Neurobehavioral Disinhibition in Childhood Predicts Early Age at Onset of Substance Use Disorder
Abstract
OBJECTIVE: This longitudinal study had three aims: 1) determine the extent to which boys at high average risk and low average risk for substance use disorder differ on a construct of neurobehavioral disinhibition, 2) evaluate the capacity of neurobehavioral disinhibition to predict substance use frequency at age 16, and 3) demonstrate the utility of neurobehavioral disinhibition in predicting substance use disorder. METHOD: The authors derived an index of neurobehavioral disinhibition from measures of affect, behavior, and cognition. The neurobehavioral disinhibition score was used to discriminate youth at high and low average risk for substance use disorder and to predict substance use frequency after 4–6 years and substance use disorder after 7–9 years. RESULTS: The neurobehavioral disorder score significantly discriminated boys at high average risk from those at low average risk at ages 10–12. Neurobehavioral disinhibition at age 16, in conjunction with substance use frequency and risk status group, predicted substance use disorder at age 19 with 85% accuracy and accounted for 50% of the variance in Drug Use Screening Inventory overall problem density score. Neurobehavioral disinhibition was a stronger predictor of substance use disorder (odds ratio=6.83) than substance consumption frequency (odds ratio=3.19). CONCLUSIONS: Cross-sectional and longitudinal analyses indicated that neurobehavioral disinhibition is a component of the liability to early age at onset of substance use disorder.
Variation in the risk for and severity of substance use disorder is the product of the interaction of numerous biobehavioral traits and environmental variables. Accordingly, the multifactorial model of liability to complex (polygenic) disorders (1) is a standard framework for research directed at elucidating the etiology of substance use disorders (2). From accumulating evidence demonstrating that substance use disorder is a developmental outcome (3), the multifactorial model has been recently adapted to etiological investigations having an ontogenetic framework (4).
Deficient capacity to control behavior and regulate emotion commensurate with situational demands has been documented in many studies to be associated with the liability for early age at onset of substance use disorder (see references 3 and 5 for reviews). Youth at high risk for substance use disorder commonly exhibit impulsivity, reactive aggression, sensation seeking, and excessive risk taking (3, 6). Irritability, negative affect, and a difficult temperament makeup have also been frequently documented in youth at high risk for substance use disorder (7–9). In addition, compared with the general population, high-risk youth more frequently qualify for conduct disorder, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, and depressive disorder (10–12). It is not uncommon for internalizing and externalizing disorders to occur conjointly, suggesting that a core feature comprising the liability for substance use disorder is behavioral and affective dysregulation. Notably, a review of the literature concluded that the scope of disturbances reflecting deficient self-regulation in youth at high risk for substance use disorder is consistent with the pattern of disturbances concomitant to a prefrontal cortex dysfunction (3). Significantly, two childhood psychiatric disorders associated with increased risk for substance use disorder, namely conduct disorder and ADHD, have been implicated as reflecting a prefrontal cortex disturbance (13, 14).
Evidence has also been accrued that directly points to an association between prefrontal cortex dysfunction and increased risk for substance use disorder. Neuropsychological tests sensitive to detecting prefrontal cortex disturbance have revealed impairments in high-risk youth (15–17). Furthermore, severity of neurocognitive impairment pertaining to executive cognitive functions correlates significantly with drug use frequency and drug use problems in adolescents (18).
Amplitude attenuation of the P300 component of the event-related potential has been found to be most prominent over the frontal convexity (19). Low P300 amplitude points to low physiological inhibition (20). In addition, the attenuated P300 amplitude observed in youth at high risk for substance use disorder reflects a maturational lag (21). It is also noteworthy that the capacity to execute an antisaccade eye movement, a marker of prefrontal cortex functioning, is impaired in high-risk individuals (22, 23).
Considered in aggregate, the available evidence points to a prefrontal cortex disturbance underlying, at least in part, the liability for substance use disorder. Collectively, the manifest disturbances encompass impaired executive cognitive capacity, dysregulated emotion, and behavior undercontrol. This profile, termed “disinhibitory psychopathology” (24), has been shown to be strongly influenced by genetic factors (25). The extent to which disinhibitory psychopathology in childhood predicts substance use disorder has, however, not been determined.
This study had three objectives. First, we sought to determine whether neurobehavioral disinhibition, indexed by indicators of executive cognitive functioning, emotion regulation, and behavior control, distinguishes 10–12-year-old boys at high and low average risk for substance use disorder. Second, we evaluated the extent to which neurobehavioral disinhibition predicted substance use behavior in mid-adolescence (age 16). Last, we examined whether substance use disorder outcome at age 19 could be predicted by neurobehavioral disinhibition. It was hypothesized that neurobehavioral disinhibition would discriminate youth at high and low average risk for substance use disorder and would predict this outcome in early adulthood.
Method
Subjects
For this report, the study group consisted of 10–12-year-old biological male offspring of probands who either satisfied DSM-III-R criteria for lifetime substance use disorder (N=47) or had no lifetime substance use disorder or other axis I or axis II disorder in adulthood (N=65). These two offspring groups were respectively designated as being at high average risk and low average risk on the basis of the frequent observation that the former subjects have a four- to sevenfold greater risk to develop substance use disorder (4). The probands had been recruited by using multiple methods from diverse sources to minimize sampling bias that could occur if recruitment was conducted from only one source. Seventy-seven percent of the substance use disorder men were recruited through advertisement. The remainder were accrued by a market research firm that used random-digit dialing or were from the pool of graduates of a substance abuse treatment program. This group, which consisted of treatment and nontreatment probands and used a combination of self-referred and investigator-initiated recruitment methods, increases the likelihood that the full spectrum of substance use disorder severity was represented. The psychiatrically normal probands were recruited by using the same procedures except that none was derived from treatment facilities. Although the sampling strategy was not random because of the specific recruitment criteria that needed to be satisfied by the family, comparison of the probands in this study and their offspring with subjects in epidemiological studies indicates similarity (26).
Only one child in each family—the oldest boy in the 10–12-year age range—was enrolled in this study. All of the boys underwent a physical examination conducted by a nurse. The presence of physical anomalies associated with intrauterine chronic alcohol exposure as well as maternal drug dependence during gestation disqualified the child from study. In addition, psychosis, neurological injury, and severe physical or developmental disability were exclusionary criteria.
Procedure
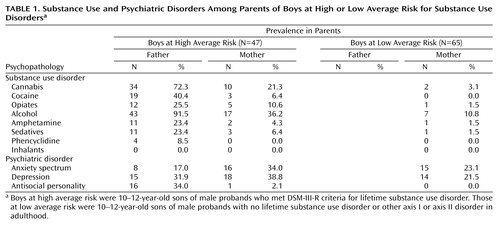
Prior to implementing the research protocols, written assent and informed consent were respectively obtained from the children and their parents. In addition, subjects were informed that privacy of the findings from this research was protected by a Certificate of Confidentiality issued to the Center for Education and Drug Abuse Research by the National Institute on Drug Abuse. The research protocol described here is part of a comprehensive investigation aimed at elucidating the genetic, biochemical, physiological, psychological, and environmental components of the liability for substance use disorder. Total time required for the baseline evaluation was approximately 26 hours spread across 2 days. The follow-up evaluations at ages 16 and 19 required approximately 10 hours and 4 hours, respectively, and were completed in one day. Upon completion of the baseline assessment, the child was paid $100 in the form of a gift certificate. At ages 16 and 19, the compensation was $150 and $100. The biological parents were assessed at the same time as the child’s baseline evaluation to characterize their psychiatric history (Table 1). They were each paid $100 for participation. Teachers served as informants of the classroom behavior of the boys and were compensated $10 for completing the rating scale.
Diagnostic Formulation
The diagnostic evaluation of the probands—and their sons when they attained age 19—was conducted with an expanded version of the Structured Clinical Interview for DSM-III-R (SCID) (27). The SCID was modified to characterize antisocial and substance use behavior in extensive detail. Diagnoses were consensually formulated by a committee consisting of a board-certified psychiatrist (chair), another psychiatrist or clinical psychologist, and the research associate who conducted the interview. The best-estimate procedure for diagnosis (28) was utilized: the results of the structured interview were considered in conjunction with all available medical, legal, psychiatric, and social history information. The diagnostic interviews of the children at ages 10–12 and 16 were conducted with the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic Version (K-SADS-E) (29). Information regarding the temporal patterning of psychiatric status and drug use behavior was also obtained (30). At the age 19 follow-up evaluation, 19.6% of the study group (N=22) qualified for a diagnosis of substance use disorder consequent to consumption of any compound with the exception of nicotine. Nicotine dependence was not considered an outcome because this condition is not ordinarily related to social maladjustment. For more details regarding the study group, the reader is referred to Clark et al. (30–32).
Neurobehavioral Disinhibition
The neurobehavioral disinhibition construct was derived by using item response theory methods applied to indicators of affect, behavior, and cognition. The affect dimension was assessed with the Revised Dimensions of Temperament Survey (33). On the basis of a previous finding that the estimate of the latent trait score of the difficult temperament index correlates very highly with the total number of positive responses (34), we recorded the sum of endorsed responses. The behavior dimension was assessed by tabulating the number of conduct disorder, oppositional defiant disorder, and ADHD externalizing symptoms reported by the mother on the K-SADS-E (29) and the total score on the Disruptive Behavior Disorders Rating Scale (35) reported by the teacher. Internal reliability of this scale was very high (alpha=0.95). Inasmuch as the child is in elementary school at the time of baseline evaluation, he has primarily one teacher. Thus, there is a high level of familiarity with the child’s classroom behavior. The cognitive dimension of neurobehavioral disinhibition was evaluated by using a battery of tests measuring executive cognitive functions (15). These higher-order cognitive functions exercise a supervisory or control influence on emotional regulation and behavioral control. The specific tests administered by trained master’s-level clinical associates were the Stroop, Porteus Mazes, vigilance, motor restraint, forbidden toys, and Block Design test of the WISC-III-R. The scores on these tests have been previously shown to constitute a single first-order factor (15).
Outcome Variables
The dependent variable at age 16 was substance use frequency. This variable measured the combined frequency of use of alcohol, tobacco, marijuana, and other drugs consumed in the prior 30 days. This information was obtained from section 1 of the revised Drug Use Screening Inventory (36).
At age 19, two dependent variables were analyzed. First, categorical substance use disorder diagnosis (present/absent) was investigated. The diagnosis of substance use disorder was based on DSM-III-R criteria because this project was implemented prior to the advent of DSM-IV. Second, the 149-item self-report Drug Use Screening Inventory (36) measured severity of disturbance at age 19 beyond the categorical diagnosis. The Drug Use Screening Inventory evaluates, using a range of 0%–100%, the severity of problems on 10 scales: 1) substance abuse, 2) psychiatric disturbance, 3) health problems, 4) behavior disorder, 5) school maladjustment, 6) work problems, 7) social skill deficits, 8) peer relationship problems, 9) family disruption, and 10) recreation/leisure problems. In addition to scores on the primary scales, an overall problem density score summarizes severity across all domains. Psychometric studies have demonstrated that this inventory is a reliable and valid self-report assessment (37, 38).
Statistical Analysis
Comparison between the high average risk and low average risk boys on the neurobehavioral disinhibition trait measured at baseline and mid-adolescence was conducted by using a t test. Multiple linear regression was employed to test the relationship between the score on the latent trait of neurobehavioral disinhibition at age 10–12 and substance use behavior at age 16. Last, logistic and linear hierarchical regression analyses were conducted to determine the extent to which neurobehavioral disinhibition singly and in combination with substance use at age 16 predicted transition to substance use disorder and Drug Use Screening Inventory overall problem density score at age 19. In both types of regression analyses, IQ and socioeconomic status were entered first followed by neurobehavioral disinhibition and substance use frequency scores. In the logistic regression analysis, the neurobehavioral disinhibition and substance use frequency scores were standardized to enable direct comparison of odds ratios.
Results
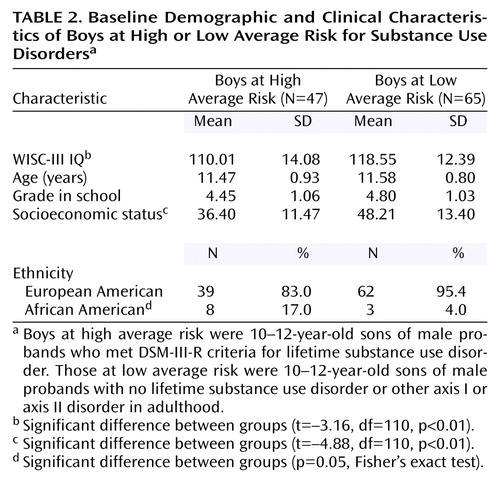
Table 2 summarizes the characteristics of the boys at high average risk and low average risk at the time of baseline assessment. The average IQ score was significantly lower in the boys at high average risk, although their performance was in the normal range. Age and education were comparable in the two groups. As expected, significantly lower socioeconomic status (39) was seen in the high average risk group than the low average risk group. Compared with the boys at low average risk, a lower proportion of the high average risk group was of European American background, and a higher proportion was of African American background.
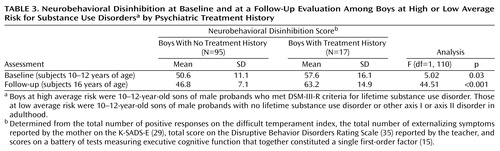
Following baseline study at age 10–12, the high average risk and low average risk groups were reevaluated in two follow-up assessments conducted at ages 16 and 19. By age 19, 15.2% of the subjects had received treatment for a psychiatric or substance abuse problem. As shown in Table 3, the score for the latent trait of neurobehavioral disinhibition was significantly higher at baseline and the age 16 follow-up evaluation in the boys who had received treatment. Because the number of boys who had received psychiatric treatment was small (N=17), it was not possible to determine whether this factor had an impact on the risk for substance use disorder.
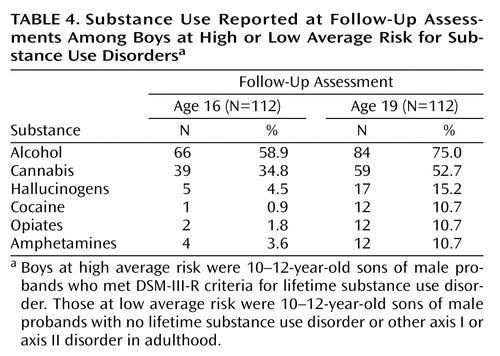
Table 4 summarizes the lifetime rate of use of a variety of compounds associated with abuse or dependence liability. These rates should not be construed to represent the prevalence rate in the population inasmuch as the study group was not randomly accrued but rather ascertained on the basis of presence/absence of substance use disorder consequent to illicit drug use in the proband fathers.
Neurobehavioral Disinhibition Factor Analyses
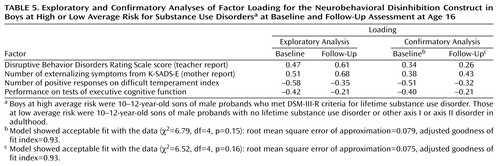
Unidimensionality of the neurobehavioral disinhibition scale was first checked by using exploratory factor analysis at ages 10–12 and 16. A covariance matrix was used to conduct a principal-component factor analysis. The number of factors retained was decided by plotting the eigenvalue derived from the factor analysis against the component rank (scree plot). In each factor analysis, the scree plot strongly suggested a one-factor solution. The first eigenvalue was 1.56 at age 10–12 and 1.57 at age 16. The first factor explained 29% of variance at ages 10–12 and 16. A single factor that explains over 20% of the variance is consensually accepted to reflect a dominant factor (40). The results of these analyses thus support the unidimensionality of the neurobehavioral disinhibition construct at ages 10–12 and 16. The factor loadings are presented in Table 5.
Next, unidimensionality of the variance-covariance matrix of variables that constitute neurobehavioral disinhibition was tested by using confirmatory factor analysis. First, the fit of one-factor model was tested for each assessment (ages 10–12 and 16). Error variances were set to be equal, and a correlation was allowed between the error terms of disruptive behavior and externalizing symptoms in the model because they measure the same trait (41). Table 5 summarizes the results of this maximum likelihood method analysis, which showed acceptable data-model fit at each assessment.
Next, a two-factor model was tested: disruptive behavior and executive cognitive function were indicators of the first factor, and externalizing behavior symptoms and difficult temperament index were indicators of the second factor. Because no significant improvement was observed from the one-factor model to the two-factor model at either the baseline assessment (χ2=5.99, df=3, p=0.11, adjusted goodness of fit index=0.91; change in χ2=0.80, df=1, p=0.37) or age 16 follow-up evaluation (χ2=6.48, df=3, p=0.09, adjusted goodness of fit index=0.91; change in χ2=0.04, df=1, p=0.84), the one-factor model was preferred.
In a follow-up analysis, we tested for invariance of the factor structure between assessments. We first replaced the factor loadings obtained from the model tested at age 10–12 with the factor loadings of the model tested at age 16. Results of this analysis indicated an acceptable fit between the data and the model (χ2=9.45, df=7, p=0.22; adjusted goodness of fit index=0.97).
We also tested a more restrictive model by replacing factor loadings and error terms obtained in the baseline model (age 10–12) with the factor loadings and error terms in the follow-up model tested at age 16. This model had poorer fit compared with the previous model: χ2=18.10, df=9, p<0.04; adjusted goodness of fit index=0.92. These two models were statistically different (change in χ2=8.15, df=2, p=0.002). Thus, the results indicate invariance of factor loadings of the model at ages 10–12 to 16. The differences between baseline and follow-up were due only to the error terms.
The stability of the neurobehavioral disinhibition latent variable from ages 10–12 to 16 is also indicated by the significant intraclass correlation coefficient between the respective indices (r=0.45, 95% CI=0.29–0.58; p<0.001).
Discriminant and Predictive Power of Neurobehavioral Disinhibition
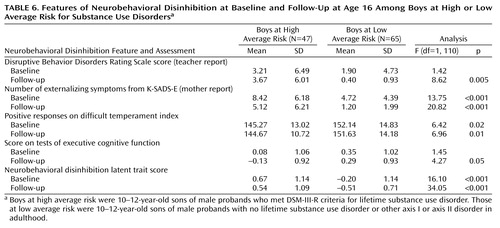
Table 6 presents the results of the group comparison on the features and latent trait of neurobehavioral disinhibition. At baseline and age 16, the high average risk and low average risk youth were significantly different on two of the four variables. At age 16, all four variables discriminated the two groups. Also, as shown in Table 6, the high average risk and low average risk boys differed significantly at baseline and at age 16 on the neurobehavioral disinhibition latent trait.
Next, the score for the latent trait of neurobehavioral disinhibition at age 10–12 was used to predict frequency of substance use at age 16. The proportion of drug consumption variance at age 16 accounted for by neurobehavioral disinhibition alone at age 10–12 was not significant (R2=0.01; F=0.52, df=1, 110, p=0.47). The neurobehavioral disinhibition construct was, however, a significant predictor of substance use disorder outcome 7–9 years later (odds ratio=1.51, 95% CI=1.01–2.74; Wald χ2=3.97, df=1, p=0.04). Sensitivity was 64%, specificity was 63%, positive predictive power was 64%, and negative predictive power was 63%. Overall classification accuracy was 63%. The odds ratios for risk status group, IQ, and socioeconomic status were not significant.
As expected, because of the shorter duration between assessment and outcome, prediction was more accurate between ages 16 and 19. Logistic regression analysis indicated that substance use disorder outcome at age 19 was predicted by neurobehavioral disinhibition (odds ratio=6.83, 95% CI=2.33–20.01; Wald χ2=12.26, df=1, p<0.001) and substance use frequency at age 16 (odds ratio=3.19, 95% CI=1.69–6.04; Wald χ2=12.75, df=1, p<0.001). The odds ratios for risk status (i.e., son of substance use disorder or healthy comparison father), IQ, and socioeconomic status were not significant. Overall, the predictive classification accuracy of neurobehavioral disinhibition and substance use combined was 85%. Sensitivity was 91%, specificity was 83%, positive predictive power was 97%, and negative predictive power was 61%.
In addition to the categorical outcome of substance use disorder, it was observed that neurobehavioral disinhibition (beta=0.44; t=4.64, df=106, p<0.001) and substance use frequency at age 16 (beta=0.32; t=3.96, df=106, p<0.001) explained 50% of the variance in Drug Use Screening Inventory overall problem density score at age 19 (F=18.45, df=5, 106, p<0.001). High-risk status, IQ, and socioeconomic status were not significant predictors.
Discussion
The findings of this study indicate that neurobehavioral disinhibition discriminates preadolescent boys who are at high and low average risk for a substance use disorder. The score on this trait at age 10–12 did not predict level of substance use behavior in mid-adolescence (age 16) but did predict transition to substance use disorder at age 19. This finding suggests that neurobehavioral disinhibition may not portend substance use but rather is an indicator of liability to develop substance use disorder. Notably, the odds ratio for substance use disorder prediction was larger for the neurobehavioral disinhibition trait at age 16 than the odds ratio for substance use frequency. These results contribute to mounting evidence indicating that neurobehavioral disinhibition is a component of the liability to early age at onset of substance use disorder (42–44).
This research was guided by the hypothesis that measures of labile affect (difficult temperament), externalizing behavior (oppositional defiant disorder, conduct disorder, and ADHD symptoms), and executive cognitive function are indicators of a common underlying process. Results of both the exploratory and the confirmatory factor analyses supported this hypothesis. Importantly, the indicators encompass the three main domains of psychological functioning, namely cognition, affect, and behavior. As noted in Table 5, the neurobehavioral construct is not merely synonymous with quantification of disruptive behavior that has been shown frequently to presage substance use disorder.
The results reported herein have heuristic ramifications for elucidating the etiology of substance use disorder. In particular, the findings point to the utility of using a continuous trait indexing severity beyond dichotomous diagnosis for identifying youth who are at high risk for substance use disorder. In this regard, the neurobehavioral disinhibition trait, encompassing the facets of both externalizing and internalizing disorders, parsimoniously reduces the manifest features into an index reflecting their shared variance. As noted previously, the indicators of this trait reflect the integrity of prefrontal cortex functioning.
What is the relation between the latent trait of neurobehavioral disinhibition and substance use disorder? Inasmuch as neurobehavioral disinhibition appears to be a component of the liability for substance use disorder, it is reasonable to conclude that increasing severity on this trait covaries with the probability of succumbing to a disorder. The particular psychiatric presentation reflects the differential salience of the manifest affect and behavior disturbances resulting in internalizing and externalizing diagnoses which, not uncommonly, are comorbid within the individual.
One issue raised by the findings reported herein concerns whether the neurobehavioral disinhibition construct has superior predictive utility compared with only externalizing disorder. To address this issue, the analyses predicting substance use disorder outcome were also computed by using number of externalizing symptoms (ADHD, conduct disorder, oppositional defiant disorder). The resulting odds ratio for externalizing symptoms was 4.74; this is about 30% lower than the odds ratio of 6.83 for neurobehavioral disinhibition. It can thus be concluded that the neurobehavioral disinhibition construct is a somewhat stronger predictor of substance use disorder than externalizing disturbance alone.
Several limitations of this study are noteworthy. First, the study group was confined to male subjects; thus, it is not known whether the predictive accuracy extends to early age at onset of substance use disorder in female subjects. Notably, Caspi et al. (45) observed that 3-year-old boys described as irritable, impulsive, and distractible were approximately three times more likely than a comparison group of boys to qualify for an alcohol dependence disorder at age 21. However, no association between these characteristics and substance use disorder was observed in girls. It may be that there is gender specificity with respect to the contribution of neurobehavioral disinhibition on the risk for substance use disorder or that different mediating and moderating factors influence this association. Second, the study group size (N=112) at age 19 was small in relation to the size of patient groups typically employed in epidemiological investigations. Clearly, cross-validation with a larger sample is required before the measures described herein can be routinely utilized in clinical settings. And third, whereas this study supports the predictive utility of the neurobehavioral disinhibition construct, it is essential to emphasize that substance use disorder risk is determined by the quality of manifold complex phenotype-environment interactions (3). For example, a recent study by Wong et al. (46) found that children with poor behavioral self-control evoked more negative reactions from parents which, in turn, resulted in externalizing behavior. This latter study highlights the need for future research to emphasize the quality of person-environment interactions biasing the developmental trajectory toward or away from a substance use disorder outcome. These limitations notwithstanding, the present results illustrate the need to develop prevention interventions that specifically target the factors contributing to the risk for substance use disorder.
 |
 |
 |
 |
 |
 |
Received June 13, 2002; revision received Dec. 11, 2002; accepted Dec. 27, 2002. From the University of Pittsburgh Department of Pharmaceutical Sciences, Department of Psychiatry, and Department of Medicine, Pittsburgh. Address reprint requests to Dr. Tarter, School of Pharmacy, University of Pittsburgh, 711 Salk Hall, Pittsburgh, PA 15261; [email protected] (e-mail). Supported by grants from the National Institute on Drug Abuse (DA-05605 and DA-00237), the National Institute on Alcohol Abuse and Alcoholism (AA-00291 and AA-11637), and the National Institute of Dental and Craniofacial Research (DF-13844).
1. Falconer D: The inheritance of liability to certain diseases estimated from the incidence among relatives. Ann Hum Genet 1965; 29:51-76Crossref, Google Scholar
2. Reich T, Cloninger C, Guze S: The multifactorial model of disease transmission, 1: description of the model and its use in psychiatry. Br J Psychiatry 1975; 127:1-10Crossref, Medline, Google Scholar
3. Tarter R, Vanyukov M, Giancola P, Dawes M, Blackson T, Mezzich A, Clark D: Etiology of early age onset substance use disorder: a maturational perspective. Dev Psychopathol 1999; 11:657-683Crossref, Medline, Google Scholar
4. Vanyukov M, Tarter R: Genetic studies of substance abuse. Drug Alcohol Depend 2000; 59:101-123Crossref, Medline, Google Scholar
5. Clark DB, Winters KC: Measuring risks and outcomes in substance use disorders prevention research. J Consult Clin Psychol 2002; 70:1207-1223Crossref, Medline, Google Scholar
6. Brook JS, Whiteman MM, Finch S: Childhood aggression, adolescent delinquency, and drug use: a longitudinal study. J Genet Psychol 1992; 153:369-383Crossref, Medline, Google Scholar
7. Blackson T, Butler T, Belsky J, Ammerman R, Shaw D, Tarter R: Individual traits and family contexts predict sons’ externalizing behavior and preliminary relative risk ratios for conduct disorder and substance use disorder outcomes. Drug Alcohol Depend 1999; 56:115-131Crossref, Medline, Google Scholar
8. Chassin L, Rogush F, Barrera M: Substance use and symptomatology among adolescent children of alcoholics. J Abnorm Psychol 1991; 100:449-463Crossref, Medline, Google Scholar
9. Tarter R, Blackson T, Brigham J, Moss H, Caprara G: Precursor and correlates of irritability: a two-year follow-up of boys at risk for substance abuse. Drug Alcohol Depend 1995; 39:2253-2261Google Scholar
10. Clark D, Parker A, Lynch K: Psychopathology and substance-related problems during early adolescence: a survival analysis. J Clin Child Psychol 1999; 28:333-341Crossref, Medline, Google Scholar
11. Biederman J, Wilens T, Mick E, Faraone SV, Weber W, Curtis S, Thornell A, Pfister K, Jetton JG, Soriano J: Is ADHD a risk factor for psychoactive substance use disorders? findings from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry 1997; 36:21-29Crossref, Medline, Google Scholar
12. Clark D, Sayette M: Anxiety and the development of alcoholism: clinical and scientific issues. Am J Addict 1993; 2:59-76Crossref, Google Scholar
13. Moffitt T, Heary B: Neuropsychological assessment of executive functions in self-reported delinquents. Dev Psychopathol 1989; 1:105-118Crossref, Google Scholar
14. Barkley RA: Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 1997; 121:65-94Crossref, Medline, Google Scholar
15. Aytaclar S, Tarter R, Kirisci L, Lu S: Association between hyperactivity and executive cognitive functioning in childhood and substance abuse in early adolescence. J Am Acad Child Adolesc Psychiatry 1999; 38:172-178Crossref, Medline, Google Scholar
16. Giancola P, Martin C, Tarter R, Moss H, Pelham W: Executive cognitive functioning and aggressive behavior in preadolescent boys at high risk for substance abuse. J Stud Alcohol 1996; 57:352-359Crossref, Medline, Google Scholar
17. Giancola P, Tarter R: Executive cognitive functions and risk for substance abuse. Psychol Sci 1999; 10:203-210Crossref, Google Scholar
18. Shoal G, Giancola P: Executive cognitive functioning, negative affectivity and drug use in adolescent boys with and without a family history of a substance use disorder. J Child Adolesc Subst Abuse 2001; 10:111-121Crossref, Google Scholar
19. Bauer L, Hesselbrock V: CSD/REM localization of P300 sources in adolescents “at risk”: evidence of frontal cortex dysfunction in conduct disorder. Biol Psychiatry 2001; 50:600-608Crossref, Medline, Google Scholar
20. Begleiter H, Porjesz B: What is inherited in the predisposition toward alcoholism? a proposed model. Alcohol Clin Exp Res 1999; 23:1125-1135Crossref, Medline, Google Scholar
21. Hill S, Sher S, Locke J, Steinhauer S, Konicky C, Lowers L, Connelly J: Developmental delay in P300 production in children at high risk for developing alcohol-related disorders. Biol Psychiatry 1999; 46:970-981Crossref, Medline, Google Scholar
22. Iacono W: Identifying psychophysiological risk for psychopathology: examples from substance abuse and schizophrenia research. Psychophysiology 1998; 35:621-637Crossref, Medline, Google Scholar
23. Blecker T, Ramchandari V, Flury L, Foround T, Karakenn D, Yee R, Li T-K, O’Connor S: Saccadic eye movements are associated with a family history of alcoholism at baseline and after exposure to alcohol. Alcohol Clin Exp Res 2002; 26:1568-1573Crossref, Medline, Google Scholar
24. Gorrenstein S, Newman J: Disinhibitory psychopathology: a new perspective and model for research. Psychol Rev 1980; 87:301-315Crossref, Medline, Google Scholar
25. Young S, Stallings M, Corley R, Krauter K, Hewitt J: Genetic and environmental influence on behavioral disinhibition. Am J Med Genet 2000; 96:684-695Crossref, Medline, Google Scholar
26. Tarter R, Vanyukov M: Introduction: Theoretical and operational framework for research into the etiology of substance use disorder. J Child Adolesc Subst Abuse 2001; 10:1-12Crossref, Google Scholar
27. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R (SCID). New York, New York State Psychiatric Institute, Biometrics Research, 1987Google Scholar
28. Leckman J, Sholomaskas D, Thompson W: Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry 1982; 39:879-883Crossref, Medline, Google Scholar
29. Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R: Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. J Am Acad Child Psychiatry 1982; 21:392-397Crossref, Medline, Google Scholar
30. Clark D, Pollock N, Mezzich A, Cornelius J, Martin C: Diachronic assessment and the emergence of substance use disorders. J Child Adolesc Subst Abuse 2001; 10:13-22Crossref, Google Scholar
31. Clark D, Moss H, Kirisci L, Mezzich A, Miles R, Ott P: Psychopathology in preadolescent sons of substance abuse. J Am Acad Child Adolesc Psychiatry 1997; 36:495-502Crossref, Medline, Google Scholar
32. Clark D, Kirisci L, Moss H: Early adolescent gateway drug use in sons of fathers with substance use disorders. Addict Behav 1998; 23:561-566Crossref, Medline, Google Scholar
33. Windle M: The Revised Dimensions of Temperament Survey (DOTS-R): simultaneous group confirmatory factor analysis for adolescent gender groups. Psychol Assess 1992; 4:228-234Crossref, Google Scholar
34. Kirisci L, Blackson T: Psychometric evaluation of the Dimensions of Temperament Survey, in Proceedings of the 1996 Annual Convention of the American Psychological Association. Washington, DC, American Psychological Association, 1996Google Scholar
35. Pelham W, Murphy D: The DBD Rating Scale: a parent and teacher rating scale for the disruptive behavior disorders of childhood in DSM-III-R. Pittsburgh, University of Pittsburgh Medical School, Department of Psychiatry, 1987Google Scholar
36. Tarter R: Evaluation and treatment of adolescent substance abuse: a decision tree method. Am J Drug Alcohol Abuse 1990; 16:1-46Crossref, Medline, Google Scholar
37. Kirisci L, Hsu T, Tarter R: Fitting a two-parameter logistic item response model to clarify the psychometric properties of the Drug Use Screening Inventory for adolescent alcohol and drug abusers. Alcohol Clin Exp Res 1994; 18:1335-1341Crossref, Medline, Google Scholar
38. Kirisci L, Mezzich A, Tarter R: Norms and sensitivity of the adolescent version of the Drug Use Screening Inventory. Addict Behav 1995; 20:149-157Crossref, Medline, Google Scholar
39. Hollingshead AB: Four-Factor Index of Social Status. New Haven, Conn, Yale University, Department of Sociology, 1975Google Scholar
40. Reckase MD: Unifactor latent trait models applied to multifactor tests: results and implications. J Educational Statistics 1979; 4:207-230Crossref, Google Scholar
41. Bollen KA: Structural Equation With Latent Variables. New York, John Wiley & Sons, 1989Google Scholar
42. Dawes M, Tarter R, Kirisci L: Behavioral self-regulation: correlates and 2 year follow-up for boys at risk for substance abuse. Drug Alcohol Depend 1997; 45:165-176Crossref, Medline, Google Scholar
43. Disney ER, Elkins IJ, McGue M, Iacono WG: Effects of ADHD, conduct disorder, and gender on substance use and abuse in adolescence. Am J Psychiatry 1999; 156:1515-1521Link, Google Scholar
44. Legrand L, McGue M, Iacono W: Searching for interactive effects in the etiology of early onset substance use. Behav Genet 1999; 29:433-444Crossref, Medline, Google Scholar
45. Caspi A, Moffitt TE, Newman D, Silva DA: Behavioral observations at age 3 years predict adult psychiatric disorders: longitudinal evidence from a birth cohort. Arch Gen Psychiatry 1996; 53:1033-1039Crossref, Medline, Google Scholar
46. Wong M, Zucker R, Puttler L, Fitzgerald H: Heterogeneity of risk aggregation for alcohol problems between early and middle childhood: nesting structure variations. Dev Psychopathol 1999; 11:727-744Crossref, Medline, Google Scholar



