Relationship Between Multiple Forms of Childhood Maltreatment and Adult Mental Health in Community Respondents: Results From the Adverse Childhood Experiences Study
Abstract
OBJECTIVE: This study examined the prevalence of a history of various combinations of childhood maltreatment types (physical abuse, sexual abuse, and witnessing of maternal battering) among adult members of a health maintenance organization (HMO) and explored the relationship with adult mental health of the combinations of types of childhood maltreatment and emotional abuse in the childhood family environment. METHOD: A total of 8,667 adult members of an HMO completed measures of childhood exposure to family dysfunction, which included items on physical and sexual abuse, witnessing of maternal battering, and emotional abuse in the childhood family environment. The adults’ current mental health was assessed by using the mental health scale of the Medical Outcomes Study 36-item Short-Form Health Survey. RESULTS: The prevalences of sexual abuse, physical abuse, and witnessing of maternal violence were 21.6%, 20.6%, and 14.0%, respectively, when the maltreatment types were considered separately. Among respondents reporting any of the maltreatment types, 34.6% reported more than one type of maltreatment. Lower mean mental health scores were associated with higher numbers of abuse categories (mean=78.5, 75.5, 72.8, and 69.9 for respondents with no, one, two, and three abuse types, respectively). Both an emotionally abusive family environment and the interaction of an emotionally abusive family environment with the various maltreatment types had a significant effect on mental health scores. CONCLUSIONS: Childhood physical and sexual abuse, as well as witnessing of maternal battering, were common among the adult members of an HMO in this study. Among those reporting any maltreatment, more than one-third had experienced more than one type of maltreatment. A dose-response relation was found between the number of types of maltreatment reported and mental health scores. In addition, an emotionally abusive family environment accentuated the decrements in mental health scores. Future research examining the effects of childhood maltreatment on adult mental health should include assessments of a wide range of abusive experiences, as well as the family atmosphere in which they occur.
Although much is known about both the prevalence and consequences of various types of childhood maltreatment, few studies have estimated the occurrence of multiple abuse types within individuals (1, 2). Instead, research has focused on either physical or sexual abuse or, more recently, emotional abuse or witnessing of interparental violence (3). In studies where various forms of abuse have been assessed simultaneously, the prevalence of multiple categories of maltreatment has rarely been reported. Some researchers have reported only selected prevalences of overlapping abuse types (4), whereas others have stated that overlap occurs frequently, without reporting the percentages of subjects with co-occurring types of abuse (5).
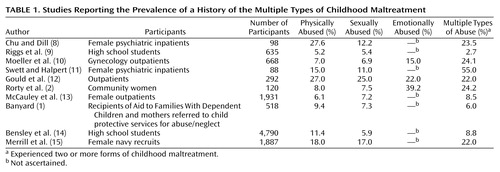
The studies that have calculated the co-occurrence of multiple categories of abuse have found that it is indeed very common. Research analyzing data from verified cases of victimization in children has reported low prevalences for single types of maltreatment, typically less than 10% of all child abuse cases (6, 7), and have instead found that the majority of these children have been abused in multiple ways. Multicategory abuse rates among adults and adolescents vary widely depending on the characteristics of the study sample. Table 1 lists 10 studies published in 1990 or later that have reported the prevalence of the co-occurrence of multiple types of maltreatment (1, 2, 8–15). In these studies, the highest prevalence of multicategory abuse was found among female psychiatric inpatients (11); the lowest prevalence was reported for a sample of high school students (9).
Studies that focus on a single type of abuse may suffer from two methodological limitations. First, they may assume the absence of other forms of maltreatment among comparison subjects and thus not assess other types of abuse. Second, participants classified as “abused” may have heterogeneous abuse experiences, ranging from a single incident to chronic long-term victimization. In studies that are subject to the first limitation, between-group differences may be minimized; in those subject to the second limitation, within-group variability may be increased. Both misclassification biases have the potential of reducing the probability of detecting significant outcomes of maltreatment.
Although the effect of the co-occurrence of multiple categories of maltreatment on psychological health and well-being has often been overlooked, available data indicate that the effects are negatively related to the number of abuse types experienced. Felitti et al. (16) reported a dose-response relationship between the number of indicators of childhood maltreatment or family dysfunction and a broad range of health outcomes among adult patients in a health maintenance organization (HMO). That is, as the number of negative experiences increased, poorer health was reported. Similarly, in a community sample of women, Mullen et al. (17) found poorer mental health among women reporting more than one type of abuse, compared to those reporting a single type.
Limited information is available to determine whether certain combinations of maltreatment are associated with poorer outcomes. In one of the few studies examining this question, Ney et al. (7) found that children who reported a combination of neglect, physical abuse, and verbal abuse expressed the most negative outlook on life, compared to those with other combinations of abuse types. Swett and Halpert (11) found that female psychiatric inpatients who reported only physical abuse or both physical and sexual abuse scored significantly higher on a measure of dissociation than those who reported no abuse or only sexual abuse.
Most of the relevant research has contrasted persons reporting one type of abuse with those reporting another but has rarely considered the joint effects of multicategory abuse. For instance, Briere and Runtz (5) found that childhood physical abuse was associated with aggressive behavior, sexual abuse with maladaptive sexual conduct, and emotional abuse with low self-esteem. Hart et al. (18) reported that sexually abused adolescent inpatients in a psychiatric unit were rated more socially defiant by staff members than were physically abused or nonabused inpatients.
Emotional abuse and witnessing of interparental violence have only recently been recognized as distinct forms of maltreatment (3, 19). Some researchers have suggested that emotional abuse is inherent in all forms of maltreatment and cannot be disentangled from other types of abuse (20). Other investigators have demonstrated that emotional abuse can and does occur independently of other abuse types (21, 22). We believe that an emotionally abusive family environment interacts with abusive acts to amplify the effects associated with maltreatment.
Some researchers have suggested that standardizing the classification of maltreatment is critical to understanding the effects of abuse. Manly et al. (23) and other investigators have recommended that scientists develop a systematic method of describing abuse experiences in order to tease apart differences in outcomes that may be due to specific interactions between maltreatment types. But to better understand differences in abuse outcomes, assessment of the quality of the childhood family environment may also be necessary. Chaotic, emotionally abusive, or neglectful family situations have been implicated as the real culprit in certain abuse outcomes (24–26). In contrast to individual abusive acts, such as an episode of sexual abuse or a severe beating, these family atmospheres may be better described as a continuous undercurrent that may accompany abuse.
In addition to neglecting the effect of family climate, most studies have not had enough subjects to estimate the prevalence of maltreatment combinations in a nonclinical sample. Further, although gender differences in the types of maltreatment experienced are well known, little information is available about multicategory abuse reported by men or about the co-occurrence of childhood abuse in men, compared with women.
In this report, we describe the prevalence of self-reported multicategory childhood maltreatment in a large epidemiological research project undertaken to assess the long-term effects of a variety of childhood stressors on adult health problems. We then examine the relationship between combinations of maltreatment types and adult mental health. We theorized that multicategory maltreatment would lead to greater decrements in mental health in a dose-response fashion, compared to single-category abuse. Further, we hypothesized that emotional abuse would heighten the effects of abusive acts such as physical and sexual abuse, resulting in lower mental health scores independent of and in combination with the abuse type.
The data were derived from the Adverse Childhood Experiences Study, an investigation that is being conducted at a large, metropolitan HMO to examine the associations between childhood maltreatment, family dysfunction, and adult health outcomes (16).
Method
Participants
HMO members undergoing a complete physical examination completed the Medical Outcomes Study 36-item Short-Form Health Survey (27) before their examination. One week later, they received a family health questionnaire (described in the next section) by mail. Of the 13,494 HMO members who had undergone a complete physical examination over a 1-year period during this phase of the study, 8,667 returned the questionnaire, for a response rate of 64%. Compared with nonrespondents, respondents were younger, more likely to be women, and less likely to be members of an ethnic minority group (28). Women made up 54.2% of the respondents. The average age was 55 years (range=19–97). Almost three-fourths (73.7%) of the respondents were white, with Hispanic (10.9%), Asian (8.0%), and African American (4.3%) respondents accounting for most of the remainder. More than 75% of the respondents had some college education. The analysis of the relationship between childhood maltreatment and current mental health was based on data from 7,505 respondents (85.6%) for whom a completed Medical Outcomes Study 36-item Short-Form Health Survey was available.
The Adverse Childhood Experiences study was approved by the institutional review boards of Kaiser Permanente, Emory University, and the Office of Protection From Research Risks, National Institutes of Health. Potential participants were sent letters that accompanied the Adverse Childhood Experiences study questionnaire informing them that their participation was voluntary and that their answers would be held in strictest confidence and would never become part of their medical record.
Measures
Family health history
Participants completed a 162-item family health history questionnaire that included questions about childhood abuse and exposure to family dysfunction, as well as current health behaviors and conditions. Items about various types of childhood maltreatment were adapted from other widely used and validated tests.
Childhood sexual abuse was assessed with four categorical questions adapted from a questionnaire used by Wyatt (29) that covered fondling, attempted intercourse, and intercourse. An affirmative answer to any of the four items resulted in the respondent being classified as sexually abused.
Childhood physical abuse was assessed with two items adapted from the Conflict Tactics Scale (30). Respondents who indicated that they had been pushed, grabbed, shoved, slapped, or had something thrown at them “often” or “very often” or who indicated that they had been hit so hard that they had marks or were injured “once” or “more than once” were considered victims of childhood physical abuse.
Being a witness of maternal battering was assessed with four items adapted from the Conflict Tactics Scale. Respondents were considered to have witnessed maternal battering if their answers indicated that the respondent had witnessed his or her mother “sometimes” or more often being pushed, grabbed, or slapped or having something thrown at her or had witnessed more serious violence (the mother being kicked, bit, hit with a fist or something hard, repeatedly hit over at least a few minutes, threatened with a knife or gun, or hurt with a knife or shot) once or more than once.
The intensity of emotional abuse in the childhood family environment was assessed with the emotional abuse subscale of the short form of the Childhood Trauma Questionnaire (21). The family health questionnaire incorporated the 5-item scale, which provides a continuous, rather than dichotomous, measure of emotional abuse. Higher scores indicate more emotional abuse. In this group of respondents, Cronbach’s alpha of 0.87 for internal consistency was obtained for this scale.
Mental health measure
The mental health scale of the Medical Outcomes Study 36-item Short-Form Health Survey (27) was used to assess current mental health status. Consisting of five items, this scale measures both depression and anxiety. Higher scores indicate better mental health. Cronbach’s alpha of 0.73 for internal consistency was obtained in this group of respondents.
Group Assignment
Respondents were assigned to one of seven mutually exclusive groups on the basis of the assessment of their maltreatment experiences across abuse types. Three groups consisted of individuals who reported only a single type of maltreatment: childhood sexual abuse, childhood physical abuse, or witnessing of maternal battering. Two groups were formed from respondents who indicated two abuse types: 1) those who reported both childhood physical and sexual abuse and 2) those who reported witnessing of maternal battering and either childhood sexual or physical abuse. In the second group, the sexual and physical abuse types were combined because a low number of respondents had witnessed maternal battering and had also experienced one of the two other types of abuse. A sixth group consisted of those who reported all three types of maltreatment (sexual abuse, physical abuse, and witnessing of maternal battering). The final group was made up of individuals who did not report any type of maltreatment. The intensity of emotional abuse in the childhood family environment was assessed within each abuse classification.
To test whether a dose-response relation exists between adverse childhood experiences and current mental health, respondents were reclassified by the number of abuse categories they experienced (range=0–3). The number of abuse categories was used as an ordinal variable for further analysis of abuse effects.
Analyses
Chi-square tests and t tests of proportions were used to determine whether the prevalences of abuse and abuse combinations differed by gender. Analyses of variance (ANOVAs) were performed to test for differences in current mental health by type of abuse, separately for men and women, as well as to determine the independent contribution to mental health of emotional abuse in the family environment.
Results
Prevalences of Single and Multiple Categories of Childhood Maltreatment
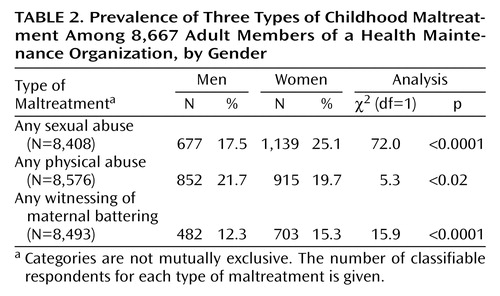
The prevalences of childhood sexual abuse, physical abuse, and witnessing of maternal battering were 21.6% (N=1,816 of 8,408), 20.6% (N=1,767 of 8,576), and 14.0% (N=1,185 of 8,493), respectively. Table 2 shows the prevalences for the three dichotomous maltreatment classifications by gender. Highly significant gender differences were found for each maltreatment type. Women reported significantly higher prevalences of childhood sexual abuse and witnessing of maternal battering than men. Childhood physical abuse was reported significantly more often by men.
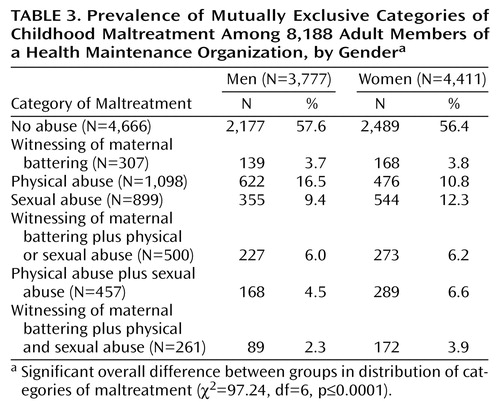
When abuse types were considered jointly, a somewhat different picture emerged. Table 3 presents the prevalences of each of the seven mutually exclusive abuse categories by gender. Among the 25.1% of women who reported any childhood sexual abuse, more than half (13.5%) also reported at least one additional form of abuse. Similarly, among the 21.7% of men who reported childhood physical abuse, about half (10.8%) also reported childhood sexual abuse, witnessing of maternal battering, or both. Prevalence rates of childhood sexual abuse remained significantly higher for women (12.3% versus 9.4% for men), as did childhood physical abuse prevalences for men (16.5% versus 10.8% for women). In the analyses based on the mutually exclusive abuse classifications, no significant difference by gender was found for witnessing of maternal battering. In two of the three multicategory abuse groups (childhood physical and sexual abuse, witnessing of maternal battering and both childhood physical and sexual abuse), women reported significantly higher prevalences than did men. No differences in prevalence by gender were found for no abuse, witnessing of maternal battering, and witnessing of maternal battering plus either childhood physical or sexual abuse.
Emotional Abuse in the Childhood Family Environment
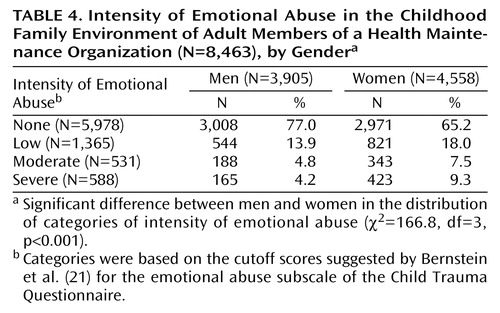
Women reported a significantly poorer emotional abuse climate in the family than men (mean=8.4, SD=4.5 versus mean=7.3, SD=3.5) (t=–12.9, df=8,460, p<0.001). We classified participants into four groups based on the cutoff scores for intensity levels of emotional abuse suggested by Bernstein et al. (21). As shown in Table 4, substantially higher percentages of women reported the presence of a low through severe intensity of emotional abuse in the family environment (χ2=166.8, df=3, N=8,463, p<0.001).
Adult Mental Health
Decrements in the mental health score occurred in a dose-response manner as the number of abuse types increased (Figure 1). The presence of emotional abuse accentuated this effect; generally, as the intensity of emotional abuse within each category increased, mental health scores declined. There were two exceptions, however. Among those who experienced no childhood sexual or physical abuse and did not witness maternal battering, respondents who reported severe emotional abuse had better mental health (mean mental health score=76.0, SD=15.6) than respondents with low (mean=73.1, SD=16.3) or moderate (mean=69.5, SD=18.7) emotional abuse. Among respondents reporting all three types of abuse, moderate emotional abuse was associated with a slightly higher mental health score than low emotional abuse (mean=73.9, SD=15.0, and mean=72.2, SD=16.1, respectively).
For all respondents, the mean mental health score obtained from the Short-Form Health Survey was 76.6 (SD=16.2). Gender and age were significantly related to mental health score, but no age-by-gender interaction occurred. Men had significantly higher mental health scores than women (mean=78.8, SD=15.5, versus mean=74.8, SD=16.6) (t=10.7, df=7,404, p<0.001). Mental health scores increased with age in both genders (r=0.11, N=7,408, p<0.01).
Gender-specific ANOVAs for the mental health score were carried out to test the association between the mutually exclusive abuse classifications and mental health, with age as a covariate. For men, significant main effects for abuse type (F=2.7, df=6, 3,209, p<0.02) and intensity of emotional abuse (F=20.6, df=3, 3,209, p<0.001) were obtained, as well as a significant interaction between abuse type and intensity of emotional abuse (F=2.1, df=18, 3,209, p<0.003). Among women, a significant main effect for intensity of emotional abuse (F=4.7, df=3, 3,667, p<0.003) and a significant interaction between abuse type and intensity of emotional abuse (F=2.4, df=18, 3,667, p<0.001) were obtained, but the main effect for abuse type only approached significance (F=2.2, df=6, 3,667, p<0.06).
To further evaluate the dose-response hypothesis, the maltreatment classifications were combined to form four categories: no abuse and one, two, or three types of abuse. An ANOVA with age and gender as covariates was conducted by using this ordinal variable as a predictor of mental health. As hypothesized, significant main effects were found for the number of reported types of abuse (F=3.07, df=3, 6,914, p<0.03), the intensity of emotional abuse (F=15.73, df=3, 6,914, p<0.001), and the interaction between the number of abuse types and the intensity of emotional abuse (F=3.07, df=9, 6,914, p<0.001).
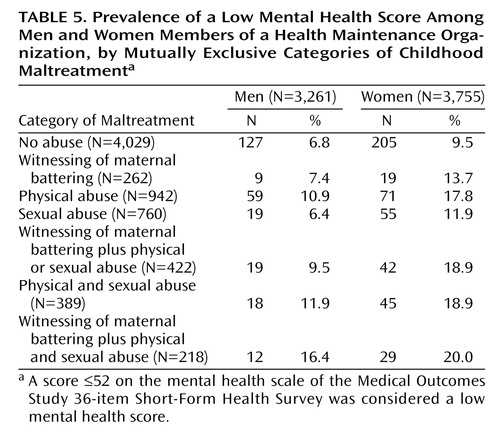
We assessed the effect of abuse on mental health by respondents into two groups on the basis of their score on the mental health scale of the Medical Outcomes Study 36-item Short-Form Health Survey (≤52 and >52). Persons scoring ≤52 have been found to have a high probability of psychiatric disorder (31). Table 5 shows the number and proportion of respondents in each abuse category who scored ≤52. We performed logistic regression analyses separately by gender to test for the relation between abuse category and poor mental health. The overall test of trend for abuse category was significant (odds ratio=1.72, 95% confidence interval=1.65–1.78, p<0.001). The proportion of respondents with a score ≤52 increased in a dose-response fashion from the no abuse group to the multicategory abuse groups, with the exception of the childhood sexual abuse group. Among men who had a score ≤52, the proportion who reported witnessing of maternal battering plus sexual and physical abuse was 2.4 times that for those who reported no abuse. Among women with a score ≤52, the proportion who reported all three types of maltreatment was 2.1 times that for those who reported no abuse.
Discussion
Four notable attributes of this study distinguish it from previous work in this nascent research area. First, this study included more than 8,000 participants, a fourfold increase over the number of participants in the largest prior study of multicategory abuse. Second, the data were derived from community respondents and thus provide a better estimate of the prevalence of multicategory maltreatment in the population than can be obtained from clinical studies. Third, both men and women were included in the study. To our knowledge, this study was only the second study to assess the long-term effects of multicategory childhood abuse in men. Finally, to our knowledge, this is the first study to include the assessment of witnessing of maternal battering in childhood as a category of maltreatment along with other more standard types of childhood abuse.
It is noteworthy that about 43% of the participants met the criteria for at least one of the six separate abuse types or combinations assessed in this study. Multicategory abuse was common; of the 43% of participants reporting any abuse, 34.6% reported experiencing at least two types of maltreatment in childhood. Thus, recognizing the overlap of abuse is important to understanding the clustering of childhood abuse and the effect of cumulative stressors on later-life adjustment.
Because of the age and source of the respondents and the operational definitions and categories of maltreatment used in this study, there are considerable differences between this study and the few other studies that have estimated multicategory maltreatment. Nonetheless, the prevalence estimates obtained in this study appear to be similar to those from prior research. For example, 6.6% of women in the present study reported the co-occurrence of physical and sexual abuse, which is similar to reports in other studies involving community participants (9, 15). However, they were considerably lower than those obtained in clinical studies (8, 11).
New insights into the nature of the maltreatment of men were obtained. As in previous research (32), about 25% of the men in this study reported childhood physical abuse. However, more than one-third of these respondents also reported at least one other form of abuse; the most common combination among men was childhood physical abuse and childhood sexual abuse (6.0%). In contrast, 6.6% of the women participants reported both childhood physical abuse and childhood sexual abuse. When treatment categories were collapsed, 12.8% of the men versus 16.7% of the women reported multicategory abuse (χ2=26.7, df=2, N=8,191, p<0.001). Thus, although men may experience multicategory abuse somewhat less frequently than women, multicategory abuse still has a substantial prevalence among men.
In addition to examining the co-occurrence of different forms of childhood maltreatment, we assessed the long-term mental health consequences of such victimization. An overall trend for poorer mental health as the number of abuse types increased was confirmed, implying that a dose-response relation is present. Although the mean differences in mental health scores between the abuse classifications were relatively small, these differences represent a real effect in terms of social functioning. According to Berwick et al. (31), a 3-point difference on the mental health scale of the Medical Outcomes Study 36-item Short-Form Health Survey is equivalent to the psychological distress of being fired or laid off from one’s job.
To better understand the contribution of childhood family environment to mental health later in life, we conceptualized family climate by assessing perceptions of emotional abuse, which allowed us to test our idea that the environment represents the “ground” against which the “figure” of abusive acts is experienced. Emotional abuse in the childhood family environment proved to have a significant main effect on adult mental health. In addition to its power as an independent predictor, emotional abuse served to heighten the effect of abusive acts. This relationship is compatible with the ecological approach (33) on which most contemporary models of maltreatment effects rely. By adjusting for emotional abuse in the family environment, large decrements in mental health scores (of more than 10 points) were obtained for both men and women (Figure 1).
Future research in this area should include consideration of specific mechanisms in family dynamics, such as attachment. For example, compensatory warmth by mothers with battering partners is a possible moderator of the effects of witnessing of interparental violence (34). Extrafamilial childhood sexual abuse that occurs in an otherwise loving and caring family environment is yet another example of the complexity of abusive acts. In these scenarios, a loving and warm childhood environment may mitigate the effects of other abusive experiences.
Limitations on the generalizability of these data exist. First, the respondents were drawn from HMO membership and may not be representative of persons without access to high-quality medical care. Second, use of a preventive health clinic resulted in overrepresentation of older respondents, because younger persons are less likely to seek out routine health screenings. The overwhelming majority of the participants were white and had at least some college education, hence additional studies should be performed to confirm these findings with more demographically diverse groups. Even higher abuse prevalences may have been obtained had a more diverse group of respondents been included. Nevertheless, the maltreatment prevalences obtained for the single abuse types were similar to those for other large, population-based groups (32, 35). However, no conclusions about the temporal sequence of abuse experiences could be drawn, because the breadth of the family health history did not allow collection of detailed information about when each type of abuse was experienced or the sequence in which it occurred.
Finally, this study was based on adults’ self-reports of childhood maltreatment, and we had no information about the accuracy of those reports. As such, our conclusions were based on reported, rather than confirmed, cases of childhood maltreatment. Studies that have examined the accuracy of retrospective reports have found that the validity of such reports differs on such dimensions as the objective specificity of the variable assessed or the affective state of the respondent (36, 37). It has been found that “researcher-defined” reports of child maltreatment (i.e., in which the researcher identifies particular behaviors, as was done in this study) result in higher rates of abuse than “self-defined” accounts (38). Even so, Widom and Shepard (39) found that researcher-defined reports of child physical abuse (i.e., child protective service reports), although characterized by considerable accuracy, still reflect some underreporting. Henry et al. (36) recommended using retrospective reports for testing hypotheses about the relative standing of individuals in a distribution rather than hypotheses about event frequencies or timing, as we have done here.
Mental health practitioners have long been aware of the findings this research has highlighted: that multicategory abuse in childhood is a common experience among those who have been abused. By accounting for the climate in which the abuse occurs, the wide range of outcomes within a seemingly homogenous group can be addressed. These results suggest that much of the earlier research in child abuse may be limited by reliance on reports of a single abuse type when multicategory abuse is the norm rather than the exception. In studies that compared those “abused” on a single abuse dimension to those who are “not abused,” between-group differences may have been compromised. Greater care in assessing and classifying persons with regard to a range of abusive experiences, as well as the climate in which it occurs, should produce results that better illuminate the effects of childhood victimization.
 |
 |
 |
 |
 |
Presented at the International Family Violence Conference held July 25–28, 1999, in Durham, N.H. Received July 5, 2001; revisions received Aug. 29 and Dec. 27, 2002; accepted March 17, 2003. From the Centers for Disease Control and Prevention; the University of Texas at Austin; and Kaiser Permanente, San Diego. Address reprint requests to Dr. Edwards, Centers for Disease Control and Prevention, Mailstop K-67, 4770 Buford Highway, NE, Atlanta, GA 30341; [email protected] (e-mail). Supported by cooperative agreement TS-44-10/11 between the Centers for Disease Control and Prevention and the Association of Teachers of Preventive Medicine and a grant from the Garfield Memorial Fund. This research was conducted in partial fulfillment of requirements for the first author’s doctoral degree. The authors thank Naomi Howard, Laura Gamble, and Matthew Sydney for assistance in collecting and preparing the data.
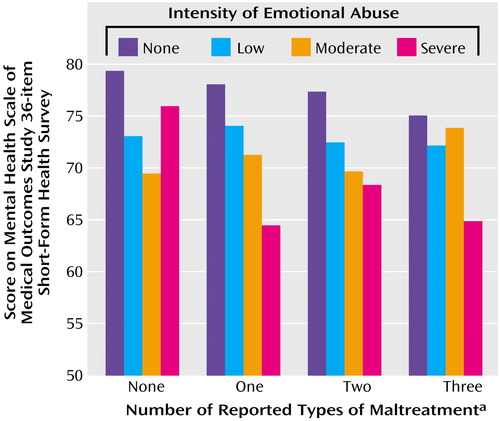
Figure 1. Mean Mental Health Score of Adult Members of a Health Maintenance Organization (N=6,932) Grouped by the Number of Reported Types of Childhood Maltreatment and Intensity of Emotional Abuse in the Childhood Family Environment
aThe three types of abuse considered in the analysis were childhood sexual abuse, childhood physical abuse, and witnessing of maternal battering.
1. Banyard V: Childhood maltreatment and the mental health of low-income women. Am J Orthopsychiatry 1999; 69:161–171Crossref, Medline, Google Scholar
2. Rorty M, Yager J, Rossotto E: Childhood sexual, physical, and psychological abuse in bulimia nervosa. Am J Psychiatry 1994; 151:1122–1126Link, Google Scholar
3. Holden GW, Geffner R, Jouriles EN (eds): Children Exposed to Marital Violence: Theory, Research, and Applied Issues. Washington, DC, American Psychological Association, 1998Google Scholar
4. Cavaiola AC, Schiff M: Behavioral sequelae of physical and/or sexual abuse in adolescents. Child Abuse Negl 1988; 12:181–188Crossref, Medline, Google Scholar
5. Briere J, Runtz M: Multivariate correlates of childhood psychological and physical maltreatment among university women. Child Abuse Negl 1988; 12:331–341Crossref, Medline, Google Scholar
6. McGee RA, Wolfe DA, Yuen SA, Wilson SK, Carnochan J: The measurement of maltreatment: a comparison of approaches. Child Abuse Negl 1995; 19:233–249Crossref, Medline, Google Scholar
7. Ney PG, Fung T, Wickett AR: The worst combinations of child abuse and neglect. Child Abuse Negl 1994; 18:705–714Crossref, Medline, Google Scholar
8. Chu JA, Dill DL: Dissociative symptoms in relation to childhood physical and sexual abuse. Am J Psychiatry 1990; 147:887–892Link, Google Scholar
9. Riggs S, Alario AJ, McHorney C: Health risk behaviors and attempted suicide in adolescents who report prior maltreatment. J Pediatr 1990; 116:815–821Crossref, Medline, Google Scholar
10. Moeller TP, Bachmann GA, Moeller JR: The combined effects of physical, sexual, and emotional abuse during childhood: long-term health consequences for women. Child Abuse Negl 1993; 17:623–640Crossref, Medline, Google Scholar
11. Swett C, Halpert M: Reported history of physical and sexual abuse in relation to dissociation and other symptomatology in women psychiatric inpatients. J Interpers Violence 1993; 8:545–555Crossref, Google Scholar
12. Gould DA, Stevens NG, Ward NG, Carlin AS, Sowell HS, Gustafson B: Self-reported childhood abuse in an adult population in a primary care setting: prevalence, correlates, and associated suicide attempts. Arch Fam Med 1994; 3:252–256Crossref, Medline, Google Scholar
13. McCauley J, Kern DE, Kolodner K, Dill L, Schroeder AF, DeChant HK, Ryden J, Derogatis LR, Bass EB: Clinical characteristics of women with a history of childhood abuse: unhealed wounds. JAMA 1997; 277:1362–1368Crossref, Medline, Google Scholar
14. Bensley LS, Van Eenwyk J, Spieker SJ, Schoder J: Self-reported abuse history and adolescent problem behaviors: I. antisocial and suicidal behaviors. J Adolesc Health 1999; 24:163–172Crossref, Medline, Google Scholar
15. Merrill LL, Newell CE, Thomsen CJ, Gold SR, Milner JS, Koss MP, Rosswork SG: Childhood abuse and sexual revictimization in a female Navy recruit sample. J Trauma Stress 1999; 12:211–225Crossref, Medline, Google Scholar
16. Felitti VJ, Anda RF, Nordenberg DF, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS: Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998; 14:248–258Crossref, Google Scholar
17. Mullen PE, Martin JL, Anderson JC, Romans SE, Herbison GP: The long-term impact of the physical, emotional, and sexual abuse of children: a community study. Child Abuse Negl 1996; 20:7–21Crossref, Medline, Google Scholar
18. Hart LE, Mader L, Griffith K, deMendonca M: Effects of sexual and physical abuse: a comparison of adolescent inpatients. Child Psychiatry Hum Dev 1989; 20:49–57Crossref, Medline, Google Scholar
19. Jaffe PG, Wolfe DA, Wilson SK: Children of Battered Women. Newbury Park, Calif, Sage Publications, 1990Google Scholar
20. Garbarino J, Guttman E, Seeley J: The Psychologically Battered Child. San Francisco, Jossey-Bass, 1986Google Scholar
21. Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J: Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry 1994; 151:1132–1136Link, Google Scholar
22. Claussen AH, Crittenden PM: Physical and psychological maltreatment: relations among types of maltreatment. Child Abuse Negl 1991; 15:5–18Crossref, Medline, Google Scholar
23. Manly JT, Cicchetti D, Barnett D: The impact of subtype, frequency, chronicity, and severity of child maltreatment on social competence and behavior problems. Dev Psychopathol 1994; 6:121–143Crossref, Google Scholar
24. Brock KJ, Mintz LB, Good GE: Differences among sexually abused and nonabused women from functional and dysfunctional families. J Couns Psychol 1997; 44:425–432Crossref, Google Scholar
25. Harter S, Alexander P, Neimeyer RA: Long-term effects of incestuous child abuse in college women: social adjustment, social cognition, and family characteristics. J Consult Clin Psychol 1988; 56:5–8Crossref, Medline, Google Scholar
26. Nash MR, Hulsey TL, Sexton MC, Harralson TL, Lambert W: Long-term sequelae of childhood sexual abuse: perceived family environment, psychopathology, and dissociation. J Consult Clin Psychol 1993; 61:276–283Crossref, Medline, Google Scholar
27. Ware JE Jr, Sherbourne CD: The MOS 36-Item Short-Form Health Survey (SF-36), I: conceptual framework and item selection. Med Care 1992; 30:473–483Crossref, Medline, Google Scholar
28. Edwards VJ, Anda RF, Nordenberg DF, Felitti VJ, Williamson DF: Factors affecting probability of response to a survey about childhood abuse. Child Abuse Negl 2001; 25:307–312Crossref, Medline, Google Scholar
29. Wyatt GE: The sexual abuse of Afro-American and white-American women in childhood. Child Abuse Negl 1985; 9:507–519Crossref, Medline, Google Scholar
30. Straus MA: Measuring intrafamily conflict and violence: the Conflict Tactics (CT) Scales. J Marriage Fam 1979; 41:75–88Crossref, Google Scholar
31. Berwick DM, Murphy JM, Goldman PA, Ware JE, Barsky AJ, Weinstein MC: Performance of a five-item mental health screening test. Med Care 1991; 29:169–176Crossref, Medline, Google Scholar
32. MacMillan HL, Fleming JE, Trocme N, Boyle MH, Wong M, Racine YA, Beardslee WR, Offord DR: Prevalence of child physical and sexual abuse in the community: results from the Ontario Health Supplement. JAMA 1997; 278:131–135Crossref, Medline, Google Scholar
33. Belsky J: Etiology of child maltreatment: a developmental-ecological analysis. Psychol Bull 1993; 114:413–434Crossref, Medline, Google Scholar
34. Ritchie KL, Holden GW: Parenting stress in low income battered and community women: effects on parenting behavior. Early Educ Dev 1998; 9:97–112Crossref, Google Scholar
35. Finkelhor D, Hotaling G, Lewis IA, Smith C: Sexual abuse in a national survey of adult men and women: prevalence, characteristics, and risk factors. Child Abuse Negl 1990; 14:19–28Crossref, Medline, Google Scholar
36. Henry B, Moffitt TE, Caspi A, Langley J, Silva PA: On the “remembrance of things past”: a longitudinal evaluation of the retrospective method. Psychol Assess 1994; 6:92–101Crossref, Google Scholar
37. Prescott A, Bank L, Reid JB, Knutson JF, Burraston BO, Eddy JM: Tthe veridicality of punitive childhood experiences reported by adolescents and young adults. Child Abuse Negl 2000; 24:411–423Crossref, Medline, Google Scholar
38. Silvern L, Waelde LC, Baughan B, Karyl J, Kaersvang LL: Two formats for eliciting retrospective reports of child sexual and physical abuse: effects on apparent prevalence and relationships to adjustment. Child Maltreat 2000; 5:236–250Crossref, Medline, Google Scholar
39. Widom CS, Shepard RL: Accuracy of adult recollections of childhood victimization: part 1. childhood physical abuse. Psychol Assess 1996; 8:412–421Crossref, Google Scholar



