Personality Diagnoses in Adolescence: DSM-IV Axis II Diagnoses and an Empirically Derived Alternative
Abstract
OBJECTIVE: The study of personality pathology in adolescence is in its infancy. This article examined the applicability and limits of DSM-IV axis II personality disorder diagnoses in adolescents, assessed the validity of a method for assessing adolescent personality pathology, and began to develop an empirically grounded classification. METHOD: A total of 296 randomly selected clinicians described a patient age 14–18 in treatment for maladaptive personality patterns using axis II ratings scales and the Shedler-Westen Assessment Procedure–200 for Adolescents (SWAP-200-A), a Q-sort instrument for assessing adolescent personality pathology. After examining the nature and frequency of axis II disorders in the sample, the authors used Q-factor analysis to identify naturally occurring groupings of patients on the basis of shared personality features. RESULTS: Axis II diagnoses in adolescents resembled those in adults, although application of DSM-IV criteria appeared to overdiagnose antisocial and avoidant personality disorder in adolescents. Q analysis with the SWAP-200-A isolated five personality disorders (antisocial-psychopathic, emotionally dysregulated, avoidant-constricted, narcissistic, and histrionic) and one personality style. Patients’ dimensional scores on each diagnostic prototype showed predictable associations with ratings of current axis II disorders, measures of adaptive functioning, and symptoms assessed with the Child Behavior Checklist. CONCLUSIONS: With some exceptions, personality pathology in adolescence resembles that in adults and is diagnosable in adolescents ages 14–18. Categories and criteria developed for adults may not be the optimal way of diagnosing adolescents. Data from samples of adolescents may prove useful in developing an empirically and clinically grounded classification of personality pathology in adolescents.
Although DSM-IV cautions against routine diagnosis of personality disorders in adolescents, a growing body of research over the last decade has suggested that personality syndromes are recognizable in adolescence (1–6). Longitudinal and epidemiological research suggests that 1) roughly 15% of adolescents in the community meet adult criteria for axis II disorders, a rate similar to that found in adult samples, 2) the presence of a personality disorder shows some stability over time, and 3) patients with an adolescent personality disorder are at a greater risk for both axis I and axis II conditions in young adulthood, even with childhood axis I diagnoses held constant (1, 7–9). Existing data suggest that despite substantial developmental changes in adolescence, enduring maladaptive personality characteristics can be assessed in the teen years, are not reducible to axis I disorders, and show predictive value above and beyond axis I diagnoses (10).
Indeed, data suggest that differences in personality styles within a diagnostic group, such as depression or conduct disorder in adolescence, may be of tremendous relevance to the understanding and treatment of patients with the disorder. For example, depressed adolescents with and without borderline personality disorder differ on multiple variables, including etiological variables such as history of abuse and family instability, and phenomenological variables such as rejection sensitivity, a tendency to view themselves as all bad or evil, dissociative symptoms, and so on (3–5). Conduct disorder similarly appears to be a heterogeneous diagnosis that includes at least two kinds of patients, one with an earlier onset and a more pernicious course and the other with a later onset and a much more variable course (6).
To what extent the personality disorder diagnoses represented on axis II provide an optimal way of classifying or diagnosing adolescent personality pathology is, however, unknown. The axis II literature suggests a number of potential pitfalls in extending these adult-derived diagnoses to adolescents, among the most important of which are the following (11). First, comorbidity among axis II personality disorders is high (12, 13); patients who receive one personality disorder diagnosis typically received three to six of the 10 in DSM-IV. Second, the axis II diagnostic criteria dichotomize symptoms as present or absent when, in reality, most of these variables are continuous and do not show clear breakpoints (e.g., identity confusion, social anxiety, or entitlement). They also dichotomize personality disorder diagnoses as present or absent (categorical diagnoses), whereas dimensional personality disorder diagnoses tend to show substantially higher reliability and validity for most disorders in most samples (14, 15). Third, axis II addresses only severe personality disturbances, which limits its use in diagnosing and treating problematic personality patterns not severe enough to warrant a personality disorder diagnosis (e.g., rejection sensitivity or low self-esteem). Such patterns appear to be at least as prevalent as diagnosable personality disorders (16), hence our use of the term “personality pathology” to describe the wider range of personality disturbances seen in adolescents and adults. Finally, problems of measurement plague research on personality disorders. Questionnaires and structured interviews show relatively weak convergence with one another and minimal convergence with clinical diagnosis as assessed with the LEAD (longitudinal evaluation using all available data) standard (17, 18). Complicating matters for extending these methods to adolescence is that, except for borderline personality disorder (3), reliable and valid measures of axis II pathology in adolescents do not exist. For the major study of the epidemiology of axis II disorders in the community (1), the investigators developed algorithms to piece together diagnoses from available self-report and interview data and felt confident reporting data only at the broad level of the three DSM-IV axis II clusters (A, B, and C).
These and other considerations suggest that if one is to employ or develop a system for classifying adolescent personality pathology, one would do well to consider the following. First, one should assess the operating characteristics of axis II diagnoses, treated both dimensionally and categorically, to see whether they function similarly in adolescents and adults. Second, following these analyses, one should use adolescent samples to derive diagnostic groupings using empirical techniques, such as factor analysis, cluster analysis, and other methods designed to reveal latent structure, rather than assuming the DSM-IV categories and criteria developed for (and from) adult samples. Optimally, these statistical procedures should be applied to broad item sets that encompass not only current and recent axis II criteria but also constructs identified as important through research on personality and developmental psychology relevant to adolescents. Third, one should not commit a priori to categorical diagnoses or diagnostic criteria. Fourth, instruments for assessing and classifying personality pathology should not assume that patients (particularly adolescents) have enough insight into their own personality processes to provide accurate self-descriptions. Furthermore, these instruments should be capable of capturing pathology across the full spectrum of adolescent personality functioning rather than just the most severe end of the distribution. Finally, a system for classifying personality pathology should be not only empirically grounded but also clinically relevant and useful.
The present article had three primary goals. The first was to provide data on the frequency and applicability of current axis II categories and criteria to a sample of adolescents treated in the community for personality pathology. The second goal was to assess the validity of a method for assessing adolescent personality pathology that could be used to assess axis II diagnoses as currently configured but could also be used to develop an alternative empirically derived classification system. The third goal was to use this method to make a first pass at developing an empirically grounded, developmentally sound, and clinically relevant system for classifying adolescent personality pathology and to provide initial data bearing on its validity by assessing associations between empirically derived diagnoses and DSM-IV axis II diagnoses, measures of adaptive functioning, and scores on the Child Behavior Checklist (19–23).
Method
Participants
To collect data on a large sample of adolescents with personality pathology, we used a practice research network approach, recruiting experienced clinicians to provide data. In a first wave of data collection, we recruited psychologists and psychiatrists from the membership roster of the American Academy of Child and Adolescent Psychiatry. Because of a low rate of response (approximately 20% of our total of initial letters of inquiry) to the first wave, in the second wave, we supplemented the list with a random sample of members of the American Psychological Association who were selected by computer search and who reported treating adolescents and had at least 3 years of posttraining practice experience. The rate of response of this latter sample was much higher (slightly less than 40%); approximately half submitted data for the present study.
Procedure
We sent clinicians an initial letter inquiring about their willingness to participate in a study of adolescent personality pathology and enclosed a postcard on which they could provide information about the number of patients in their practice of the following ages: 14, 15, 16, 17, and 18. Clinicians who agreed to participate subsequently received packets asking them to provide data on a randomly selected adolescent patient (operationalized as “the last patient you saw last week before completing this form who meets study criteria”) currently in treatment for “enduring maladaptive patterns of thought, feeling, motivation, or behavior—that is, personality.” To obtain an age-stratified sample, we asked clinicians to select a patient of a particular age (14, 15, 16, 17, or 18) on the basis of their initial survey response. To minimize rater-dependent variance, each clinician was asked to describe only one patient. We sent out packets in batches of 50–100, divided equally by age. On the basis of the number of packets received for each age group, we adjusted the numbers sent in the next batch by age to try to obtain roughly equal representation for each age. The clinicians who contributed data received an honorarium of $25.
The packets included the Shedler-Westen Assessment Procedure–200 for Adolescents (SWAP-200-A) (available at http://www.psychsystems.net/lab); measures of current axis II symptoms; a demographic, diagnostic, developmental, and family history questionnaire; and additional questionnaires measuring personality and symptoms. (Those relevant to the present study will be described.)
SWAP-200-A: A Q-Sort Instrument for Assessment of Adolescent Personality Disorder
A Q sort is a set of statements that provides a standard vocabulary for clinicians to use to describe their clinical observations. Each statement is printed on a separate index card. To describe a patient using the SWAP-200-A Q sort, a clinician sorts (rank orders) the statements into eight categories based on their applicability to the patient, from those that are irrelevant or not descriptive (assigned a value of 0) to those that are highly descriptive (assigned a value of 7). Statements that apply to a greater or lesser degree are placed into intermediate categories.
The SWAP-200-A is a Q-sort instrument for assessing adolescent personality pathology that is designed for use by skilled clinical observers, based on either longitudinal knowledge of the patient over the course of treatment or a systematic clinical interview of the patient and parents. The SWAP-200-A was adapted from its adult progenitor, the SWAP-200, which has shown initial evidence of validity, reliability, and utility in taxonomic research with adult samples (11, 24–27). Interviews and clinician diagnoses have predicted a range of measures of adaptive functioning, such as a history of hospitalizations and scores on the Global Assessment of Functioning Scale (DSM-IV), as well as etiological variables.
The item set for the adult version of the instrument was developed and revised over approximately 7 years and was subsequently adapted for adolescents. The items reflect constructs from a mixture of sources: axis II criteria for DSM-III through DSM-IV; selected symptoms currently represented by axis I criteria that are associated with personality disturbance and tend to be enduring (such as chronic depression and anxiety); clinical literature on personality disorders; research on personality disorders, normal personality traits, and psychological health (14, 28–30); a model of functional diagnosis that describes the range of personality functions used in a clinical case formulation (31); research on child and adolescent personality and psychopathology; videotaped clinical interviews; the clinical experience of the investigators; and feedback from more than 1,000 experienced clinicians. To develop the adolescent version of the instrument, we deleted, revised, and added items as appropriate on the basis of the adolescent literature, the authors’ prior research and experience with adolescent personality pathology, and consultation with senior adolescent clinicians who used the instrument to describe patients and then provided feedback on items that were ambiguous, necessary for describing their patient but missing from the item set, etc.
SWAP-200-A statements are written in a manner close to the data (e.g., “Tends to run away from home” or “Has an exaggerated sense of self-importance”), and items that require inference about internal processes are stated in simple language without jargon (e.g., “Tends to blame others for own failures or shortcomings” or “Tends to believe his/her problems are caused by external factors”). Thus, clinicians can use the SWAP-200-A regardless of their theoretical orientation. Empirically, clinicians’ theoretical orientation appears to have little impact on cluster- or factor-analytic solutions that emerge when using the SWAP-200 (24).
The Q-sort method normally requires that clinicians assign a specified number of items to each category (28). In the present study, which was the first to apply the SWAP-200-A to adolescents, clinicians used a semiconstrained rating scale version of the instrument, which did not require the use of a fixed distribution. Instead, they were given general guidelines on the number of items to assign a rating of 5, 6, or 7. We used this method in this study to evaluate whether the fixed distribution developed for adult patients is appropriate for an adolescent sample and to maximize the rate of response (because the sorting procedure takes considerably longer for adolescents).
Axis II Pathology
The clinicians assessed axis II pathology in multiple ways, both categorical and dimensional. We built in redundancy in data collection to maximize the reliability and validity of the data obtained. First, we asked clinicians to provide primary and secondary axis II (categorical) diagnoses, if applicable. Second, we listed the axis II disorders and asked the clinicians to rate the extent to which their patient met the criteria for each disorder (on a 7-point rating scale; 1=not at all, 4=has some features, 7=fully meets criteria). This provided a dimensional measure of axis II pathology. Third, we presented the clinicians with a checklist of all criteria currently included in axis II for all disorders, randomly ordered, and asked them to 1) rate each criterion as present or absent, as in the current diagnostic system and 2) rate the extent to which each item applied on a 1–7 scale. These checklist data generated two additional dimensional measures of axis II pathology (the number of diagnostic criteria endorsed as present for each personality disorder and the mean of the 1–7 ratings for each applicable criterion) as well as categorical diagnoses that were derived by summing the number of criteria present and applying DSM-IV rules regarding the number of criteria required for diagnosis. Similar methods have produced robust findings in previous research (e.g., references 32 and 33). (Because of a clerical error, one schizoid criterion was missing and two paranoid criteria were combined; hence, we reduced categorical diagnostic thresholds for each disorder by one.)
Clinical Data Form
The Clinical Data Form (available from http://www.psychsystems. net/lab) assesses a range of variables relevant to demographic characteristics, diagnosis, and etiology. Clinicians first provided basic demographic data on themselves and their patient, including their discipline (psychiatry or psychology), theoretical orientation, years of experience, employment sites (e.g., private practice, inpatient unit, school), sex, and race, as well as the patient’s age, sex, race, socioeconomic status, family composition, current living situation (e.g., one-parent home, foster care), axis I diagnoses, and so on. After answering basic demographic and diagnostic questions, clinicians rated the patient’s adaptive functioning, including school functioning (1=severe conduct problems/suspensions, 7=working to potential); peer functioning (1=very poor, 7=very good); history of suicide attempts, arrests, and hospitalizations; and social support (number of close confidantes in which the patient felt comfortable confiding). In prior research, we found such ratings to be highly reliable and to correlate strongly with ratings made by independent interviewers (34). The final section of the Clinical Data Form assesses aspects of the patient’s developmental and family history.
Child Behavior Checklist Data
The clinicians also completed a clinician-report adaptation of the parent form of the Child Behavior Checklist (19). Recent research from our laboratory (unpublished data) found that the clinician-report version of the instrument has similar psychometric properties to the parent- and teacher-report versions.
Statistical Analyses
Our first goal was to apply the axis II diagnostic criteria to adolescents to assess 1) the frequency in the sample of these disorders using the clinicians’ categorical diagnoses as well as diagnoses made by applying DSM-IV diagnostic algorithms to their axis II checklist data, 2) the extent to which axis II diagnoses operate similarly in adolescents and adults (e.g., produce similar patterns of co-occurrence of diagnoses), and 3) the extent to which these diagnoses are associated with criterion variables (measures of adaptive functioning and relevant Child Behavior Checklist scores) in ways that indicate the validity of diagnoses.
Our second goal was to assess the validity of the SWAP-200-A as a method for assessing current axis II diagnoses. The SWAP-200-A allows both dimensional and categorical diagnosis. For clarity of presentation, we present primarily dimensional diagnoses, although categorical diagnoses produced the same pattern of results. SWAP-200-A dimensional diagnoses reflect the magnitude of the correlation, or the degree of match, between an individual patient’s profile and a diagnostic prototype. We refer to these correlations (which can be converted to T scores for ease of interpretation, with a mean of 50 and standard deviation of 10) as dimensional personality disorder scores or, simply, personality disorder scores. (Categorical diagnoses simply involve establishment of cutoff points for the dimensional personality disorder scores.) To assess the validity of the instrument, we correlated SWAP-200-A personality disorder scores with the number of DSM-IV criteria met for each disorder, the measures of adaptive functioning, and Child Behavior Checklist scale scores.
Our next goal was to step back from existing diagnostic categories and criteria with the aim of making a first attempt at developing an alternative empirically derived diagnostic system for adolescent personality pathology. To identify naturally occurring groupings among the patients on the basis of their personality profiles, we applied a cluster-analytic technique, Q-factor analysis (or simply Q analysis), to data from the SWAP-200-A. Q analysis identifies groups of patients who are similar to one another and distinct from patients in other groups. The technique has been used successfully by biologists to aid in the classification of species and by personality psychologists to classify normal personality (28); more recently, it has been used in studies of the SWAP-200 and other Q-sort instruments with adult patients with personality and eating disorders and with troubled adolescents (11, 24–27).
Q-factor analysis can be understood in relation to conventional factor analysis, which identifies groups of variables that are highly similar to one another (i.e., highly intercorrelated). Q analysis is computationally the same procedure, except that it creates groupings of similar people—not variables. These groupings of people, called Q factors, represent empirically derived diagnostic prototypes—that is, aggregated portraits of particular kinds of people. In a typical data file, columns represent variables, and rows represent people. Factor analysis identifies columns of data that are highly intercorrelated, whereas Q analysis identifies similar rows of data. The computational procedure is identical and is accomplished simply by transposing the data matrix (i.e., exchanging rows and columns) before performing calculations. The Q analysis makes use of all 200 items in the SWAP-200-A to cluster patients and thus takes account of the configuration of personality characteristics across a broad range of psychological constructs, such as affectivity, affect and impulse regulation, interpersonal functioning, cognitive functioning, and experience of self and others.
As a first test of the validity of the classification system derived with Q analysis, we once again examined the association between the patients’ dimensional scores (this time for the empirically derived diagnoses rather than for the axis II diagnoses) and the three sets of criterion variables: dimensional assessments of axis II disorders, measures of adaptive functioning, and Child Behavior Checklist scale scores.
Results
Demographic Characteristics
The sample consisted of 296 patients. The clinician-respondents (61.4% psychiatrists, 50.2% men) were, on average, highly experienced (years of posttraining experience: mean=13.4, SD=9.4). The clinicians’ theoretical orientation was varied: 34.8% described themselves as psychodynamic; 11.6%, cognitive behavior; 6.5%, biological; 3.8%, family systems; and 42.7%, eclectic. Most worked in multiple settings: 77.0% in private practice, 31.3% in outpatient clinics, 25.8% in hospitals, 13.4% in schools, and 6.5% in forensics. The clinicians tended to know the patients well; the median length of treatment before completion of the questionnaire was 20 sessions.
The patients were relatively evenly distributed by gender (52.9% were girls) and age (for ages 14, 15, 16, 17, and 18, the numbers of patients per age were 54, 58, 67, 59, and 53, respectively) (some data were missing). The majority (84.9%) was white; most of the remaining patients were black or Hispanic. The clinicians rated the patients as poor (7.5%), working class (20.9%), middle class (50.7%), and upper class (20.9%). The most prevalent axis I diagnoses in the sample were major depressive disorder (25.3%), dysthymic disorder (24.3%), attention deficit hyperactivity disorder (16.1%), oppositional defiant disorder (9.0%), and conduct disorder (6.1%).
Diagnosing Adolescents With DSM-IV Axis II Criteria
Our first goal was to see whether personality disorders can be diagnosed in adolescents with DSM-IV categories and criteria as a first approximation. As described, we obtained categorical personality disorder diagnoses in two ways: by asking clinicians to provide a primary and secondary axis II diagnosis (where applicable) and by tallying the number of axis II criteria they checked off as present and applying DSM-IV cutoff rules. As in adult samples (unpublished data), the two methods produced different estimates of axis II pathology. According to the clinicians’ own categorical axis II diagnoses, only a minority of the patients received an axis II diagnosis (N=84, 28.4%). The most common diagnosis was borderline personality disorder (N=27, 9.1%), followed by borderline features (N=16, 5.4%). The only other diagnosis given to more than 2% of the sample was narcissistic personality disorder (N=9, 3.0%). As in studies of adults, the clinicians tended to give only one personality disorder diagnosis; only 10 clinicians in this sample offered a secondary axis II diagnosis.
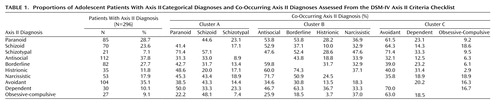
Far more patients received a categorical diagnosis when we tallied criteria directly from the axis II checklist. Table 1 provides categorical diagnoses of the sample with this second method, along with data for co-occurring disorders. Four findings are of note. First, 75.3% of the patients (N=223) received at least one axis II diagnosis; 36.8% (N=109) received cluster A diagnoses, 54.4% (N=161) received cluster B diagnoses, and 41.2% (N=122) received cluster C diagnoses. Second, as in adult studies, most patients who received one personality disorder diagnosis received many; of the patients who received any personality disorder diagnosis, approximately two-thirds received between two and nine. Third, the pattern of comorbidity in this sample was virtually identical to that found in adult samples. For example, patients with histrionic pathology tended to have borderline pathology, patients with schizoid pathology tended to score high on measures of schizotypal and avoidant personality disorders, and so forth. Dimensional diagnoses provided comparable findings, with correlations between disorders generally in the range of 0.30 to 0.60, showing extensive diagnostic redundancy. Finally, several disorders showed particularly high frequencies in the sample when diagnosed with adult criteria, most notably avoidant and antisocial personality disorders (likely corresponding to childhood internalizing and externalizing disorders, respectively). Taken as a whole, the data suggest that the distribution of axis II disorders in an adolescent sample was similar to that in adults, with the exception of higher rates of avoidant and antisocial diagnoses.
To see whether these diagnoses were meaningful in adolescents—that is, whether they had conceptually and clinically relevant antecedents and correlates—we examined the association between axis II diagnoses and measures of adaptive functioning and relevant factor scores on the Child Behavior Checklist. For simplicity, we report findings based on dimensional diagnoses, which provide readily interpretable effect-size estimates (Pearson’s correlations), although categorical analyses produced similar findings. Table 2 shows the correlations between axis II dimensional diagnoses (number of criteria met for each disorder) and 12 measures of adaptive functioning and symptoms: 7-point ratings of school functioning; 7-point ratings of peer relationships; number of close friends (a measure of social support); history of suicide attempts, psychiatric hospitalizations, and arrests (dummy coded 1 for present and 0 for absent); and six scale scores from the Child Behavior Checklist relevant to adaptive functioning. The data showed expected associations between axis II dimensional diagnoses and conceptually relevant criterion variables, such as a strong negative correlation between schizoid personality disorder and measures of social functioning and a high correlation with the score on the withdrawal scale on the Child Behavior Checklist. These data support the construct validity of the DSM-IV personality disorder diagnosis in adolescents.
Validity of the SWAP-200-A
The data presented thus far suggest that personality pathology, provisionally assessed by using axis II criteria, can be diagnosed in adolescents. Our next goal was to assess the validity of an instrument for assessing personality pathology that was designed for use with adolescents, the SWAP-200-A. As a first step, we examined the relationship between SWAP-200-A scores for each of the axis II disorders and the same measures of adaptive functioning and Child Behavior Checklist symptoms just described. To generate scores for each personality disorder, we correlated each subject’s SWAP-200-A profile with SWAP-200 prototype descriptions for each axis II disorder (derived from a normative sample of adult patients with personality disorders [12]). (To calculate these correlations, we deleted all items for which the adolescent version had no adult counterpart or vice versa, which led to deletion of eight items.) This provided us with a dimensional SWAP-200 diagnosis for each adolescent for each personality disorder. (Thus, a subject might have received a score of 0.55 for antisocial personality disorder, –0.13 for schizoid personality disorder, etc.; these scores indicate the correlation, or degree of match, between the patient’s profile and the SWAP-200 prototypes of the axis II personality disorders.)
Table 3 shows the correlations between the axis II personality disorders, as assessed dimensionally by using the SWAP-200-A, and the measures of adaptive functioning and the symptoms used to examine the validity of axis II diagnoses by using DSM-IV criteria. The pattern of findings strongly supported construct validity. For example, history of suicide attempts was associated with the borderline dimension, history of arrests was associated with the antisocial dimension, and strong school functioning (but not peer relationships) was associated with the obsessive-compulsive dimension. An additional Child Behavior Checklist finding (not reported on the table) was of note: a 0.41 correlation between schizotypal personality disorder scores on the SWAP-200-A and the Child Behavior Checklist thought problems scale (df=281, p<0.001). The data are also similar to those in Table 2, in which DSM-IV criteria were correlated with measures of adaptive functioning and Child Behavior Checklist scores and produced similar findings for the same disorders. Indeed, the median correlation between SWAP-200-A diagnoses and dimensional DSM-IV diagnoses (the number of symptoms met for each disorder) was 0.69.
Deriving an Empirically Based Taxonomy: Q Analysis
Having provided initial data supporting the validity of the SWAP-200-A as a method of assessing adolescent personality pathology, we next turned to the development of an empirically and clinically based classification. We applied Q analysis to the SWAP-200-A data using commonly accepted factor-analytic procedures. To determine the number of Q factors to extract, we performed an initial principal-components analysis and retained Q factors (principal components) with eigenvalues >1 (Kaiser’s criteria). These Q factors were then subjected to varimax (orthogonal) rotation. The first six of the rotated Q factors were theoretically coherent, readily interpretable, and accounted for 46.2% of the variance. Thus, we retained these six Q factors. Similar Q factors emerged when we rotated different numbers of factors using oblique and orthogonal solutions, although the solution described here yielded the most clinically coherent findings.
The first Q factor, or prototype, was composed of patients characterized by generally healthy functioning; these patients differed in type of pathology within a generally adaptive personality structure. (In Q-factor analysis, patients rather than items load on factors; the factor is defined by the patients with the highest loading on the factor.) Shapiro (35) described these patients in terms of neurotic styles. Because so many of the adolescents in the sample were grouped into this category, or Q factor, we conducted a second Q analysis to identify subgroups of patients within this large high-functioning group. This Q analysis paralleled the procedure described. We performed a principal-components analysis on the patients with loadings of 0.50 or above on this “healthy” Q factor. The scree plot suggested a break between two and five factors. We subjected the data to factor analysis with a varimax rotation. All solutions produced two robust factors (as did exploratory analyses with oblique rotations). We report the results of the three-factor solution, which accounted for 50.0% of the variance in the data set, retaining the first two of the three factors (together accounting for 36.7% of the variance). The first Q subfactor was again a Q factor for a general or psychological health index. The second factor is better described as a personality style than a personality disorder.
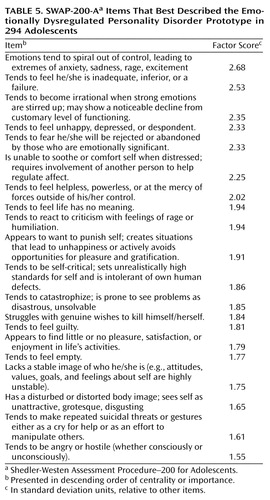
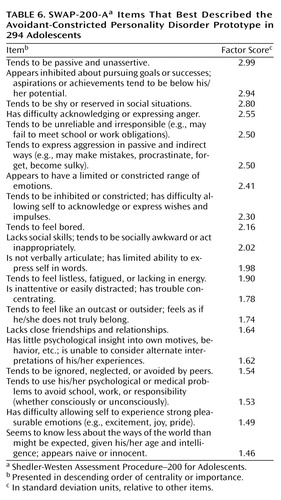
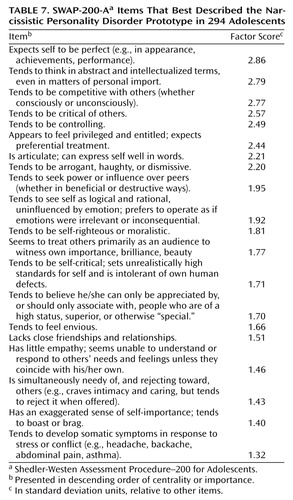
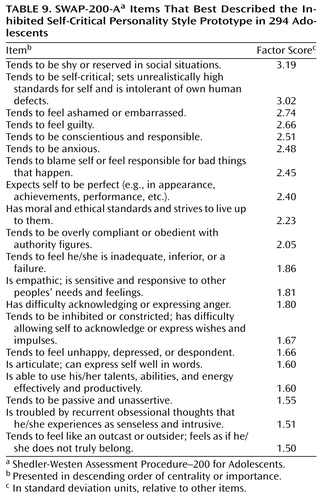
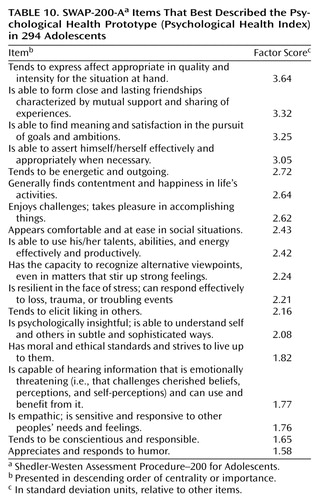
Table 4, Table 5, Table 6, Table 7, and Table 8 list the SWAP-200 items that best described the five empirically derived personality disorders. Table 9 and Table 10 describe the two subfactors derived from the first Q factor, which we labeled inhibited self-critical personality style and psychological health. The second column of each table shows the factor score for each item, which reflects its centrality or importance in defining the Q factor or prototype. (The factor scores are equivalent to factor scores in conventional factor analysis, except that they apply to items, not subjects.) The items in each table are listed in descending order of centrality or importance.
As the items in the tables make clear, the Q factors (diagnostic prototypes) require minimal interpretation. Many of these prototypes clearly resemble current axis II adult diagnoses, particularly the antisocial-psychopathic and narcissistic Q factors. The Q-factor prototypes, however, have an important advantage over axis II categories because they are statistically independent and nonoverlapping and were derived from an adolescent sample. All five personality disorder prototypes and the inhibited self-critical personality style strongly resemble Q factors that emerged empirically in a similar study of adult patients with personality disorders (27). Of note are two kinds of patients (emotionally dysregulated and histrionic) that are conceptually related to the DSM-IV borderline construct but are nonoverlapping, one characterized by intense, dysphoric emotions and desperate efforts to escape them and the other characterized by intense, dramatic emotions, along with a number of features currently defined as borderline or dependent.
Validity of the Empirically Derived Taxonomy
As a first test of the validity of this diagnostic system, we created dimensional scores for each patient, which we called Q scores and which index the match or degree of fit between the patient’s 200-item personality profile and each of the empirically derived diagnostic prototypes listed in Table 4, Table 5, Table 6, Table 7, Table 8, Table 9, and Table 10 (see the Statistical Analyses section). We then correlated these scores with the three sets of criterion variables used earlier (axis II diagnoses, measures of adaptive functioning, and Child Behavior Checklist symptom scales) to try to paint a clearer picture of the relation between these prototypes and constructs that are currently well known and better understood (that is, to locate the prototypes within a nomological net provided by existing constructs). Axis II diagnoses and Child Behavior Checklist scales are particularly useful as criterion variables or benchmarks because they provide the primary way clinicians and researchers currently classify enduring, maladaptive patterns of thought, feeling, motivation, and behavior in adolescents. Because many of the Q factors are similar to current axis II diagnostic categories, these analyses allowed us to assess, for example, whether patients with high scores on our antisocial-psychopathic Q factor also received high-dimensional scores for antisocial personality disorder as currently defined. Furthermore, because the item content of many of the empirically derived prototypes included features characteristic of more than one current axis II disorder (e.g., our histrionic prototype included borderline and dependent features as well as histrionic), we were also able to assess the extent to which these empirically derived groupings have predictable secondary associations with other disorders. (In these analyses, to obtain the most reliable estimate of axis II pathology as criterion variables—essentially assuming the constructs but not the specific algorithms in DSM-IV for measuring them—we generated composite dimensional axis II ratings by z-scoring the three-dimensional personality disorder ratings made by clinicians [the number of criteria endorsed as present for each personality disorder, the mean 7-point ratings of each personality disorder criterion for each disorder, and the 7-point global personality disorder ratings for each personality disorder] and took the mean of the z scores.) Measures of adaptive functioning are similarly useful because they provide relatively objective indices that any classification of personality pathology must be able to predict.
Table 11 shows the correlations between the patients’ Q scores (scores on each Q factor or prototype, which index the extent to which the patient matches the prototype) and composite axis II ratings. The data provide initial construct validity for the empirically derived classification system that, for example, generates an antisocial-psychopathic diagnosis that correlates strongly with DSM-IV antisocial personality disorder. At the same time, the data also show ways that axis II may make diagnostic distinctions that are not optimal for adolescents. For example, the avoidant-constricted Q factor correlated with the three DSM-IV disorders characterized by social withdrawal (schizoid, schizotypal, and avoidant), which all correlate highly with one another in adult studies as well. This finding suggests that these diagnostic distinctions are not empirically supportable in this adolescent sample (as many of them have not proven supportable in adult samples). Additionally, borderline personality disorder, as defined by adult axis II criteria, is associated with both the emotionally dysregulated and histrionic Q factors; however, these empirically derived Q factors were empirically distinct and nonoverlapping in our sample (as they are in several prior studies with adult samples; see reference 11).
Next, we examined the correlations between Q scores and measures of adaptive functioning and Child Behavior Checklist scores. As Table 12 shows, the pattern of correlations strongly supports construct validity. For example, as predicted, the inhibited self-critical personality style did not show the uniformly negative correlations with the measures of adaptive functioning as did the personality disorders but was associated with internalizing pathology. The other prototypes showed predictable correlates, including relatively objective criteria (e.g., suicide attempts, arrests) that require little or no clinical inference and hence avoid potential confounds entailed by the same observer (the clinician), providing both personality descriptions and data assessing the validity of empirically derived prototypes.
Discussion
Within the limitations of the method, the primary findings of this study are as follows. Supporting research using very different methods (1), the data suggest that personality pathology exists and is diagnosable in adolescence. Axis II diagnoses operate similarly in adolescents and in adults and predict criterion variables in expected ways. At the same time, axis II criteria produce high rates of diagnostic comorbidity and appear to diagnose relatively diffuse symptoms of externalizing and internalizing pathology as antisocial and avoidant personality disorder, respectively. The SWAP-200-A holds promise as a measure of personality pathology in adolescence that can be useful both in assessing current axis II disorders and in taxonomic work aimed at developing a more clinically relevant, developmentally sound classification system. Q analysis of data from the SWAP-200-A yielded an empirically derived classification system that avoided problems of comorbidity and produced diagnostic prototypes that were clinically coherent and correlated in predictable ways with criterion variables.
Assessing Axis II Disorders in Adolescents
Personality disorder diagnoses do appear to be applicable to adolescents ages 14–18. Using axis II criteria, we found patterns of co-occurring personality disorders similar to those in adult samples, and as we report elsewhere, factor and cluster analyses of the DSM-IV criteria produced structures that strongly resemble the axis II categories developed for adults. Furthermore, axis II diagnoses correlated with measures of adaptive functioning and symptoms in predictable ways with adult criteria, suggesting substantial convergence between the constructs used in adolescence and adulthood.
The data also highlighted problems applying axis II to adolescents. Of particular concern are the high rates of comorbidity seen in this sample, which strongly resembled adult data. More specific to adolescents was the high percentage of patients diagnosed with antisocial and avoidant personality disorders (upward of 30% each, as assessed with axis II criteria and cutoffs). Although this could reflect characteristics of the sample or an accurate portrait of adolescent personality pathology, a more likely explanation is that axis II criteria overpathologize adolescent acting out and place depressed or anxious adolescents in an overinclusive avoidant category.
As in adult samples, when asked to make categorical (present/absent) diagnoses, clinicians diagnose personality disorders with far less frequency than is implied by their endorsement of specific symptoms when these symptoms are aggregated by using DSM-IV diagnostic algorithms. This discordance could reflect any of three possible causes. First, clinicians could simply have inadequate knowledge of DSM-IV criteria and cutoffs. Second, instead of mentally reviewing each of the 80 criteria in axis II and counting them, clinicians may be using a prototype-matching approach to diagnosis, whereby they diagnose patients by gauging the degree of matching between the patient’s personality and a mental prototype (i.e., a template or schema) of each axis II personality disorder. Whether a prototype-matching process of this sort yields more or less valid diagnoses than application of DSM-IV diagnostic algorithms has never, to our knowledge, been tested. This would require examination of their comparative validity in predicting variables relevant to etiology, prognosis, and treatment response—a task worthy of future research. A third possibility is that axis II criteria may overpathologize personality features that are normative in adolescence or in adolescent clinical groups and that clinicians discount certain data (e.g., the presence of identity confusion or rage at parents) on the basis of developmental considerations.
Validity of the SWAP-200-A
The data provide initial support for the SWAP-200-A as an instrument for assessing personality pathology in adolescents. Dimensional personality disorder scores constructed by correlating patients’ SWAP-200-A descriptions with prototypes of each DSM-IV axis II disorder correlated in expected and conceptually meaningful ways with other ways of assessing axis II disorders; with multiple measures of adaptive functioning, such as measures of school and peer functioning and history of hospitalizations, suicide attempts, and arrests; and with Child Behavior Checklist scores.
Research with the adult version of the instrument (the SWAP-200) suggests multiple advantages of use of this method to assess personality pathology. Among the most important are the mounting evidence for its validity, its ability to assess personality strengths as well as weaknesses across the broad spectrum of mild and severe personality disturbances, its capacity to quantify clinical judgment on the basis of all available data longitudinally over the course of treatment by an experienced clinician as well as by research interviews, its usefulness for taxonomic work, and its capacity to provide both a descriptive and a functional assessment of personality, thus integrating diagnosis and case formulation (27, 31). A strong benefit specific to assessment of adolescent psychopathology is its potential use in integrating knowledge from multiple sources. Whereas structured interviews encounter difficulties when teenagers and their parents provide conflicting information, the SWAP-200-A does not tie specific criteria to specific questions or informants. Instead, the clinician or interviewer integrates all available data and observations, including clinical judgments about believability, coherence of explanations, and soon, to arrive at a SWAP-200-A description of the patient.
An Empirically Derived Classification of Adolescent Personality Pathology
Whereas axis II criteria provide overlapping diagnoses in adolescence, Q analysis produced empirically and clinically coherent diagnostic prototypes that cover the range of adolescent personality pathology, from the relatively severe (antisocial psychopathic) to the relatively high functioning (inhibited self-critical). These diagnostic prototypes are, we believe, clinically recognizable as well as empirically grounded.
Several features of this classification are noteworthy. First, the antisocial-psychopathic Q factor strongly resembles the classic concept of psychopathy (36, 37). Particularly in adolescence, when criminal behavior or misconduct are common in the absence of psychopathic traits, the diagnosis of antisocial personality disorder should be reserved for individuals who lack empathy, show little remorse, seem impervious to consequences, and so forth. In adults, these traits taken together as a construct (psychopathy) have demonstrated criterion validity in multiple studies, predicting variables such as recidivism and response to experimental challenges (38). In adolescents, they appear to distinguish a more insidious early-onset delinquency from adolescent-onset delinquency, which has a much more variable prognosis (6, 39).
Second, as in two prior studies of adult samples, Q analysis isolated two distinct (orthogonal) personality configurations that share many features of what is currently diagnosed as borderline personality disorder that need to be clearly distinguished: an emotionally dysregulated diagnosis (characterized by intense, distressing, poorly modulated emotions that spiral out of control and lead to desperate attempts to regulate them) and a histrionic diagnosis (characterized by a dramatic rather than primarily dysphoric affect, classic histrionic traits such as seductiveness and theatrics, and borderline and dependent traits such as the tendency to form quick attachments, to be needy, and to fear rejection and aloneness). The replication of these two distinct Q factors in multiple samples, in both adolescents and adults, suggests that the comorbidity of borderline, histrionic, and dependent personality disorder observed in multiple studies of DSM-III, DSM-III-R, and DSM-IV criteria is a likely artifact of overlapping diagnostic categories and criterion sets that do not adequately reflect the natural distribution of personality pathology seen in clinical practice.
Third, Q analysis did not reproduce the multiple disorders currently included in DSM-IV that are characterized by social isolation (schizoid, schizotypal, and avoidant personality disorders). Rather, it produced only a hybrid avoidant-constricted diagnosis. Three explanations could account for this finding. First, three discrete disorders characterized by social withdrawal may not exist in adolescence. Second, low base rates of schizotypal pathology (and paranoid personality disorder, which also did not emerge in our Q analysis) may have prevented detection of distinctions among different types of withdrawn adolescents in our sample. Third, social-emotional peculiarities on a continuum with negative symptoms of schizophrenia and paranoid and subclinical thinking disturbances on a continuum with positive symptoms may represent personality traits rather than the broader, multifaceted configurations of psychological characteristics that have traditionally defined the construct of personality disorder (as in the preamble to axis II in DSM-IV). Traits of this sort are more likely to emerge with conventional factor analysis (which groups items to identify traits) rather than Q analysis (which groups patients to identify prototypes). Factor-analytic data from this sample suggest that this is, in fact, the case, as is the case for adult samples (unpublished data).
Fourth, the inhibited self-critical neurotic style represents a high-functioning version of internalizing pathology not captured by axis II. We believe the isolation of personality styles other than those severe enough to warrant a personality disorder diagnosis is important to the understanding and treatment of adolescent personality pathology and should be a focus of future research. Similarly, inclusion of a psychological health prototype as an index of global personality functioning appears to be a useful addition to axis II for both adolescents and adults; it can be used both to index clinically relevant strength and to track characterological change over the course of treatment.
The findings also provide initial evidence for the validity of this empirically derived diagnostic system. The diagnostic prototypes show strong and theoretically coherent associations with relevant criterion variables that index adaptive functioning, ranging from school and peer functioning to a history of suicide attempts, hospitalizations, and arrests, as well as with current axis II diagnoses and Child Behavior Checklist factor scores that index prominent domains of adolescent psychopathology.
Potential Objections and Limitations
The major potential objection to the findings is our reliance on one source of information for each patient—the treating clinician. Several considerations, however, limit the impact of this concern. First, most studies of personality disorders (and, indeed, of axis I disorders as well) rely on a single observer, usually the patient, either through self-report questionnaires or structured interviews. We believe the judgments of experts with an average of over 13 years of practice experience who have known the patient over an extended period of time (in this case, for 20 sessions on average) are likely to be at least as informative as either self-reports or judgments made in brief interviews that sample a cross-section of verbal behavior on a single day. This is particularly true given the potential confounds of state and trait that make assessment of personality disorders difficult, especially in adolescents. Nevertheless, further studies based on multiple data sources are clearly warranted.
Second, data from our laboratory suggest that ratings of adaptive functioning as well as SWAP-200 personality descriptions show high reliability and validity and strongly predict relevant criterion variables, as assessed by other observers (34). For example, SWAP-200 descriptions of patients made by their treating clinicians correlate strongly with SWAP-200 descriptions made by independent interviewers, with median correlations of r=0.80 (unpublished data), and ratings of global, peer, and occupational functioning showing interrater reliability of r>0.70. Furthermore, we used multiple measures of adaptive functioning to validate both axis II and SWAP-200-A diagnoses and relied on clinicians who varied in their training (psychiatrists and psychologists), theoretical orientations, and likely beliefs about the appropriateness of applying axis II criteria to adolescents, which minimized the likelihood of systematic sources of error stemming from rater biases. Perhaps most important, we included criterion variables, such as history of arrests and psychiatric hospitalizations, that were not dependent on any observer inferences, and these measures showed similar patterns of correlations as more inferential ratings.
A second limitation concerns the question of the durability of personality pathology in adolescence and the appropriateness of diagnosing personality pathology at all in teenagers, an issue we addressed in detail elsewhere (10). The data presented here are cross-sectional, and future research should surely employ longitudinal designs. However, multiple considerations converge in suggesting that recognizable forms of personality pathology can be observed in adolescents and that our diagnostic prototypes do indeed reflect robust personality constructs. These considerations include the similarity of the empirically derived prototypes to adult prototypes derived empirically and the item content, which clearly assesses personality and not states. Furthermore, we instructed clinicians to describe only enduring aspects of the patient’s personality, not state-dependent features; clinicians typically had seen the patients over a considerable period of time and hence could likely make such distinctions. In addition, as we report elsewhere, the prototypes remain strongly predictive of adaptive functioning even when axis I diagnoses such as conduct disorder are held constant. Ongoing research in our laboratory is testing whether patterns such as those we observed can be seen in 13- and 14-year-olds or emerge between early and late adolescence.
A third potential concern is the response rate. Although we would have preferred to have a higher rate of response, particularly from members of the American Academy of Child and Adolescent Psychiatry, the fact that clinician-participants received minimal compensation for a relatively time-consuming task and that many randomly selected members of the academy either did not meet study criteria or do not treat adolescents rendered a high rate of response unlikely. Furthermore, our aim was not to survey clinician attitudes, for which a random sample of clinicians unbiased by potential differences between responders and nonresponders would be essential; rather, our aim was to obtain a cross-section of adolescents with personality pathology treated nationally. An appropriate comparison for this study, given its aims, is a sample of patients typically included in studies of adolescent psychopathology, for whom representativeness is generally at least as problematic, given that the patients are usually treated in a single location (usually a university hospital), are willing to participate in a research study, and so forth.
A fourth limitation is the relatively small sample size for taxonomic work. Although the sample was large by the standards of personality disorder research, a larger sample would ensure that we did not fail to identify low-base-rate forms of personality pathology that might be better represented in larger samples. Research currently underway is attempting to address many of these limitations in a sample of 1,000 adolescents to see whether the personality prototypes identified here replicate our results and whether we can further differentiate personality configurations that were not identifiable with the present sample size. Future research should address the extent to which data provided by systematic clinical research interviews match those provided by treating clinicians, as they do with adults, and whether clinicians can apply these prototypes to adolescents in ways that enhance clinical practice, treatment, and prediction.
In summation, the data suggest that personality pathology exists and is diagnosable in adolescents. We should think carefully, however, about whether the optimal way to study and assess adolescent personality pathology is to apply adult diagnoses to adolescents or whether we might do better to develop ways of classifying personality pathology in adolescence that start with adolescent samples. In so doing, we could draw on the knowledge of what has and has not worked in the refinement of axis II over the last two decades and integrate that knowledge with a more specific understanding of adolescent development.
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
Received Aug. 17, 2001; revisions received April 5 and Sept. 5, 2002; accepted Oct. 12, 2002. From the Departments of Psychology and Psychiatry, Emory University. Address reprint requests to Dr. Westen, Department of Psychology and Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, 532 North Kilgo Circle, Atlanta, GA 30322; [email protected] (e-mail). Supported in part by NIMH grants MH-59685 and MH-60892. The authors thank the more than 300 clinicians who helped them refine the SWAP-200-A assessment instrument, including the 296 who participated in the present study.
1. Bernstein DP, Cohen P, Skodol A, Bezirganian S, Brook JS: Childhood antecedents of adolescent personality disorders. Am J Psychiatry 1996; 153:907-913Link, Google Scholar
2. Grilo CM, McGlashan TH, Quinlan DM, Walker ML, Greenfeld D, Edell WS: Frequency of personality disorders in two age cohorts of psychiatric inpatients. Am J Psychiatry 1998; 155:140-142Link, Google Scholar
3. Ludolph PS, Westen D, Misle B, Jackson A, Wixom J, Wiss FC: The borderline diagnosis in adolescents: symptoms and developmental history. Am J Psychiatry 1990; 147:470-476Link, Google Scholar
4. Westen D, Ludolph P, Misle B, Ruffins S: Physical and sexual abuse in adolescent girls with borderline personality disorder. Am J Orthopsychiatry 1990; 60:55-66Crossref, Medline, Google Scholar
5. Wixom J, Ludolph P, Westen D: The quality of depression in adolescents with borderline personality disorder. J Am Acad Child Adolesc Psychiatry 1993; 32:1172-1177Crossref, Medline, Google Scholar
6. Moffitt T, Caspi A, Dickson N, Silva P, Stanton W: Childhood-onset versus adolescent-onset antisocial conduct problems in males: natural history from ages 3 to 18 years. Dev Psychopathol 1996; 8:399-424Crossref, Google Scholar
7. Bernstein DP, Cohen P, Velez CN, Schwab-Stone M, Siever LJ, Shinsato L: Prevalence and stability of the DSM-III-R personality disorders in a community-based survey of adolescents. Am J Psychiatry 1993; 150:1237-1243Link, Google Scholar
8. Johnson JG, Cohen P, Skodol A, Oldham J, Kasen S, Brook JS: Personality disorders in adolescence and risk of major mental disorders and suicidality during adulthood. Arch Gen Psychiatry 1999; 56:805-811Crossref, Medline, Google Scholar
9. Kasen S, Cohen P, Skodol AE, Johnson JG, Brook JS: Influence of child and adolescent psychiatric disorders on young adult personality disorder. Am J Psychiatry 1999; 156:1529-1535Link, Google Scholar
10. Westen D, Chang CM: Adolescent personality pathology: a review. Adolesc Psychiatry 2000; 25:61-100Google Scholar
11. Westen D, Shedler J: A prototype matching approach to personality disorders: toward DSM-V. J Personal Disord 2000; 14:109-126Crossref, Medline, Google Scholar
12. Bell E, Jackson D: The structure of personality disorders in DSM-III. Acta Psychiatr Scand 1992; 85:279-287Crossref, Medline, Google Scholar
13. Oldham JM, Skodol AE, Kellman HD, Hyler SE, Rosnick L, Davies M: Diagnosis of DSM-III-R personality disorders by two semistructured interviews: patterns of comorbidity. Am J Psychiatry 1992; 149:213-220Link, Google Scholar
14. Livesley WJ (ed): The DSM-IV Personality Disorders. New York, Guilford, 1995Google Scholar
15. Widiger T, Frances A: Toward a dimensional model for the personality disorders, in Personality Disorders and the Five-Factor Model of Personality. Edited by Costa P, Widiger T. Washington, DC, American Psychological Association, 1994, pp 19-39Google Scholar
16. Westen D, Arkowitz-Westen L: Limitations of axis II in diagnosing personality pathology in clinical practice. Am J Psychiatry 1998; 155:1767-1771Link, Google Scholar
17. Pilkonis PA, Heape CL, Proietti JM, Clark SW, McDavid JD, Pitts TE: The reliability and validity of two structured diagnostic interviews for personality disorders. Arch Gen Psychiatry 1995; 52:1025-1033Crossref, Medline, Google Scholar
18. Spitzer RL: Psychiatric diagnosis: are clinicians still necessary? Compr Psychiatry 1983; 24:399-411Crossref, Medline, Google Scholar
19. Achenbach TM: Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington, University of Vermont, Department of Psychiatry, 1991Google Scholar
20. Cronbach L, Meehl P: Construct validity in psychological tests. Psychol Bull 1955; 52:281-302Crossref, Medline, Google Scholar
21. Livesley W, Jackson D: Guidelines for developing, evaluating, and revising the classification of personality disorders. J Nerv Ment Dis 1992; 180:609-618Crossref, Medline, Google Scholar
22. Millon T: Classification in psychopathology: rationale, alternatives, and standards. J Abnorm Psychol 1991; 100:245-261Crossref, Medline, Google Scholar
23. Robins E, Guze SB: Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry 1970; 126:983-987Link, Google Scholar
24. Shedler J, Westen D: Refining the measurement of axis II: a Q-sort procedure for assessing personality pathology. Assessment 1998; 5:335-355Crossref, Google Scholar
25. Westen D, Harnden-Fischer J: Personality profiles in eating disorders: rethinking the distinction between axis I and axis II. Am J Psychiatry 2001; 158:547-562Link, Google Scholar
26. Westen D, Shedler J: Revising and assessing axis II, part I: developing a clinically and empirically valid assessment method. Am J Psychiatry 1999; 156:258-272Abstract, Google Scholar
27. Westen D, Shedler J: Revising and assessing axis II, part II: toward an empirically based and clinically useful classification of personality disorders. Am J Psychiatry 1999; 156:273-285Abstract, Google Scholar
28. Block J: The Q-Sort Method in Personality Assessment and Psychiatric Research. Palo Alto, Calif, Consulting Psychologists Press, 1978Google Scholar
29. McCrae R, Costa PT Jr: Personality trait structure as a human universal. Am Psychol 1997; 52:509-516Crossref, Medline, Google Scholar
30. McCrae R, Costa P: Personality in Adulthood. New York, Guilford, 1990Google Scholar
31. Westen D: Case formulation and personality diagnosis: two processes or one? in Making Diagnosis Meaningful. Edited by Barron J. Washington, DC, American Psychological Association, 1998, pp 111-138Google Scholar
32. Blais M, Norman D: A psychometric evaluation of the DSM-IV personality disorder criteria. J Personal Disord 1997; 11:168-176Crossref, Medline, Google Scholar
33. Morey LC: Personality disorders in DSM-III and DSM-III-R: convergence, coverage, and internal consistency. Am J Psychiatry 1988; 145:573-577Link, Google Scholar
34. Westen D, Muderrisoglu S, Fowler C, Shedler J, Koren D: Affect regulation and affective experience: individual differences, group differences, and measurement using a Q-sort procedure. J Consult Clin Psychol 1997; 65:429-439Crossref, Medline, Google Scholar
35. Shapiro D: Neurotic Styles. New York, Basic Books, 1962Google Scholar
36. Cleckley H: The Mask of Sanity. St Louis, Mosby, 1941Google Scholar
37. Hare R, Hart S: Commentary on antisocial personality disorder: the DSM-IV field trial, in The DSM-IV Personality Disorders. Edited by Livesley WJ. New York, Guilford, 1995, pp 127-134Google Scholar
38. Bernstein A, Newman JP, Wallace JF, Luh KE: Left-hemisphere activation and deficient response modulation in psychopaths. Psychol Sci 2000; 11:414-418Crossref, Medline, Google Scholar
39. Moffitt T: “Life-course persistent” and “adolescent-limited” antisocial behavior: a developmental taxonomy. Psychol Rev 1993; 100:674-701Crossref, Medline, Google Scholar



