Ziprasidone in the Treatment of Acute Bipolar Mania: A Three-Week, Placebo-Controlled, Double-Blind, Randomized Trial
Abstract
OBJECTIVE: The study evaluated the efficacy and tolerability of ziprasidone, compared with placebo, in the treatment of adult patients with acute bipolar mania. METHOD: Patients with a primary DSM-IV diagnosis of bipolar I disorder and a current manic or mixed episode (confirmed by the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition) (N=210) were randomly assigned in a 2:1 ratio to 3 weeks of double-blind treatment with ziprasidone (40–80 mg twice daily) or placebo. Efficacy was assessed with the Schedule for Affective Disorders and Schizophrenia, Change Version (which contains the Mania Rating Scale), Positive and Negative Syndrome Scale, Clinical Global Impression (CGI) severity scale, CGI improvement scale, and Global Assessment of Functioning Scale. Primary efficacy variables were differences from baseline to endpoint (last observation carried forward) in mean Mania Rating Scale and CGI severity scale scores between the ziprasidone and placebo groups. Safety evaluations included monitoring of adverse events, vital signs, electrocardiogram results, and clinical laboratory values and assessment of movement disorders and akathisia. RESULTS: Ziprasidone produced rapid, sustained improvements relative to baseline and placebo on all primary and most secondary efficacy measures at endpoint. Significant improvements were typically observed within 2 days after treatment commenced and were maintained throughout the 3 weeks. Ziprasidone was well tolerated and associated with a low rate of extrapyramidal symptoms; neither weight gain nor clinically significant changes in vital signs or other safety parameters were observed with ziprasidone. CONCLUSIONS: Ziprasidone monotherapy was significantly superior to placebo in reducing symptoms of acute mania in patients with bipolar I disorder. Onset of action was rapid, and tolerability of ziprasidone was generally comparable to that of placebo.
Three medications—lithium, divalproex, and olanzapine—have demonstrated efficacy in the treatment of acute bipolar mania in two or more randomized, placebo-controlled trials (1–8). In addition, carbamazepine and chlorpromazine were superior to placebo in treatment of acute mania in small clinical trials (9, 10). Despite the array of medications available to treat acute mania, many patients fail to respond adequately to monotherapy with these agents or experience treatment-limiting side effects (11).
Ziprasidone is an atypical antipsychotic agent with a unique receptor-binding profile. It is a potent antagonist of both serotonin 2A (5-HT2A) and dopamine D2 receptors, with an affinity for 5-HT2A receptors approximately 1,000-fold higher than that for D2 receptors. Ziprasidone also has high affinity for 5-HT1A receptors, where it acts as an agonist, and for 5-HT1D and 5-HT2C receptors (12). In addition, ziprasidone appears to inhibit reuptake of serotonin and norepinephrine (12). Studies in individuals with schizophrenia and schizoaffective disorder have shown that ziprasidone improves positive, negative, and associated depressive symptoms (13–15). In an analysis of ziprasidone’s thymoleptic activity in patients with schizoaffective disorder (bipolar and depressive subtypes), ziprasidone exerted dose-related reductions in manic and depressive symptoms compared with placebo (16). Pooled tolerability data from placebo-controlled trials demonstrated a favorable overall tolerability for ziprasidone (17), and the agent appears to be less likely to induce weight gain than other atypical antipsychotics, including clozapine, olanzapine, quetiapine, and risperidone (18).
Based on preliminary evidence of the efficacy of ziprasidone in improving mood symptoms, as well as psychotic symptoms (13–16), we conducted a large, randomized, controlled trial evaluating the efficacy and tolerability of ziprasidone as monotherapy for acute bipolar mania.
Method
Design
The efficacy and tolerability of oral ziprasidone was assessed in a 3-week, double-blind, placebo-controlled, randomized, parallel-group, multicenter trial (21 U.S. and three Brazilian sites) involving 210 inpatients.
Inclusion and Exclusion Criteria
Men and women >18 years of age with a primary DSM-IV diagnosis of bipolar I disorder and a current manic or mixed episode, confirmed by the Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-P) (19), were eligible for study participation. Patients were required to have a Mania Rating Scale (20) total score ≥14, with a score ≥2 on at least four items at screening and at baseline (within 12 hours before the first dose of double-blind medication).
Patients with schizophrenia, schizoaffective disorder, or acute bipolar I disorder with a current depressed episode were excluded from the study. Other exclusion criteria included DSM-IV-defined substance or alcohol abuse or dependence within the preceding 2 months and treatment with clozapine within 12 weeks, a depot antipsychotic within 4 weeks, or a monoamine oxidase inhibitor within 2 weeks of study baseline. Patients considered at high risk for suicide or violence were also excluded.
Women of childbearing age were eligible if they had undergone bilateral tubal ligation, hysterectomy, or bilateral total oophorectomy, were 1 year postmenopausal, or had tested negative at screening on a serum pregnancy test and had agreed to use investigator-approved contraceptive methods throughout the study. At screening, eligible patients were without clinically significant laboratory and ECG abnormalities and were 80% to 140% of ideal weight for sex, height, and frame as established in the Metropolitan Life Insurance Height and Weight Tables (21).
Patients with a history of clinically significant and currently relevant hematologic, renal, hepatic, gastrointestinal, endocrine, pulmonary, dermatologic, oncologic, or neurologic (including seizures or epilepsy) disease were excluded. Also ineligible were subjects with a history of significant cardiovascular disease, bypass surgery, or concurrent cardiovascular disease, including uncontrolled hypertension, hypotension, congestive heart failure, angina pectoris, or recent myocardial infarction (within the past 6 months). Anyone with a history of chronic hepatitis or with serologic evidence of acute or chronic hepatitis (positive hepatitis B surface antigen [HBsAg]) or hepatitis C antibodies and elevated liver enzymes, as well as those known to be infected with the human immunodeficiency virus, was also excluded.
Other reasons for exclusion included a history of hypersensitivity to antipsychotic compounds, a history of neuroleptic malignant syndrome developing from the administration of antipsychotic compounds, use of phencyclidine at any time during the 30-day period immediately preceding screening, use of any investigational drug within 4 weeks before screening, and treatment with ziprasidone in a previous clinical trial.
This study was conducted in compliance with the ethical principles originating from the 1989 Declaration of Helsinki. After complete description of the study, written informed consent was obtained from all participating patients.
Treatments
During screening, patients discontinued all psychotropic drugs except lorazepam, temazepam, and medications to manage movement disorders. Benzodiazepines other than lorazepam or temazepam were permitted only with the approval of a clinician employed by the sponsor (Pfizer Inc.) to monitor the study. Patients received single-blind placebo during a 1–7-day washout period. Patients were then randomly assigned in a 2:1 ratio to receive oral ziprasidone or placebo over a 3-week, double-blind treatment phase. Before the start of the study, we prepared a randomization list indicating the treatment assignment for each subject number. Drug treatment cards were numbered for each patient entering the double-blind phase, and the investigator or pharmacist allocated numbers to patients in sequence of entry into the study.
Ziprasidone (given with meals) was started at 40 mg b.i.d. on day 1, increased to 80 mg b.i.d. on day 2, and adjusted by a maximum of 40 mg/day within the range of 80–160 mg/day during the course of the trial. Placebo was given as matching capsules.
Lorazepam was permitted to treat agitation and anxiety (up to 8 mg/day from day 1 to day 7, up to 2 mg/day on days 8 and 9, and then discontinued). Temazepam (up to 30 mg/day) or, in the three Brazilian study centers, diazepam (up to 15 mg/day) was permitted as needed up to 3 days a week for insomnia throughout the study. None of these medications was permitted within 4 hours of study assessments, and a record was kept of the frequency of administration and the dose administered. The only other related medications allowed during double-blind treatment were benztropine and propranolol, which were given as needed for the management of Parkinsonian side effects and akathisia, respectively.
Evaluations
Efficacy
Efficacy was assessed by using the following instruments: Schedule for Affective Disorders and Schizophrenia, Change Version (SADS-C [20], which contains the Mania Rating Scale), Positive and Negative Syndrome Scale (22), investigator-rated Clinical Global Impression (CGI) severity scale (23), investigator-rated CGI improvement scale (23), and Global Assessment of Functioning Scale (23). Raters were blind to patients’ study medication. The SADS-C, CGI severity scale, and CGI improvement scale were administered at screening (except for the CGI improvement scale), at baseline (day 1, within 12 hours before the first dose), and on days 2, 4, 7, 14, and 21 (or at study termination, within 12 hours after the final dose). The Positive and Negative Syndrome Scale and Global Assessment of Functioning Scale were administered at baseline and on days 7, 14, and 21 (or at study termination). Sites were standardized on use of the SADS-C at an investigator meeting where videotaped interviews were rated and discussed.
Safety and tolerability
All observed or reported adverse events, including illnesses with onset during the study or exacerbations of preexisting illnesses, were recorded. Adverse events were evaluated for severity, duration, and possible relation to the study drug.
Parkinsonism was assessed with the Simpson-Angus Rating Scale (24) at screening, baseline, day 7, and day 21 (or study termination). Akathisia was evaluated with the Barnes akathisia rating scale (25) at the same times. Abnormal involuntary movements were assessed with the Abnormal Involuntary Movement Scale (AIMS) (23) at screening, baseline, and study endpoint. Treatment-emergent dystonic movements were recorded as adverse events, and the use of concomitant therapy for movement disorders (benztropine or propranolol) was recorded.
Laboratory assessments done only at screening included urine drug screening, hepatitis battery (HBsAg, hepatitis C antibodies), and plasma concentrations of lithium, carbamazepine, or valproate for patients receiving these medications at study entry. Tests performed at both screening and study endpoint included urinalysis, complete blood count with differential and platelet count, and blood chemistry, including thyroxine and thyroid-stimulating hormone. Blood pressure and pulse rate were measured at each visit, including screening, baseline, and study endpoint. A physical examination, including body weight measurement, and a 12-lead ECG were also performed at these times.
Data Analysis
The size of the study group was estimated on the basis of Mania Rating Scale parameters. A difference of 5 points on the Mania Rating Scale between treatment groups was deemed to be the smallest clinically relevant difference in endpoint values. The standard deviation of the Mania Rating Scale was expected to be less than 11.5. On the basis of these parameters, a study group of 200 subjects (133 taking ziprasidone and 67 taking placebo) was necessary to provide at least 80% power (alpha=0.05, two-tailed) to detect such a mean difference.
Background and demographic data were recorded and compared at baseline to ensure balance between the two treatment groups.
Efficacy analyses were performed on an intent-to-treat basis. All comparisons between the two treatment groups were analyzed for significance at the two-tailed 0.05 level. When appropriate, the last observation was carried forward to interpolate missing data.
Primary efficacy analyses were the differences from baseline to endpoint in mean Mania Rating Scale and CGI severity scale scores between the ziprasidone and placebo groups. These variables were assessed by using analysis of covariance (ANCOVA) models that included terms for study center, treatment, and the center-by-treatment interaction, with the baseline score used as a covariate.
Patients were identified as responders (decrease in Mania Rating Scale score ≥50% from baseline to specific time point) or nonresponders (decrease in Mania Rating Scale score <50% from baseline to specific time point) at each nominal protocol visit and endpoint visit (day 21 or termination). The treatment groups were compared by using a Cochran-Mantel-Haenszel test statistic with stratification by center.
Secondary efficacy analyses included the difference between the ziprasidone and placebo groups in mean changes from baseline to endpoint in scores on the manic syndrome subscale and behavior and ideation subscale of the Mania Rating Scale, the positive and total scores on the Positive and Negative Syndrome Scale, and the Global Assessment of Functioning Scale score. Groups were compared with respect to these variables by using ANCOVA, as described earlier. The mean CGI improvement scale scores at endpoint for the ziprasidone and placebo groups were also compared by using ANCOVA models.
Descriptive statistics were applied to clinical and laboratory safety data for each within-group parameter. These were then evaluated on the basis of tabular and graphic displays.
Results
Patient Demographics and Baseline Clinical Characteristics
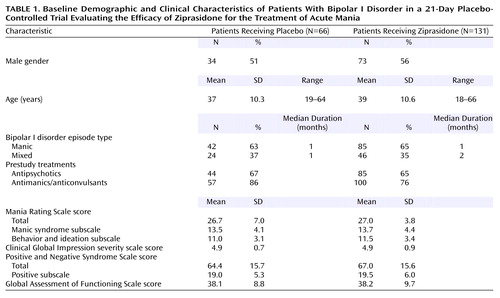
Of the 274 patients screened for study inclusion, 210 met the inclusion criteria and were randomly assigned to receive ziprasidone (N=140) or placebo (N=70). Data from all 210 patients were used in the evaluation of the safety of ziprasidone, and data from 131 and 66 patients in the respective treatment groups were used in the evaluation of efficacy. Eleven patients (eight assigned to receive ziprasidone and three to receive placebo), all at a single site, were excluded owing to data quality concerns (e.g., lack of sufficient source documentation to support collected data), and two patients (one in each group) were excluded because they lacked postbaseline data (Figure 1).
The demographic and baseline clinical characteristics of the study patients are summarized in Table 1. Patients with manic episodes constituted 65% and 63% of the ziprasidone and placebo groups, respectively. All others were classified as having mixed episodes. Prior treatment included antipsychotic medications for approximately two-thirds of those in both groups; more than three-quarters of the patients in each group had received antimanic drugs. At baseline, all patients had a Mania Rating Scale total score ≥14, and there were no statistically significant differences between the ziprasidone and placebo groups with respect to any primary or secondary variable.
Ziprasidone Dosing
The median duration of treatment for patients assigned to receive ziprasidone was 20.0 days. Eighty-seven of the 140 patients (62%) completed >14 days in randomized treatment. The mean ziprasidone dose was 81.3 mg (SD=24.5) on day 1 and 147.1 mg (SD=30.2) on day 2. Thereafter, the dose averaged 139.1 mg/day (SD=29.4) during days 8 to 14 and 130.1 mg/day (SD=34.5) during days 15 to 21. The median duration of dosing was 15.0 days for placebo-treated patients, of whom 36 of 70 (51%) completed >14 days.
Efficacy
Treatment with ziprasidone improved mood and other symptoms of acute mania in all primary and secondary efficacy variables. On day 2, the ziprasidone-treated patients demonstrated significant improvement in the Mania Rating Scale score, compared with placebo-treated patients. By day 7, the ziprasidone-treated patients showed significant improvement in all evaluation scales, compared with the placebo recipients. Intergroup differences increased throughout the second and third weeks of the study for all variables.
Mania Rating Scale and subscales
On the 11-item Mania Rating Scale, ziprasidone-treated patients achieved a reduction in mean score of 12.4 points (SD=12.0) from baseline to endpoint. Placebo-treated patients experienced a decrease of 7.8 (SD=12.9) over the same period. The difference between groups was significant (F=9.20, df=1, 164, p<0.005). Patients in the manic and mixed subsets had comparable improvement in Mania Rating Scale scores at endpoint (mean=–13.1, SD=12.8, and mean=–11.2, SD=10.6, respectively). A significant difference between the ziprasidone and placebo groups in mean change in the Mania Rating Scale score was evident by the second day of treatment and was maintained throughout the 21-day trial (Figure 2).Significantly more ziprasidone-treated subjects than placebo-treated subjects were classified as responders (50% versus 35%) (χ2=3.96, df=1, p<0.05).
The mean reductions in scores on the Mania Rating Scale manic syndrome subscale were 6.5 (SD=6.1) for the ziprasidone group and 4.8 (SD=6.7) for the placebo group (F=5.95, df=1, 164, p<0.05). The respective group decreases in scores on the behavior and ideation subscale were 5.1 (SD=5.4) and 2.7 (SD=5.9) (F=11.68, df=1, 164, p<0.001). On both subscales, significant between-group differences were evident by day 2 of dosing.
CGI severity scale
At endpoint, the mean CGI severity scale scores were reduced from baseline by 1.3 (SD=1.5) for ziprasidone-treated patients and by 0.9 (SD=1.6) for placebo-treated patients (F=7.27, df=1, 164, p<0.01). Patients in the manic and mixed subsets had comparable improvement in mean CGI severity scale scores (mean=–1.35, SD=1.55, and mean=–1.17, SD=1.43, respectively). Significant between-group differences were observed by day 4 of dosing.
CGI improvement scale
At endpoint, mean CGI improvement scale scores were 2.9 (SD=1.4) for the ziprasidone group and 3.5 (SD=1.7) for placebo group (F=15.06, df=1, 165, p<0.001). Significant between-group differences were observed by day 4.
Positive and Negative Syndrome Scale
At endpoint, the mean Positive and Negative Syndrome Scale positive symptom scores were reduced by 4.8 (SD=6.3) and 2.0 (SD=6.9) in ziprasidone- and placebo-treated patients, respectively (F=13.76, df=1, 156, p<0.001). The difference between groups was significant at every postbaseline assessment.
Global Assessment of Functioning Scale
At endpoint, mean Global Assessment of Functioning Scale scores had increased from baseline by 15.3 (SD=18.7) in the ziprasidone-treated patients and 8.3 (SD=18.7) in the placebo-treated patients (F=10.35, df=1, 156, p<0.005). A significant between-group difference in improvement in Global Assessment of Functioning Scale scores was evident by day 7 of the study (first postbaseline assessment with the Global Assessment of Functioning Scale).
Requirement for Benzodiazepines
Mean daily dosages and cumulative dosages for concomitant lorazepam, temazepam, and diazepam indicated that both treatment groups were generally similar in their requirements for supplementary benzodiazepines (Table 2).
Safety and Tolerability
Discontinuations
Discontinuation of treatment occurred in 46.4% (65 of 140) of patients assigned to receive ziprasidone and 55.7% (39 of 70) assigned to receive placebo. Those withdrawing because of insufficient treatment effect represented 19.3% (27 of 140) and 35.7% (25 of 70), respectively, of the two groups; those withdrawing because of adverse events, 6.4% (9 of 140) and 4.3% (3 of 70); and those withdrawing for other reasons, 20.7% (29 of 140) and 15.7% (11 of 70).
Adverse events
Treatment-emergent adverse events were experienced by 90.0% (126 of 140) of the ziprasidone-treated patients and 77.1% (54 of 70) of the placebo-treated patients. Adverse events judged by investigators to be treatment related occurred in 70.7% (99 of 140) and 54.3% (38 of 70) of patients in the respective groups. Nearly all of the treatment-related adverse events were rated mild or moderate in severity (96% of treatment-related adverse events for the ziprasidone group and 99% for the placebo group), and no serious treatment-related adverse events occurred in either group. Adverse events reported by ≥10% of patients in either group are summarized in Table 3. Reported more frequently in the ziprasidone group than in the placebo group were somnolence (37.1% versus 12.9%), headache (21.4% versus 18.6%), dizziness (22.1% versus 10.0%), hypertonia (11.4% versus 2.9%), nausea (11.4% versus 10.0%), and akathisia (10.7% versus 5.7%).
Analysis of movement disorders
Movement disorders were infrequent and resulted in discontinuations in two patients receiving ziprasidone. Scores on the Simpson-Angus Rating Scale, Barnes akathisia rating scale, and AIMS indicated no significant differences in the rating of movement disorders between patients receiving ziprasidone and those receiving placebo (Figure 3).
Laboratory values, vital signs, weight, and ECG
Clinically significant changes in laboratory values were infrequent and were found for fewer than 2% of patients in either group for any given assessment. No changes in median values for systolic or diastolic blood pressure or pulse were observed from baseline to endpoint in either group. No significant change in weight was seen with either treatment. The most common change in ECG parameters occurred in the QTc interval in the ziprasidone-treated patients, who experienced a mean prolongation of 11 msec over baseline values (Bazett’s correction). No patient had a QTc interval ≥500 msec while taking ziprasidone.
Discussion
In this study, ziprasidone was effective and well tolerated in patients with acute mania. Compared with placebo, ziprasidone treatment produced rapid and sustained improvement from baseline in the primary outcome measures of the Mania Rating Scale and CGI severity scale scores, with significant changes in these indices observed as early as the second day of treatment. Ziprasidone treatment was associated with significant improvement in scores on the manic syndrome and behavior and ideation subscales of the Mania Rating Scale by day 2. The mean change in Mania Rating Scale scores from baseline to endpoint in the ziprasidone group represented a 45% improvement. This change is comparable with the 37% and 51% reductions in the Young Mania Rating Scale score previously observed in 3-week and 4-week placebo-controlled trials of olanzapine in acute mania (3, 4). Similarly, a median 54% decrease was observed in a 3-week placebo-controlled trial of valproate (2). In a 3-week trial of divalproex, lithium, and placebo, both the divalproex group and the lithium group exhibited an approximately 35% improvement in the Mania Rating Scale score (1). However, magnitudes of improvement exhibited by agents in different trials must be compared cautiously, particularly when different instruments for rating mania have been employed.
Ziprasidone was well tolerated. The adverse events that were reported most frequently in the ziprasidone group, and more frequently in the ziprasidone group than in the placebo group, were somnolence, headache, and dizziness. Reports of movement disorders were uncommon, and observed changes on objective rating scales were generally comparable between the ziprasidone- and placebo-treated patients. Ziprasidone was not associated with weight gain or clinically significant ECG changes. The mean increase in QTc interval in this study was similar to the increase observed in clinical trials of ziprasidone in patients with schizophrenia and schizoaffective disorder (13–15). No patient had a QTc interval ≥500 msec while taking ziprasidone.
The tolerability profile of ziprasidone in this study is consistent with its pharmacologic activity and the generally favorable profile described for this agent in trials of patients with schizophrenia and schizoaffective disorder (13–15). These trials indicated a low incidence of specific adverse events commonly associated with antipsychotics such as weight gain, postural hypotension, anticholinergic side effects, and extrapyramidal symptom side effects (13–15, 17). The low incidence of extrapyramidal symptoms observed with ziprasidone compared with typical antipsychotics is a characteristic shared by other atypical agents (26–28) and has been attributed to the higher affinity of these drugs for 5-HT2A receptors than for D2 receptors (29).
In this study, the ziprasidone- and placebo-treated patients displayed a comparable requirement for supplementary benzodiazepine medication, as measured by both mean daily doses and cumulative doses. Thus, had the beneficial effects of ziprasidone in improving manic symptoms been due largely to the use of benzodiazepines, the placebo-treated patients would have experienced similar improvements. Instead, compared with placebo recipients, ziprasidone-treated patients demonstrated significant improvements on outcome measures as early as day 2 of treatment.
In summary, this double-blind, placebo-controlled study demonstrated that ziprasidone is effective and well tolerated in patients with bipolar I disorder who are experiencing acute mania. Ziprasidone therapy produced rapid and sustained improvement from baseline compared with placebo on all primary and the majority of secondary efficacy measures, thus demonstrating its capacity to ameliorate a wide range of symptoms in patients with mania. Significant improvements were typically observed by the second day of treatment and were maintained for the duration of the trial. Ziprasidone was generally well tolerated, was associated with a low rate of extrapyramidal symptoms, and was not associated with weight gain or clinically significant ECG abnormalities. These results suggest that ziprasidone is effective as monotherapy in the treatment of patients with bipolar mania.
 |
 |
 |
Received March 12, 2002; revision received Oct. 8, 2002; accepted Oct. 24, 2002. From the Department of Psychiatry, University of Cincinnati College of Medicine; Universidade Federal do Rio de Janeiro, Rio de Janeiro, Brazil; Department of Psychiatry and Human Behavior, University of California–Irvine, Irvine; CNS Healthcare, Orlando, Fla.; and Pfizer Global Research and Development, Pfizer Inc., New London, Conn. Address reprint requests to Dr. Keck, Biological Psychiatry Program, Department of Psychiatry, University of Cincinnati College of Medicine, 231 Albert Sabin Way, PO Box 670559, Cincinnati, OH 45627-0559; [email protected] (e-mail). The study medications used in this double-blind trial were provided by Pfizer Inc., New York. This study was supported by Pfizer Inc., New York. The authors acknowledge and thank the following co-investigators: Robert J. Birnbaum, M.D., Ph.D., Beth Israel Deaconess Medical Center, Boston; John S. Carman, M.D., Carman Research, Smyrna, Ga.; Franca Centorrino, M.D., McLean Hospital, Belmont, Mass.; James C.Y. Chou, M.D., New York Medical Center, New York; Larry Davis, M.D., Davis Clinic, PC, Indianapolis; Rif S. El-Mallakh, M.D., University of Louisville Hospital, Louisville; Richard Greenberg, Clinical Studies, Washington, D.C.; Robert Lynn Horne, M.D., Lake Mead Hospital, North Las Vegas, Nev.; Gunnar Larson, M.D., Zablocki Veterans Affairs Medical Center, Milwaukee; Joseph P. McEvoy, M.D., John Umstead Hospital, Butner, N.C.; Jerry Olsen, M.D., San Antonio State Hospital, San Antonio, Tex.; Fred Petty, M.D., Dallas Veterans Affairs Medical Center, Dallas; Christopher Reist, M.D., Long Beach Veterans Affairs Medical Center, Long Beach, Calif.; Robert Riesenberg, M.D., Atlanta Center for Medical Research, Decatur, Ga.; S. Craig Risch, M.D., Clinical Neuropharmacology Program, Charleston, S.C.; Jim Russell, M.D., University of Texas Medical Branch, Galveston, Tex.; Alan Swann, M.D., University of Texas Medical School, Houston; John Zajecka, M.D., Rush Hospital, Chicago; and Carlos A. Zarate, M.D., University of Massachusetts Medical School, Worcester, Mass.
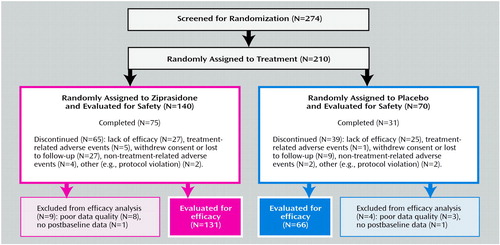
Figure 1. Summary of Participation of Patients With Bipolar I Disorder in Phases of a 21-Day Placebo-Controlled, Double-Blind, Randomized Trial of Ziprasidone in the Treatment of Acute Bipolar Mania
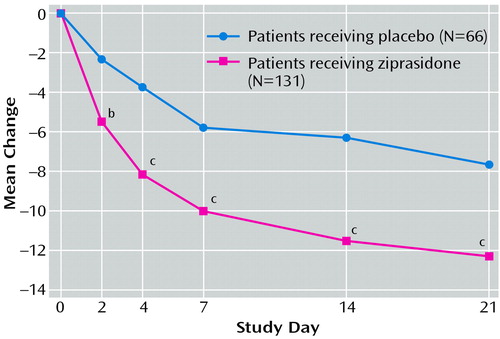
Figure 2. Mean Change in Mania Rating Scale Score From Baseline in Patients With Bipolar I Disorder in a 21-Day Placebo-Controlled Trial Evaluating the Efficacy of Ziprasidone for the Treatment of Acute Maniaa
aLast observation carried forward.
bSignificant difference between placebo-treated patients and ziprasidone-treated patients (p<0.003, F test).
cSignificant difference between placebo-treated patients and ziprasidone-treated patients (p<0.001, F test).
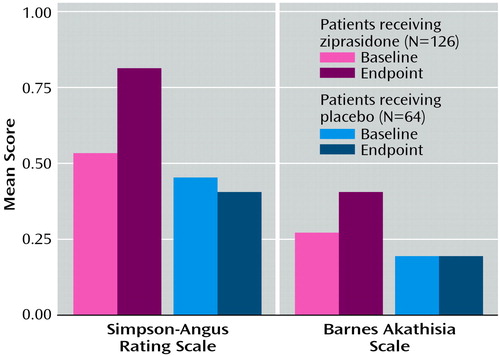
Figure 3. Scores on the Simpson-Angus Rating Scale and Barnes Rating Scale for Drug-Induced Akathisia at Baseline and Endpoint for Patients With Bipolar I Disorder in a 21-Day Placebo-Controlled Trial Evaluating the Efficacy of Ziprasidone for the Treatment of Acute Maniaa
aNo significant differences between groups were observed for changes in ratings between baseline and endpoint.
1. Bowden CL, Brugger AM, Swann AC, Calabrese JR, Janicak PG, Petty F, Dilsaver SC, Davis JM, Rush AJ, Small JG, Garza-Trevino ES, Risch SC, Goodnick PJ, Morris DD (Depakote Mania Study Group): Efficacy of divalproex vs lithium and placebo in the treatment of mania. JAMA 1994; 271:918-924Crossref, Medline, Google Scholar
2. Pope HG Jr, McElroy SL, Keck PE Jr, Hudson JI: Valproate in the treatment of acute mania: a placebo-controlled study. Arch Gen Psychiatry 1991; 48:62-68Crossref, Medline, Google Scholar
3. Tohen M, Sanger TM, McElroy SL, Tollefson GD, Chengappa KNR, Daniel DG, Petty F, Centorrino F, Wang R, Grundy SL, Greaney MG, Jacobs TG, David SR, Toma V (Olanzapine HGEH Study Group): Olanzapine versus placebo in the treatment of acute mania. Am J Psychiatry 1999; 156:702-709Abstract, Google Scholar
4. Tohen M, Jacobs TG, Grundy SL, McElroy SL, Banov MC, Janicak PG, Sanger T, Risser R, Zhang F, Toma V, Francis J, Tollefson GD, Breier A (Olanzapine HGGW Study Group): Efficacy of olanzapine in acute bipolar mania: a double-blind, placebo-controlled study. Arch Gen Psychiatry 2000; 57:841-849Crossref, Medline, Google Scholar
5. Goodwin FK, Murphy DL, Bunney WE Jr: Lithium-carbonate treatment in depression and mania: a longitudinal double-blind study. Arch Gen Psychiatry 1969; 21:486-496Crossref, Medline, Google Scholar
6. Maggs R: Treatment of manic illness with lithium carbonate. Br J Psychiatry 1963; 109:56-65Crossref, Google Scholar
7. Schon M, Juel-Nielson N, Stromgren E, Voldby H: The treatment of manic psychoses by administration of lithium salts. J Neurol Neurosurg Psychiatry 1954; 17:250-260Crossref, Medline, Google Scholar
8. Stokes PE, Shamoian CA, Stoll PM, Patton MJ: Efficacy of lithium as acute treatment of manic-depressive illness. Lancet 1971; 1:1319-1325Crossref, Medline, Google Scholar
9. Ballenger JC, Post RM: Therapeutic effects of carbamazepine in affective illness: a preliminary report. Commun Psychopharmacol 1978; 2:159-175Medline, Google Scholar
10. Klein DF: Importance of psychiatric diagnosis in prediction of clinical drug effects. Arch Gen Psychiatry 1967; 16:118-126Crossref, Medline, Google Scholar
11. Keck PE Jr, McElroy SL: Outcome in the pharmacologic treatment of bipolar disorder. J Clin Psychopharmacol 1996; 16(suppl 1):15S-23SGoogle Scholar
12. Schmidt AW, Lebel LA, Howard HR Jr, Zorn SH: Ziprasidone: a novel antipsychotic agent with a unique human receptor binding profile. Eur J Pharmacol 2001; 425:197-201Crossref, Medline, Google Scholar
13. Daniel DG, Zimbroff DL, Potkin SG, Reeves KR, Harrigan EP, Lakshminarayanan M (Ziprasidone Study Group): Ziprasidone 80 mg/day and 160 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 6-week placebo-controlled trial. Neuropsychopharmacology 1999; 20:491-505Crossref, Medline, Google Scholar
14. Keck P Jr, Buffenstein A, Ferguson J, Feighner J, Jaffe W, Harrigan EP, Morrissey MR: Ziprasidone 40 and 120 mg/day in the acute exacerbation of schizophrenia and schizoaffective disorder: a 4-week placebo-controlled trial. Psychopharmacology (Berl) 1998; 140:173-184Crossref, Medline, Google Scholar
15. Goff DC, Posever T, Herz L, Simmons J, Kletti N, Lapierre K, Wilner KD, Law CG, Ko GN: An exploratory haloperidol-controlled dose-finding study of ziprasidone in hospitalized patients with schizophrenia or schizoaffective disorder. J Clin Psychopharmacol 1998; 18:296-304Crossref, Medline, Google Scholar
16. Keck PE Jr, Reeves KR, Harrigan EP: Ziprasidone in the short-term treatment of patients with schizoaffective disorder: results from two double-blind, placebo-controlled, multicenter studies. J Clin Psychopharmacol 2001; 21:27-35Crossref, Medline, Google Scholar
17. Davis R, Markham A: Ziprasidone. CNS Drugs 1997; 8:153-159Crossref, Medline, Google Scholar
18. Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, Weiden PJ: Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 1999; 156:1686-1696Abstract, Google Scholar
19. First MB, Spitzer RL, Gibbon M, Williams JBW: Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P). New York, New York State Psychiatric Institute, Biometrics Research, 2001Google Scholar
20. Endicott J, Spitzer RL: A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia. Arch Gen Psychiatry 1978; 35:837-844Crossref, Medline, Google Scholar
21. Metropolitan Life Insurance Company: 1983 Metropolitan height and weight tables. Stat Bull Metrop Life Found 1983; 64:3-9Medline, Google Scholar
22. Kay SR, Fiszbein A, Opler LA: The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 1987; 13:261-276Crossref, Medline, Google Scholar
23. Guy W (ed): ECDEU Assessment Manual for Psychopharmacology: Publication ADM 76-338. Washington, DC, US Department of Health, Education, and Welfare, 1976, pp 534-537Google Scholar
24. Simpson GM, Angus JWS: A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl 1970; 212:11-19Crossref, Medline, Google Scholar
25. Barnes TRE: A rating scale for drug-induced akathisia. Br J Psychiatry 1989; 154:672-676Crossref, Medline, Google Scholar
26. Zarate CA Jr: Antipsychotic drug side effect issues in bipolar manic patients. J Clin Psychiatry 2000; 61(suppl 8):52-61Google Scholar
27. Meltzer HY, McGurk SR: The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr Bull 1999; 25:233-255Crossref, Medline, Google Scholar
28. Collaborative Working Group on Clinical Trial Evaluations: Assessing the effects of atypical antipsychotics on negative symptoms. J Clin Psychiatry 1998; 59(suppl 12):28-34Google Scholar
29. Glazer WM: Extrapyramidal side effects, tardive dyskinesia, and the concept of atypicality. J Clin Psychiatry 2000; 61(suppl 3):16-21Google Scholar



