Patients Who Strive to Be Ill: Factitious Disorder With Physical Symptoms
Abstract
OBJECTIVE: Factitious disorder with physical symptoms characterizes patients who strive to appear medically ill and assume the sick role. Clinical suspicion is highest for female health care workers in the fourth decade of life. This study was designed to analyze the diagnosis of factitious disorder, the demographics of affected patients, and intervention and treatment. METHOD: Retrospective examination was of 93 patients diagnosed during 21 years. Two raters agreed on subject eligibility on the basis of DSM-IV criteria and absence of a somatoform disorder and a plausible medical explanation. RESULTS: The group included 67 women (72.0%); mean age was 30.7 years (SD=8.0) for women and 40.0 years (SD=13.3) for men. Mean age at onset was 25.0 years (SD=7.4). Health care training or jobs were more common for women (65.7%) than men (11.5%). Most often, inexplicable laboratory results established the diagnosis. Eighty had psychiatric consultations; 71 were confronted about their role in the illness. Only 16 acknowledged factitious behavior. Follow-up data were available for only 28 patients (30.1%); maximum duration of follow-up was 156 months. Two patients were known to have died. Few patients pursued psychiatric treatment. Eighteen left the hospital against medical advice. CONCLUSIONS: Factitious disorder affects men and women with different demographic profiles. Diagnosis must be based on careful examination of behavior, motivation, and medical history and not on a stereotype. Laboratory data and outside medical records help identify suspicious circumstances and inconsistencies. Confrontation does not appear to lead to patient acknowledgment and should not be considered necessary for management.
Factitious disorder with physical symptoms is challenging for health care providers. DSM-IV offers two inclusion criteria: physical symptoms are intentionally produced, and the patient’s motivation is to assume the patient role. The only exclusion criterion is the lack of external incentives seen in malingering. The DSM criteria define an extremely heterogeneous population with coexisting medical and psychiatric disorders.
Case series are an invaluable data source for factitious disorders, which can cause irreversible medical consequences for the patient, tremendous cost to society, and strong emotions in health care providers (1–4). The incidence and prevalence of factitious disorder with predominantly physical symptoms are unknown because its inherently secretive nature thwarts traditional epidemiological research. Sutherland and Rodin (5) estimated the incidence at a tertiary medical center of 0.8% on the basis of 10 patients (70% female) referred to psychiatry out of 1,288 psychiatric consultations. Population-based studies that use either surveys or review of comprehensive medical records have not been conducted.
Most literature regarding factitious disorders has been based on hundreds of case reports and a few large series. In 1983, Reich and Gottfried (4) described a 10-year experience with 41 patients with factitious disorders in a hospital population. This group was 95% female, their average age was 33 years, and 68% had health-related jobs. Carney and Brown (1) described 42 patients, 76% of whom were female. The mean age was 34 years, and 50% were in “caring professions.” The profile of the young female health care worker with factitious disorder is widely accepted (6).
Method
This study was approved by the Mayo Foundation’s institutional review board. Effective Jan. 1, 1997, Minnesota law requires patient consent for all medical records review for research. Consent is not required for patients seen before that date unless they return for subsequent care. Data were collected from February until June 1997; three potential patients were excluded.
Two databases were used to identify patients. The computerized master list of dismissal diagnoses from 1976 to 1996 was searched for “factitial disorder,” “factitial symptoms,” “Munchausen’s syndrome,” and “polysurgical syndrome.” However, this database was not sufficient because some patients with a compelling diagnosis of factitious disorder were not included. In some cases, the primary medical or surgical service elected not to state “factitious disorder” as the dismissal diagnosis but preferred a less provocative diagnosis, for example, “anemia of unknown origin.” To identify cases of this type, the psychiatric consultation service list from 1980 to 1996 was manually reviewed for all requests concerning these disorders. Because psychiatric consultations were not conducted on all patients, this resource was also insufficient. The two databases were used in a concerted effort to identify all patients with possible factitious disorder in the 20-year interval. The same inclusion and exclusion criteria were used for both sources of data. Missing records from the psychiatric consultation database determined the 4-year staggered start.
Data Collection
U.S. residents who were inpatients 18 years or older at index treatment were eligible. This study was designed to test the hypothesis that patients with factitious disorder have a shorter life expectancy than a national age- and sex-matched normative population. The aim was to collect follow-up data and use the Social Security Administration Death Master File to determine the age at death of the patients. Because of tremendous difficulty obtaining follow-up data, this part of the study was not completed. Problems included no permanent address, undocumented Social Security number, false names, and records that disappeared at dismissal.
All medical records were examined by two reviewers. DSM-IV criteria were used. Patients were included if their physical signs or symptoms were intentionally produced and their motivation was to assume the sick role. If external incentives such as economic gain were present, patients were excluded. Several additional issues not referred to in DSM-IV were also addressed. Patients were excluded if their medical records revealed one or more of the following: plausible medical explanation, possible somatoform disorder (suspected unconscious symptom production and motivation), exclusively psychological factitious symptoms, or inadequate data. Patients with symptoms limited to the hair and skin (apart from nonhealing deep wounds) were excluded because this set of patients was large; in this distinct subgroup, motivation to assume the sick role was generally absent. Both raters evaluated patients independently and then reached consensus. Patients were excluded if either reviewer determined a possibility that the symptoms were not factitious, usually because of a plausible medical disorder.
The index treatment was defined as the hospitalization during which the treatment team concluded that the patient’s illness was factitious. This index treatment became a reference point, and all subsequent data were considered follow-up or outcome data. Data were sought to support the classic diagnosis of Munchausen’s disorder, which requires a self-inflicted medical condition, visits to multiple medical centers (peregrination), and pathologic lying (pseudologia fantastica) (7). This step was undertaken because many physicians persist in using Munchausen’s terminology and criteria when referring to patients with factitious disorders. Peregrination was identified as having previously visited three or more medical centers for the same problem. The authors failed to develop a definition for pseudologia fantastica that could be operationalized.
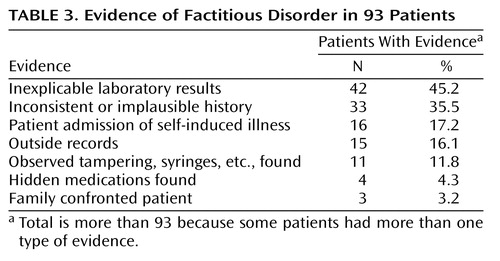
Patients were included only if there was conclusive evidence that the patient intentionally produced or feigned physical signs or symptoms (DSM-IV criterion A). The specific categories of evidence and examples are as follows:
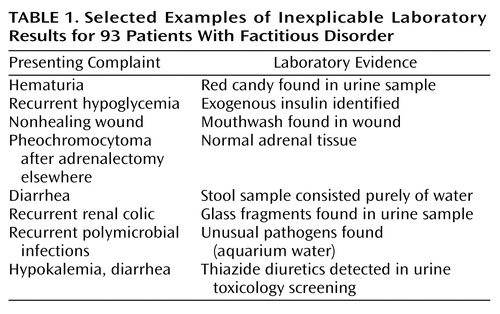
| 1. | Inexplicable laboratory results (foreign material in biopsy samples, positive results of toxicology screens, or a history of abnormal findings from biological fluids collected in private but normal findings from fluid collected while patient was under observation) (Table 1). | ||||
| 2. | Inconsistency between the history and results of physical examinations. | ||||
| 3. | Patient admission of self-induced illness. | ||||
| 4. | Records from other institutions (patients denying recent diagnostic evaluations in the context of contradictory information or criminal conviction for Munchausen’s syndrome by proxy). | ||||
| 5. | Observed tampering and inappropriate behavior (removal of dressings, manipulation of catheters, or syringes containing medications or contamination). | ||||
| 6. | Surreptitious use of medications (suspected medications were found in the patient’s possession). | ||||
| 7. | Family confrontation of patient. | ||||
Statistical Analysis
The data were entered into SAS 6.0 (SAS Institute, Cary, N.C.), and descriptive statistical analysis was conducted. Wilcoxon’s rank-sum test (also known as the Mann-Whitney U test) was used to test whether the median age was significantly different between male and female patients in the study. A two-sided test was used (8). The reported p value was based on the normal approximation; p values of 0.05 or less were considered statistically significant. The median, range, mean, and standard deviation were reported for age for each sex.
Results
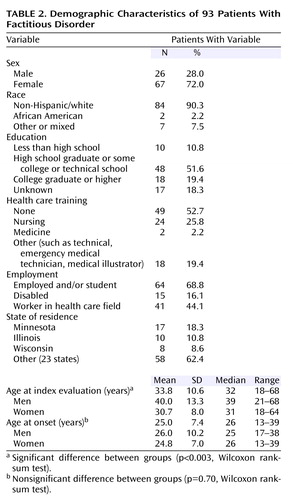
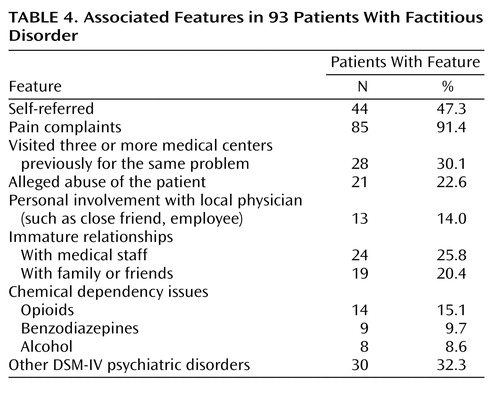
The study included 93 hospitalized patients with factitious disorder. Twenty cases were obtained from the institutional master list and 73 from the psychiatry consultation service list. The characteristics of the patients are described in Table 2. The study group was predominantly female, and the women were significantly younger than the men (p<0.003, Wilcoxon rank-sum test). Women were more likely to have health care training or jobs (N=44, 65.7%) than men (N=3, 11.5%). Peregrination was identified in 16 men (61.5%) and 28 women (41.8%). Table 3 lists the type of evidence that supported factitious disorder, and Table 4 provides several features associated with this study group. Complaints of pain were the most frequently associated feature, and problems with prescription medications were common. A subgroup had close relationships with local physicians. Several patients exhibited unusually immature behavior with hospital staff or family and friends, a finding suggesting poor coping skills.
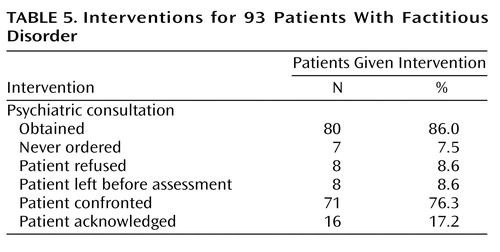
The interventions pursued by primary medical or surgical services are listed in Table 5. The majority of the patients (76.3%) were confronted with their diagnosis; however, only a small number (17.2%) acknowledged that their illness was self-induced or simulated.
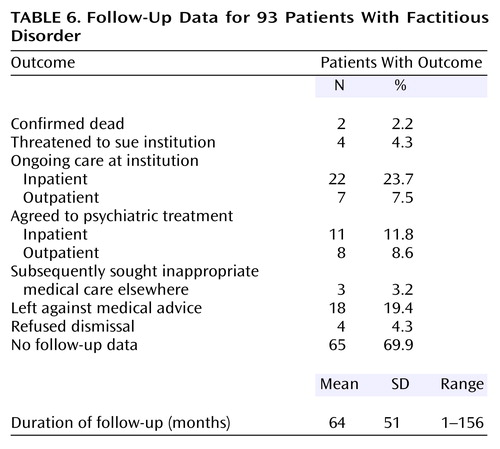
Follow-up data are included in Table 6. A small number of patients received continuing medical care at the same institution after the diagnosis of factitious disorder was established. The medical records revealed three patients who subsequently sought inappropriate medical care elsewhere. In some cases, this outcome was determined because other institutions requested medical records. Eighteen patients left against medical advice, and four patients refused dismissal. A small group of patients agreed to receive psychiatric treatment, but it was difficult to determine to what extent they engaged in treatment and modified their behavior.
Discussion
Determining what evidence is sufficient for establishing the diagnosis of factitious disorder remains difficult. Five levels of factitious disorder behavior have been proposed: 1) fictitious history, 2) simulation, 3) exaggeration, 4) aggravation, and 5) self-induction of disease (6). These levels are awkward to apply because they overlap, and patient presentation varies over time. Most of the patients included in this study group would be placed in level 4 or higher because conclusive laboratory data and physical examination data are more readily available. At lower levels of enactment, physicians must rely on inconsistent medical histories. Medical records from elsewhere offering contradictory information are useful, but secretive patients are often reluctant to authorize their release. Insightful family members, if available, also may provide invaluable data regarding a fictitious history or simulation of symptoms.
Differential diagnosis in patients with self-destructive behaviors is extensive, and the disorders include somatoform, eating, chemical dependency, personality, psychotic, and malingering. Verifying that a patient’s objective is to assume the sick role rather than, for example, to access drugs, is critically important. Evidence that was acceptable for this retrospective study was deliberately conservative. Additional patients may have presented with suspicious behaviors that were never documented as potentially factitious by the hospital teams. As a result, these patients are likely an underrepresentation of the number of patients with factitious disorder seen at our institution.
The two databases used for this study yielded similar cases existing in different contexts. The computerized master list primarily included patients with clear-cut situations. This source provided data regarding the 23 patients who were not seen by the psychiatry consultation team; reasons for this were patient refusal, patient dismissal, or lack of a request. Fewer data concerning past psychiatric history and social concerns were available for these patients. Primary services were hesitant to record factitious disorder as the dismissal diagnosis, sometimes with even robust evidence. The psychiatric consultation log revealed 121 patients with a questionable factitious disorder. In 48 instances, patients were excluded from the final study group because of insufficient evidence or exclusion criteria, but in 73 cases, the factors supporting the DSM-IV diagnosis were present in the opinion of the examining psychiatrist. However, sometimes the primary surgical or medical team still declined to explicitly state factitious disorder on the dismissal summary. The willingness for psychiatrists and nonpsychiatrists to document factitious disorder varies considerably within this institution and nationally. Even published case reports can generate controversy to consider factitious disorder in the presence of other psychiatric diagnoses (9).
In our experience, physicians are reluctant to consider a factitious process in the differential diagnosis unless definitive proof is available. If the threshold of evidence is too high, patients undergo unnecessary, risky, and expensive procedures. However, when the standard for evidence is too low, patients can be inappropriately confronted about their role in inducing an illness. In our opinion, factitious disorders must remain diagnoses with exclusion and inclusion criteria. Simply identifying core inclusion symptoms does not address the extensive psychiatric and medical differential diagnosis (10). New diagnostic results, such as low C-peptide levels in suspected exogenous insulin use, can simplify documenting a factitious process (11, 12). However, more in-depth understanding of the vast array of medical disorders and their variants can make it more difficult to confidently consider a factitious explanation.
The need for diagnostic rigor is clear. Once a treatment team becomes suspicious that a patient is deliberately fabricating or simulating an illness, countertransference issues potentially interfere with the provision of compassionate medical care. Furthermore, if the treatment team decides to confront a patient about a suspected factitious disorder, the patient-physician relationship is likely to be irrevocably damaged.
The high percentage (72.0%) of female patients in this study group challenges the DSM-IV assertion that factitious disorder is more common in men. Additional reports describing relatively large study groups would assist in determining the sex prevalence. Clearly, published single case studies may be misleading in this regard.
Our study confirms that a significant subgroup (47.3% of the total) consisted of female health care workers. The well-known stereotype of the patient with factitious disorder has likely biased this retrospective study group. Nonetheless, the study method also permitted identification of a small majority of patients (52.7%) who had a different demographic background. The vague inclusion criteria used previously may have unfairly weighed demographic factors in studies in which the patients were overwhelming female (5). The use of two reviewers to determine potential cases was expected to reduce the ascertainment bias inherent in a project of this type. The relative number of health care workers in case series of factitious disorder is striking (1, 4, 5). These patients have the knowledge and skills needed to induce a plausible illness. Whether this pattern diminishes over time with the evolution of television programs depicting realistic and graphic medical scenes remains to be seen. Close relationships with local physicians, which included family members, employees, and friends, were observed, and the illness conceivably facilitated more contact or the relationship interfered with detection of the factitious process.
Most of the patients (71.3%) were well educated (high school education or higher), and most (68.8%) were either employed or full-time students. This socioeconomic distribution is unlikely to be explained by persons having insurance coverage that permitted access to a tertiary medical center. During this study, unemployed and disabled patients would have had ready access because of government insurance programs. Patients with factitious disorders have been described as belonging to higher socioeconomic groups, but this characterization has not been a satisfactory explanation (13). The age at onset was in early adulthood for both men and women.
Evidence indicating the most effective intervention and treatment is still lacking. Immediate confrontation appears ineffective in most patients. The approach advocated by Eisendrath and associates (10) is likely preferable, in which patients suspected of having a factitious process are treated in a supportive manner without confrontation. Physicians often feel that confrontation is necessary to complete the evaluation; however, data show that few patients admit their behavior. The alternative method is gradually to develop an empathetic relationship that induces the patient to give up the maladaptive behaviors. The assistance of a psychiatrist is beneficial to assess the patient for coexisting psychiatric disorders and to advise the primary health service on management (14). However, when patients place themselves at risk of iatrogenic injury, a more direct approach is sometimes mandatory. Treatment of any coexisting chemical dependency or psychiatric disorder is optimal.
The generalizability of these observations made at a midwestern tertiary care center is unclear. Psychiatrists and nonpsychiatrists at medical centers renowned for specialized diagnostic evaluations likely encounter similar patients. This study group clearly represents a referral group because patients traveled from all over the United States for medical care. However, for many patients, the desire to obtain multiple medical opinions appears to be an element of the disorder. The impact of managed care restrictions on reducing peregrination is unclear. In our opinion, no psychiatric or medical disorder served meaningfully as a control group. In this respect, this study departs from conventional research standards. If future prospective studies are feasible for examining long-term outcome, quality of life, or health care costs, for example, some type of comparison group will be necessary.
The investigators are aware that some of the information in the medical records of this group of patients may be inaccurate. For example, the information regarding visits to previous health care centers could not be easily verified. Patients are likely to have underestimated the number of visits if they were concerned that doing otherwise would expose them to scrutiny for a factitious disorder. Several patients had social and developmental histories that were clearly implausible, but no means were available to verify their educational or occupational histories. The diagnosis of Munchausen’s syndrome requires the presence of a self-induced illness, visits to multiple medical centers, and pseudologia fantastica (7). This terminology did not prove to be useful with this study group because of the inherent difficulty in operationalizing these criteria. Because of this hurdle, we recommend that physicians use the DSM terminology of factitious disorder rather than this outdated classification system.
Medical records from other institutions were essential for establishing the diagnosis of factitious disorder for 15 patients. Outside records permitted the treatment team to be aware of the suspicions and working diagnoses of previous health care providers. They also informed the team of which diagnostic tests had been performed previously, and this information helped the team understand the patients’ relentless quest for further evaluations, which might include exploratory operations. Outside records will be increasingly difficult to access because of new federal privacy regulations. The effects of new federal privacy regulations that allow patients to request alterations to their medical records if they detect a mistake remain to be seen. Privacy legislation may encourage some patients to obtain much-needed health care. In the case of a patient with a factitious disorder, the regulations may make establishing a diagnosis addressing self-destructive behavior even more difficult.
This study was conducted in compliance with Minnesota state law regulating researchers’ access to medical records (15). Legislation is likely to interfere substantially with research on secretive disorders. Patients are unlikely to provide consent for research authorization. Compounding a patient’s inherent propensity to falsify information, this legislation may make it increasingly difficult for health care providers to understand the risk factors, appropriate interventions, and outcomes of patients with factitious disorders.
 |
 |
 |
 |
 |
 |
Received Dec. 6, 2001; revisions received May 21 and Dec. 4, 2002; accepted Jan. 22, 2003. From the Department of Psychiatry and Psychology and the Section of Biostatistics, Mayo Clinic. Address reprint requests to Dr. Krahn, Mayo Clinic, 200 First Street SW, Rochester, MN 55905; [email protected] (e-mail). The authors thank Reena Grewal, M.D., and Ann M. Harris, who assisted in data collection, and the biostatisticians at the Mayo Clinic Center for Patient-Oriented Research.
1. Carney MW, Brown JP: Clinical features and motives among 42 artifactual illness patients. Br J Med Psychol 1983; 56:57-66Crossref, Medline, Google Scholar
2. Feldman MD: The costs of factitious disorders (letter). Psychosomatics 1983; 35:506-507Crossref, Google Scholar
3. Feldman MD, Hamilton JC, Deemer HN: Factitious disorder, in Somatoform and Factitious Disorders. Edited by Phillips KA. Washington, DC, American Psychiatric Publishing, 2001, pp 129-166Google Scholar
4. Reich P, Gottfried LA: Factitious disorders in a teaching hospital. Ann Intern Med 1983; 99:240-247Crossref, Medline, Google Scholar
5. Sutherland AJ, Rodin GM: Factitious disorders in a general hospital setting: clinical features and a review of the literature. Psychosomatics 1990; 31:392-399Crossref, Medline, Google Scholar
6. Folks GD, Feldman MD, Ford CV: Somatoform disorders, factitious disorders, and malingering, in Psychiatric Care of the Medical Patient, 2nd ed. Edited by Stoudemire A, Fogel BS, Greenberg DB. Oxford, UK, Oxford University Press, 2000, pp 459-475Google Scholar
7. Asher R: Munchausen’s syndrome. Lancet 1951; 1:339-341Crossref, Medline, Google Scholar
8. Van der Vaart HR: On the robustness of Wilcoxon’s two-sample test, in Quantitative Methods in Pharmacology. Edited by de Jonge. Amsterdam, North-Holland, 1961, pp 140-158Google Scholar
9. Krahn LE: Paranoid schizophrenia—malingering or factitious disorder? (letter). Am J Psychiatry 1999; 156:498Medline, Google Scholar
10. Eisendrath SJ, Rand DC, Feldman MD: Factitious disorders and litigation, in The Spectrum of Factitious Disorders. Edited by Feldman MD, Eisendrath SJ. Washington, DC, American Psychiatric Publishing, 1996, pp 65-81Google Scholar
11. Lebowitz MR, Blumenthal SA: The molar ratio of insulin to C-peptide: an aid to the diagnosis of hypoglycemia due to surreptitious (or inadvertent) insulin administration. Arch Intern Med 1993; 153:650-655Crossref, Medline, Google Scholar
12. Wallach J: Laboratory diagnosis of factitious disorders. Arch Intern Med 1994; 154:1690-1696Crossref, Medline, Google Scholar
13. Kasdan ML, Soergel TM, Johnson AL, Lewis K, White WL: Expanded profile of the SHAFT syndrome. J Hand Surg [Am] 1998; 23:26-31Crossref, Medline, Google Scholar
14. Feldman MD, Feldman JM: Tangled in the web: countertransference in the therapy of factitious disorders. Int J Psychiatry Med 1995; 25:389-399Crossref, Medline, Google Scholar
15. Yawn BP, Yawn RA, Geier GR, Xia Z, Jacobsen SJ: The impact of requiring patient authorization for use of data in medical records research. J Fam Pract 1998; 47:361-365Medline, Google Scholar



