Modification of DSM-IV Criteria for Depressed Preschool Children
Abstract
OBJECTIVE: This study compared the severity of depression in preschoolers diagnosed by standard versus modified DSM-IV criteria for major depression. METHOD: A group of 145 preschoolers and their caregivers underwent a diagnostic assessment for preschool children. A factor analysis of depressive symptoms from the group was performed to derive a depression severity score. Scores were compared among four groups: standard DSM-IV major depression, modified DSM-IV major depression, DSM-IV attention deficit hyperactivity disorder and/or oppositional defiant disorder, and no disorder. RESULTS: A hierarchy in severity emerged, with significant differences among all four groups. Preschoolers meeting standard criteria displayed the highest severity, followed by those who met modified criteria. Both depressed groups had significantly higher severity than the two comparison groups. CONCLUSIONS: Standard DSM-IV criteria captured the most severely affected preschoolers, missing a substantial proportion of children with potentially clinically significant but less severe symptoms who were captured by modified DSM-IV criteria.
Numerous longitudinal studies have now established that depression identified in children 6 and older is a chronic and relapsing disorder that has demonstrated continuity with the adult disorder (for a review, see Luby et al. [1]). These findings point to the importance of the earliest possible identification and intervention for major depressive disorder. The more urgent public health need for criteria to accurately identify depressive disorders in children before the age of 6 is underscored by a recent survey of prescribing trends indicating an alarming national increase in the off-label prescription of antidepressant medications to preschoolers for a variety of nonspecific conditions (2). In 1994 alone, 3,000 prescriptions for fluoxetine were written for infants under 12 months of age, highlighting the dangers and extremes of this trend (2). There are currently neither age-specific criteria nor any established indications to guide the accurate identification and pharmacological treatment of depression in preschoolers. Early investigations of major depressive disorder in preschoolers found few children who met formal DSM criteria, although many showed “concerning symptoms,” suggesting the need for modified criteria for young children (3).
The current analyses are a part of a larger investigation of the age-specific nosology of depressive disorders in preschool children. Content validity of developmentally modified DSM-IV criteria for major depressive disorder for preschoolers has been established (4). To investigate the validity of these criteria for preschool-age populations, an age-appropriate structured psychiatric interview that used developmental translations of specific DSM-IV symptoms of major depressive disorder was used. Examples of these translations included that behavioral changes in “activities and play” rather than “ work or school” were assessed and that “decisions” were described as “choices.” These modifications were necessary to assess the pertinent life experience of the young child. Furthermore, because preschool children have limited verbal skills, items that addressed preoccupation with death and suicidality were modified to account for the possibility that these symptoms might be manifested as persistent themes in play (in addition to the possibility that they might be verbally expressed). All other symptoms of depression were deemed applicable to preschoolers in their current form and were unchanged.
Preschoolers who met modified DSM-IV criteria for major depressive disorder had numerous associated markers of a clinically significant syndrome. These markers included a unique and stable symptom constellation and a greater family history of related disorders relative to both comparison groups (4). Notably, these young subjects also displayed significantly greater social impairment and more self-reported negative affect in an age-appropriate puppet interview relative to the comparison group with no DSM-IV disorder (4). A unique symptom constellation, family history, and stable course are established markers of the content validity of a clinical syndrome, according to the methods outlined by Robins and Guze (5), used in development of the DSM system. This preschool depressive syndrome was found to be characterized by a predominance of typical DSM-IV symptoms of depression, while “masked” symptoms, such as somatization, once theorized as central manifestations of early-onset depression, were also found but at lower frequencies (6).
The developmental translations of symptom states, as described, were applied in the assessment of all study subjects and used in the categorization of both depressed groups. However, the following changes to the DSM-IV criteria for major depressive disorder were used to define the group with modified DSM-IV major depressive disorder:
| 1. | The strict 2-week duration requirement was set aside. This meant that parents failed to endorse that their child was depressed “for nearly every day for 2 weeks or longer,” despite endorsing that their child often seemed sad or unhappy. The absence of a 2-week period of sustained depressed mood could be consistent with the greater normative fluctuation in affective state at this early stage of development (7). However, more detailed investigation of the duration of an episode of preschool depression is needed (4). | ||||
| 2. | The required five symptoms were present in all cases, except for two subjects who had only four symptoms but who both met core criteria for major depressive disorder (sadness/irritability and anhedonia were present). These children were included in the depressed group on the basis of the notion that the presence of both core criteria were clinically significant when they occurred in a preschool child. | ||||
Notably, 75% of the preschoolers with symptoms of depression and the associated markers of the clinical syndrome described (N=39), met modified criteria for major depressive disorder but failed to meet full standard criteria. The hypothesis of these analyses was that standard DSM-IV criteria captured only the most severely depressed preschoolers and missed a substantial proportion of children with clinically significant symptoms captured by the modified criteria.
Method
The study protocol was fully approved by the Washington University School of Medicine’s institutional review board. A group of 145 children between the ages of 3 years and 5 years and 6 months were recruited from pediatricians’ offices in the community and from a preschool mental health clinic. Children with symptoms of depression, those with symptoms of “disruptive behavioral disorders,” and those without symptoms were ascertained for study participation. After complete description of the study to the families, written informed consent was obtained from the guardians. Children and their primary caregivers were invited into the laboratory for a comprehensive assessment, during which a structured diagnostic interview, a version of the Diagnostic Interview Schedule for Children, Version IV (8) (Young-Child Diagnostic Interview Schedule for Children, Version IV [9]), was administered to caregivers about their children. Reliability of the Young-Child Diagnostic Interview Schedule for Children, Version IV, for use in young-child populations has been established (Compton et al., unpublished data). On the basis of parent reports on the Young-Child Diagnostic Interview Schedule for Children, Version IV, four groups were derived and compared for these analyses: 1) those who met developmentally modified DSM-IV criteria for major depressive disorder, 2) those who met standard DSM-IV criteria for major depressive disorder, 3) a non-mood-disordered psychiatric group of children with DSM-IV attention deficit hyperactivity disorder and/or oppositional defiant disorder, and 4) a group who did not meet criteria for any DSM-IV disorder (a comparison group without a disorder).
The parents were also interviewed about the family psychiatric history of mental disorders with the Family Interview for Genetic Studies (10). Independent measures of the child’s behavior and social development were also obtained with the Child Behavioral Checklist (11) and the Vineland Adaptive Behavior Socialization Scale (12), respectively. The children themselves were interviewed about their internal experience of mood states with an age-appropriate puppet interview, the Berkeley Puppet Interview—Symptom Scales, for which reliability and validity have been established (13, 14). Observational measures of the child’s emotional reactivity and parent-child interaction were also obtained but have not yet been coded for analyses. All assessments were performed by raters who were blind to the diagnostic status of the child.
To derive a formula for calculating weighted depression severity scores, principal-component analysis was performed on all core DSM-IV symptoms of depression (not including duration items) from the major depressive disorder module from the Young-Child Diagnostic Interview Schedule for Children, Version IV, across all four study groups. The purpose of this was to allow a quantitative determination of the relative importance of each symptom of depression to the diagnosis of DSM-IV major depressive disorder. Internal consistency of the major depressive disorder scale score from the Young-Child Diagnostic Interview Schedule for Children, Version IV, was examined by calculating Cronbach’s alpha coefficient to determine if individual symptoms of depression were correlated in the study population, as expected. Severity scores between the four diagnostic groups were then compared by using one-way analysis of variance (ANOVA). To control severity scores derived from factor analysis, we also examined group differences between summary scores for all Young-Child Diagnostic Interview Schedule for Children, Version IV, symptoms of major depressive disorder. ANOVAs were then performed on the summed scores over all four diagnostic groups. To further investigate any differences between modified and standard criteria for major depressive disorder, ANOVAs were performed on the measures that were used to establish content validity as dependent variables. These included ratings of family history of affective disorders according to scores on the Family Interview for Genetic Studies, impairment based on scores on the Vineland Adaptive Behavior Socialization Scale, and dimensional ratings of psychopathology according to the Child Behavioral Checklist. If homogeneity of variance was not satisfied, Kruskal-Wallis rank ANOVAs were performed.
Results
There were no significant group differences on any demographic factor among the four diagnostic groups, with the exception of family income (χ2=18.00, df=6, p<0.01), which was lower for both of the major depressive disorder groups than the two comparison groups.
Principal-component analysis yielded a one-component solution and was therefore useful for deriving weighted depression severity scores. Depression severity scores were then computed for each study subject by using each depression symptom from the Young-Child Diagnostic Interview Schedule for Children, Version IV, at its relative weight, as indicated by its factor score. Figure 1 displays the hierarchical differences in severity scores that emerged between diagnostic groups, illustrating that the group with a standard DSM-IV diagnosis of major depressive disorder had the highest severity scores. Kruskal-Wallis one-way ANOVAs demonstrated significant differences in severity scores among the four groups (χ2=102.03, df=3, p<0.001). Post hoc Mann-Whitney U tests revealed that the group with a standard DSM-IV diagnosis of major depressive disorder had significantly higher severity scores than the group with a modified DSM-IV diagnosis of major depressive disorder (Mann-Whitney U=76.0, p<0.001), while this group had significantly higher scores than the psychiatric comparison group (U=26.0, p<0.001) and the comparison group with no disorder (U=1.0, p<0.001). The psychiatric comparison group also had significantly higher scores than the comparison subjects with no disorder (U=760.0, p<0.01). Income did not significantly influence group differences in severity scores. A similar statistically significant hierarchy between groups was also found when the sum scores were compared. Cronbach’s alpha for all major depressive disorder items from the Young-Child Diagnostic Interview Schedule for Children, Version IV, was 0.85.
Despite significant differences on multiple group comparisons across all diagnostic groups, no differences were found between the groups with modified and standard DSM-IV diagnoses of major depressive disorder on measures of impairment or any of the outcome measures used to establish content validity: internalizing T scores from the Child Behavioral Checklist (F=41.77, df=3, 130, p<0.001; post hoc Scheffé test for standard versus modified DSM-IV major depressive disorder: p<0.45), externalizing T scores from the Child Behavioral Checklist (F=19.76, df=3, 130, p<0.001; post hoc Scheffé test for standard versus modified DSM-IV major depressive disorder: p<0.99), the Vineland Adaptive Behavior Socialization Scale (F=5.38, df=3, 135, p<0.01; post hoc Scheffé test for standard versus modified DSM-IV major depressive disorder: p<0.10), and affective disorders from the Family Interview for Genetic Studies (χ2=8.33, df=3, p<0.05; post hoc U test for standard versus modified DSM-IV major depressive disorder: U=175.5, p=0.12).
Discussion
Our findings demonstrate that modified DSM-IV criteria for major depressive disorder captured a group of preschoolers with numerous symptoms of depression, social impairment, and greater depression severity than psychiatric and healthy comparison groups. Also notable was that there were no significant differences in social impairment or other associated markers of a clinical syndrome (e.g., family history of related disorders and dimensional measures of psychopathology) between the children meeting modified versus standard DSM-IV criteria for major depressive disorder. The high internal consistency of symptoms of major depressive disorder (represented by Cronbach’s alpha) shows that these symptoms of depression clustered together in preschool subjects, as expected in a valid clinical syndrome. These findings lend further support for the content validity of the modified criteria, and, taken together with the previously established markers of clinical significance or content validity that characterized the entire group of depressed preschoolers, suggest that standard criteria for DSM-IV major depressive disorder captured only the most severely depressed preschoolers and missed a larger group (75%) of less severely (but potentially clinically depressed) children.
Future studies that comprehensively investigate the impairment, adaptive functioning, and longitudinal course of this group are needed and are now underway in our laboratory. These data are necessary before any conclusions can be drawn about whether the modified criteria represent a depressive prodrome, a subsyndrome, or a clinically significant depressive syndrome that warrants clinical intervention. Determining whether this preschool depressive syndrome is stable and continuous with prepubertal major depressive disorder is critical to establishing predictive validity and to adding necessary clarity to the definition of the syndrome in the preschool period.
Received Oct. 29, 2001; revision received Oct. 1, 2002; accepted Jan. 13, 2003. From the Department of Psychiatry, Washington University School of Medicine. Address reprint requests to Dr. Luby, Department of Psychiatry, Washington University School of Medicine, 660 S. Euclid Ave., Box 8134, St. Louis, MO 63110; [email protected] (e-mail). Supported by NIMH grant MH-01462 to Dr. Luby.
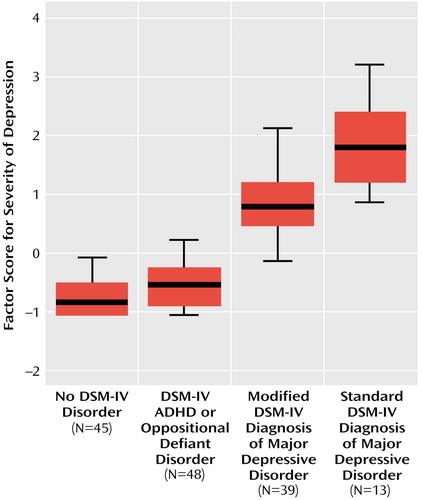
Figure 1. Depression Severity Scores for Preschoolers With DSM-IV Diagnoses of Depression, Preschoolers With Modified Diagnoses of Depression, and Two Comparison Groupsa
aA factor analysis of depressive symptoms for the entire study group was performed to derive a depression severity score. Severity scores were compared among the four subgroups.
1. Luby J, Todd R, Geller B: Outcome of childhood depressive syndromes: infancy to adolescence, in Mood Disorders Throughout the Lifespan. Edited by Shulan K, Tohen M, Kutcher S. New York, John Wiley & Sons, 1996, pp 83-100Google Scholar
2. Zito JM, Safer DJ, DosReis S, Gardner JF, Boles M, Lynch F: Trends in the prescribing of psychotropic medications to preschoolers. JAMA 2000; 283:1025-1030Crossref, Medline, Google Scholar
3. Kashani JH, Holcomb WR, Orvaschel H: Depression and depressive symptoms in preschool children from the general population. Am J Psychiatry 1986; 143:1138-1143Link, Google Scholar
4. Luby JL, Heffelfinger AK, Mrakotsky C, Hessler MJ, Brown KM, Hildebrand T: Preschool major depressive disorder: preliminary validation for developmentally modified DSM-IV criteria. J Am Acad Child Adolesc Psychiatry 2002; 41:928-937Crossref, Medline, Google Scholar
5. Robins E, Guze SB: Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry 1970; 126:983-987Link, Google Scholar
6. Luby JL, Heffelfinger AK, Mrakotsky C, Brown KM, Hessler MJ, Wallis JM, Spitznagel EL: The clinical picture of depression in preschool children. J Am Acad Child Adolesc Psychiatry 2003; 42:340-348Crossref, Medline, Google Scholar
7. Denham SA: Emotional Development in Young Children. New York, Guilford, 1998Google Scholar
8. Shaffer D, Fisher P, Lucas C (NIMH DISC Editorial Board): Diagnostic Interview Schedule for Children, Version IV. New York, Columbia University, Division of Psychiatry, 1998Google Scholar
9. Lucas C, Fisher P, Luby J: Young-Child DISC-IV Research Draft: Diagnostic Interview Schedule for Children. New York, Columbia University, Division of Child Psychiatry, Joy and William Ruane Center to Identify and Treat Mood Disorders, 1998Google Scholar
10. Maxwell E: The Family Interview for Genetic Studies Manual. Washington, DC, National Institute of Mental Health, Intramural Research Program, Clinical Neurogenetics Branch, 1992Google Scholar
11. Achenbach TM, Edelbrock C: Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, University of Vermont, Department of Psychiatry, 1995Google Scholar
12. Sparrow SS, Carter AS, Ciccheti DV: Vineland Screener: Overview, Reliability, Validity, Administration, and Scoring. New Haven, Conn, Yale University, Department of Psychology, 1987Google Scholar
13. Ablow JC, Measelle JR: The Berkeley Puppet Interview—Symptom Scales (BPI-SS). Berkeley, University of California, 1993Google Scholar
14. Ablow JC, Measelle JR, Kraemer HC, Harrington R, Luby J, Smider N, Dierker L, Clark V, Dubicka B, Heffelfinger A, Essex MJ, Kupfer DJ: The MacArthur Three-City Outcome Study: evaluating multi-informant measures of young children’s symptomatology. J Am Acad Child Adolesc Psychiatry 1999; 38:1580-1590Crossref, Medline, Google Scholar



