Lodge follow-up study, III: long-term outcome of borderline personalities. Arch Gen Psychiatry 1986; 43:20–30Crossref, Medline, Google Scholar
28. Stone MH: The Fate of Borderline Patients. New York, Guilford, 1990Google Scholar
29. Paris J, Brown R, Nowlis D: Long-term follow-up of borderline patients in a general hospital. Compr Psychiatry 1987; 28:530–536Crossref, Medline, Google Scholar
30. Paris J, Zweig-Frank H: A 27-year follow-up of patients with borderline personality disorder. Compr Psychiatry 2001; 42:482–487Crossref, Medline, Google Scholar
31. Zanarini MC, Frankenburg FR, Hennen J, Silk KR: The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder. Am J Psychiatry 2003; 160:274–283Link, Google Scholar
32. Zimmerman M, Mattia JL: Psychiatric diagnosis in clinical practice: is comorbidity being missed? Compr Psychiatry 1999; 40:182–191Crossref, Medline, Google Scholar
33. Spitzer RL, Williams JBW, Gibbon M, First MB: The Structured Clinical Interview for DSM-III-R (SCID), I: history, rationale, and description. Arch Gen Psychiatry 1992; 49:624–629Crossref, Medline, Google Scholar
34. Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL: The Revised Diagnostic Interview for Borderlines: discriminating BPD from other Axis II disorders. J Personal Disord 1989; 3:10–18Crossref, Google Scholar
35. Zanarini MC, Frankenburg FR, Chauncey DL, Gunderson JG: The Diagnostic Interview for Personality Disorders: inter-rater and test-retest reliability. Compr Psychiatry 1987; 28:467–480Crossref, Medline, Google Scholar
36. Zanarini MC, Frankenburg FR, Vujanovic AA: The inter-rater and test-retest reliability of the Revised Diagnostic Interview for Borderlines (DIB-R). J Personal Disord 2002; 16:270–276Crossref, Medline, Google Scholar
37. Zanarini MC, Frankenburg FR: Attainment and maintenance of reliability of axis I and II disorders over the course of a longitudinal study. Compr Psychiatry 2001; 42:369–374Crossref, Medline, Google Scholar
38. Greene WH: Econometric Analysis, 4th ed. Upper Saddle River, NJ, Prentice-Hall, 2000, pp 212–237Google Scholar
39. Allison PD: Event History Analysis: Regression for Longitudinal Event Data. Newbury Park, Calif, Sage Publications, 1984, pp 14–22Google Scholar
40. Zanarini MC, Frankenburg FR, Hennen J, Silk KR: Mental health service utilization by borderline personality disorder patients and Axis II comparison subjects followed prospectively for six years. J Clin Psychiatry 2004; 65:28–36Crossref, Medline, Google Scholar
41. Hasin DS, Tsai WY, Endicott J, Mueller TI, Coryell W, Keller M: Five-year course of major depression: effects of comorbid alcoholism. J Affect Disord 1996; 41:63–70Crossref, Medline, Google Scholar
42. Strakowski SM, DelBello MP, Fleck DE, Arndt S: The impact of substance abuse on the course of bipolar disorder. Biol Psychiatry 2000; 48:477–485Crossref, Medline, Google Scholar
43. Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welsh SS, Heagerty P, Kivlahan DR: Dialectical behavioral therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug Alcohol Depend 2002; 67:13–26Crossref, Medline, Google Scholar



