Obsessive-Compulsive Disorder in Adolescent Schizophrenia Patients
Abstract
OBJECTIVE: The co-occurrence of obsessive-compulsive disorder (OCD) in adult patients with schizophrenia has been increasingly recognized. However, the rate of OCD comorbidity in adolescent schizophrenia patients has yet to be systematically evaluated. METHOD: The rate of DSM-IV OCD was evaluated in 50 adolescent inpatients with schizophrenia or schizoaffective disorder. The severity of schizophrenia and OCD symptoms was assessed with the Scale for the Assessment of Positive Symptoms, Scale for the Assessment of Negative Symptoms (SANS), and Yale-Brown Obsessive Compulsive Scale. RESULTS: Thirteen schizophrenia patients (26.0%) also met the DSM-IV criteria for OCD. This subgroup scored significantly higher on the SANS subscale for affective flattening or blunting. The total SANS score positively correlated with the total Yale-Brown Obsessive Compulsive Scale score. CONCLUSIONS: A substantial proportion of adolescent schizophrenia inpatients have concomitant OCD. A prospective study is needed to evaluate the clinical course, response to treatment, and prognosis for this complex disorder.
A substantial proportion of adult schizophrenia patients also meet the DSM-IV criteria for obsessive-compulsive disorder (OCD) (1–5). Surprisingly, even though the onset of both disorders is usually in adolescence, the rate of OCD in adolescent patients with schizophrenia has not yet been evaluated, to our knowledge. Identification of OCD in schizophrenia patients may have neurobiological, prognostic, and therapeutic implications (1, 6, 7). The present study is part of an ongoing large-scale project aimed at evaluating the prevalence and clinical characteristics of OCD in schizophrenia patients across the life span. We sought to determine the prevalence of OCD in adolescent schizophrenia inpatients and hypothesized that this subgroup would exhibit more severe schizophrenia symptoms than their non-OCD schizophrenia counterparts.
Method
The study was conducted in the adolescent departments of two major Israeli mental health centers (Shalvata and Abarbanel). The study was designed to include 50 consecutively hospitalized patients who met the DSM-IV criteria for schizophrenia or schizoaffective disorder. This sample is representative of Israeli adolescent inpatients. Diagnosis was based on the Structured Clinical Interview for DSM-IV Axis I Disorders. The exclusion criteria were schizophreniform disorder, organic brain syndrome, mental retardation, pervasive developmental disorder, and substance-induced psychosis. Drug screening was performed to confirm drug-induced psychosis. All participants were physically healthy. The results of routine laboratory tests were normal.
Severity of schizophrenia symptoms was assessed by using the Scale for the Assessment of Positive Symptoms (SAPS) (8) and the Scale for the Assessment of Negative Symptoms (SANS) (9). A minimum score of 7 (mild OCD) on the Yale-Brown Obsessive Compulsive Scale (10) and a duration of at least 6 months were required for the diagnosis of clinically significant OCD. Occupational and social functioning were assessed by using the Global Assessment of Functioning Scale. The reliabilities of these instruments were satisfactory, as previously reported (4).
All clinical assessments were performed by one of us (A.N.), who was experienced in using rating instruments for schizophrenia and OCD. The study was approved by the institutional review boards, and written informed consent was obtained from the patients and their legal guardians after they received full explanations regarding study procedures.
Student’s t test, chi-square test, Bonferroni post hoc test, and Pearson’s correlation were used as appropriate.
Results
Of the 54 patients approached, 50 (32 boys, 18 girls; mean age=17.0 years, SD=2.1) consented to participate in the study. Eleven patients met the DSM-IV criteria for schizoaffective disorder, and 39 patients met the criteria for schizophrenia (18 paranoid type, 12 undifferentiated, seven disorganized, one catatonic, one residual). The four patients who refused participation did not differ in demographic and clinical characteristics from the participants. The mean age at schizophrenia onset for the total sample was 14.8 years (SD=2.2), the mean duration of schizophrenia was 2.2 years (SD=1.8), and the mean number of hospitalizations was 2.0 (SD=1.6). For 29 patients, this was the first hospitalization; for 21 patients, it was the second to sixth hospitalization.
Of the 50 patients in the study, 13 (26.0%) also met the DSM-IV criteria for OCD. Five had the paranoid type of schizophrenia, three disorganized, three undifferentiated, and one catatonic, and one subject had schizoaffective disorder. The mean score on the Yale-Brown Obsessive Compulsive Scale for these 13 patients was 20.5 (SD=6.8); the mean score on the obsession subscale score was 10.2 (SD=4.5), and the mean compulsion subscale score was 11.3 (SD=4.5). Within this subgroup, the ages at the onsets of schizophrenia and OCD were 15.1 (SD=2.4) and 14.3 (SD=2.8), respectively.
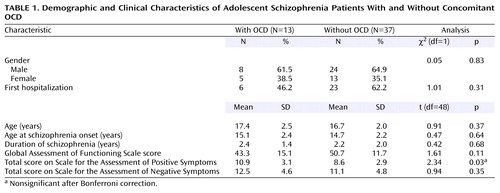
The schizophrenia patients with and without OCD did not differ in age, gender distribution, age at schizophrenia onset, duration of schizophrenia, or number of patients experiencing the first hospitalization (Table 1). There also were no between-group differences in Global Assessment of Functioning Scale score or in total scores on the SAPS and SANS (Table 1). However, the schizophrenia patients with OCD scored higher on the SANS subscale for affective flattening or blunting (mean=3.3, SD=0.9) than those without OCD (mean=2.2, SD=1.2) (t=3.16, df=48, p=0.003, significant after Bonferroni correction). Within the OCD schizophrenia group (N=13), the score on the Yale-Brown Obsessive Compulsive Scale showed a positive correlation with the total SANS score (r=0.68, p=0.03) but not the total SAPS score (r=0.46, p=0.11) score.
Discussion
In the present study, 26.0% of adolescent schizophrenia inpatients also met the diagnostic criteria for OCD. This finding is consistent with the results of most of the studies examining the rate of OCD in adult schizophrenia patients (1, 3, 4, 6, 11).
The schizophrenia patients with OCD did not differ significantly in their total SAPS, SANS, and Global Assessment of Functioning Scale scores from those without OCD. These results correspond with previous findings (4, 5) of no difference in the total scores for positive and negative symptoms between adult patients with chronic schizophrenia and OCD and adult schizophrenia patients without OCD. However, our patients with OCD scored significantly higher on the SANS subscale for affective flattening and blunting. A poorer prognosis for adult schizophrenia patients with OCD (1) and an association between negative symptoms and clinical outcome (12) have been suggested. It is noteworthy that in the current group of adolescents with OCD and schizophrenia, SANS scores positively correlated with the Yale-Brown Obsessive Compulsive Scale scores. Furthermore, despite the similar ages at onset of schizophrenia, a higher, although nonsignificant, percentage of our OCD patients than non-OCD patients required rehospitalization (53.8% versus 37.8%, respectively). Our findings suggest that the interaction of OCD and more severe schizophrenic (e.g., negative) symptoms creates a poorer prognosis for adolescent schizophrenic patients with OCD.
In conclusion, we have demonstrated that a substantial proportion of adolescent schizophrenia patients also suffer from OCD. Our study is preliminary and limited by the small sample size, the inclusion of inpatients only, and the lack of follow-up. In addition, this pilot exploratory study was not designed to compare the OCD rates in adolescents and adult schizophrenia populations (e.g., first-episode, chronic). Prospective studies are warranted in order to further evaluate and compare the co-occurrence of OCD and schizophrenia in adolescents and adults and the clinical course, response to treatment, and prognosis for this complex disorder.
 |
Received April 22, 2002; revision received Oct. 22, 2002; accepted Oct. 24, 2002. From the Adolescent Inpatient Department, Shalvata Mental Health Center, Hod Hasharon, Israel; the Research Unit, Tirat Carmel Mental Health Center and Faculty of Medicine, Israel Institute of Technology—Technion, Haifa, Israel; the Adolescent Inpatient Department, Abarbanel Mental Health Center, Bat Yam, Israel; the Department of Statistics and Operation Research and the Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel; the Clinical Psychopharmacology Unit, Tel Aviv Community Mental Health Center, Ramat Chen, Israel. Address reprint requests to Dr. Weizman, Tel Aviv Community Mental Health Center, 9 Hatzvi St., Ramat Hatayassim, Tel Aviv 67197, Israel; [email protected] (e-mail). Before his death in March 2002, Dr. Nechmad was a resident at the Shalvata Mental Health Center.
1. Fenton WS, McGlashan TH: The prognostic significance of obsessive-compulsive symptoms in schizophrenia. Am J Psychiatry 1986; 143:437-441Link, Google Scholar
2. Eisen JL, Beer DA, Pato MT, Venditto TA, Rasmussen SA: Obsessive-compulsive disorder in patients with schizophrenia or schizoaffective disorder. Am J Psychiatry 1997; 154:271-273Link, Google Scholar
3. Poyurovsky M, Fuchs C, Weizman A: Obsessive-compulsive disorder in patients with first-episode schizophrenia. Am J Psychiatry 1999; 156:1998-2000Abstract, Google Scholar
4. Poyurovsky M, Hramenkov S, Isakov V, Rauchverger B, Modai I, Schneidman M, Fuchs C, Weizman A: Obsessive-compulsive disorder in hospitalized patients with chronic schizophrenia. Psychiatry Res 2001; 102:49-57Crossref, Medline, Google Scholar
5. Berman I, Merson A, Viegner B, Losonczy MF, Pappas D, Green AI: Obsessions and compulsions as a distinct cluster of symptoms in schizophrenia: a neuropsychological study. J Nerv Ment Dis 1998; 186:150-156Crossref, Medline, Google Scholar
6. Tibbo P, Kroetsch M, Chue P, Warneke L: Obsessive-compulsive disorder in schizophrenia. J Psychiatr Res 2000; 34:39-46Crossref, Google Scholar
7. Poyurovsky M, Isakov V, Hromnikov S, Modai I, Rauchberger B, Schneidman M, Weizman A: Fluvoxamine treatment of obsessive-compulsive symptoms in schizophrenic patients: an add-on open study. Int Clin Psychopharmacol 1999; 14:95-100Crossref, Medline, Google Scholar
8. Andreasen NC: Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, University of Iowa, 1984Google Scholar
9. Andreasen NC: Scale for the Assessment of Negative Symptoms (SANS). Iowa City, University of Iowa, 1983Google Scholar
10. Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS: The Yale-Brown Obsessive Compulsive Scale, II: validity. Arch Gen Psychiatry 1989; 46:1012-1016Crossref, Medline, Google Scholar
11. Bermanzohn PC, Porto L, Arlow PB, Pollack S, Stronger R, Siris SG: Hierarchical diagnosis in chronic schizophrenia: a clinical study of co-occurring syndromes. Schizophr Bull 2000; 26:517-525Crossref, Medline, Google Scholar
12. Hwu HG, Tan H, Chen CC, Yeh LL: Negative symptoms at discharge and outcome in schizophrenia. Br J Psychiatry 1995; 166:61-67Crossref, Medline, Google Scholar



