The Relation Between Eating Disorders and Components of Perfectionism
Abstract
OBJECTIVE: The authors’ goal was to explore the relation between perfectionism and psychopathology, including eating disorders. METHOD: Using logistic regression, the authors calculated odds ratios for the associations between perfectionism subscale scores and psychiatric disorders in 1,010 female twins who completed the Multidimensional Perfectionism Scale and participated in diagnostic interviews. RESULTS: Elevated concern over mistakes was associated with anorexia and bulimia nervosa but not with other psychiatric disorders. Doubts about actions was associated with eating and anxiety disorders. Multivariable models confirmed that higher scores on the subscales for concern over mistakes and doubts about actions were most strongly associated with eating disorders. CONCLUSIONS: The aspect of perfectionism captured by scores on a subscale measuring concern over mistakes may be particularly associated with eating disorders and not generically predictive of psychopathology.
Perfectionism is a salient trait in women with anorexia nervosa and bulimia nervosa during acute illness (1, 2) and after recovery (3–5). Premorbid perfectionism may also be a risk factor for anorexia nervosa (6). These factors, together with reports of heritability estimates for perfectionism subscales ranging from 22% to 42% (unpublished paper by F. Tozzi et al.), suggest that perfectionism may be a risk factor for eating disorders and an endophenotype for genetic studies (2). Perfectionism may act in concert with low self-esteem or body dissatisfaction (7, 8).
The optimal definition of perfectionism is unclear. Several authors recommend using multidimensional scales rather than a global perfectionism score (9; unpublished study by F. Tozzi F et al.). The goal of the present study was to explore the association between components of perfectionism and seven common psychiatric disorders in a population-based sample of female twins and to determine the extent to which aspects of perfectionism are associated with anorexia nervosa and bulimia nervosa.
Method
Female-female twin pairs born from 1934 to 1974 from the population-based Virginia Twin Registry (10) participated in this study. These twins were interviewed four times between 1988 and 1997.
In 1999, questionnaires were mailed to all previous participants in the female-female twin study and a parallel male-male and opposite-sex twin study (11). Valid questionnaires were returned by 1,510 (49.5%) of 3,050 female twins. Limited resources prohibited follow-ups of nonresponders. Participants were all Caucasian, with a mean age of 42.5 years (SD=8.2). Final data were available for 1,010 members of female-female twin pairs who had returned the questionnaire and who had diagnostic information from previous interviews.
The questionnaire included 12 items from the Multidimensional Perfectionism Scale (12). The original Multidimensional Perfectionism Scale includes six subscales: concern over mistakes, doubts about actions, personal standards, organization, parental criticism, and parental expectations. On the basis of previous research on the Multidimensional Perfectionism Scale and communication with the scale developers, we included items focused on individual (rather than parental) characteristics. We chose four items each from the concern over mistakes and personal standards subscales that had shown reliable factor loadings in previous investigations (12, 13) (the original doubts about actions subscale includes only four items). Items were not included from the organization subscale because it is thought that this scale does not capture a core component of perfectionism (12).
Diagnostic data were available from previous interviews. Lifetime psychiatric and substance use disorders were diagnosed by using an adaptation of the Structured Clinical Interview for DSM-III-R (14) and DSM-III-R criteria with the following exceptions. First, we used broad definitions for several disorders—amenorrhea was not required for anorexia nervosa, and we eliminated the frequency and duration criteria for bulimia nervosa (15, 16). Second, a 1-month rather than 6-month minimum duration of illness for generalized anxiety disorder was used (17). Finally, diagnostic hierarchies were not used. The diagnostic algorithms, reliability, and interviewer training and qualifications are described elsewhere (11, 17–21). Written informed consent was obtained before face-to-face interviews, and verbal assent was obtained before telephone interviews. The studies from which these data were obtained were approved by the Virginia Commonwealth University Institutional Review Board and the Western Institutional Review Board.
We conducted logistic regressions using generalized estimating equations as operationalized in PROC GENMOD in SAS (22) to control for the correlated nature of twin data. We conceptualized the seven binary psychiatric diagnoses as dependent variables and the standardized perfectionism subscale scores as independent variables. Given the high rates of comorbidity in individuals with eating disorders, all analyses of other disorders controlled for the presence of anorexia nervosa and bulimia nervosa.
Results
Participation in this questionnaire was predicted by female gender (odds ratio=2.14, χ2=192.0, df=1, p<0.0001), older age (odds ratio=1.22 [per decade], χ2=82.1, df=1, p<0.0001), greater education (odds ratio=1.12 [per year], χ2=113.4, df=1, p<0.0001), and monozygosity (odds ratio=1.47, χ2=43.4, df=1, p<0.0001).
The prevalence of the seven psychiatric syndromes were 3.4% (N=34) for anorexia nervosa, 9.1% (N=92) for bulimia nervosa, 30.3% (N=306) for major depression, 16.6% (N=168) for alcohol abuse or dependence, 22.9% (N=231) for generalized anxiety disorder, 9.4% (N=95) for panic disorder, and 29.2% (N=295) for any phobia.
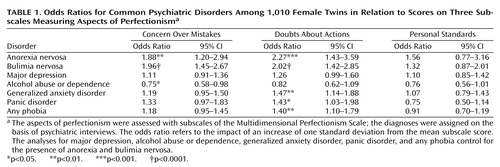
The correlations among the three perfectionism subscales were between concern over mistakes and personal standards (r=0.58), between personal standards and doubts about actions (r=0.29), and between doubts about actions and concern over mistakes (r=0.65). Table 1 shows the odds ratios and 95% confidence intervals for the univariate logistic regression analyses. Concern over mistakes was uniquely associated with significantly elevated odds ratios for anorexia nervosa and bulimia nervosa and was protective against alcohol abuse or dependence. Doubts about actions was associated with both anorexia nervosa and bulimia nervosa as well as panic disorder, generalized anxiety disorder, and phobia. There were no significant associations between any of the diagnostic categories and personal standards.
We then included concern over mistakes, doubts about actions, and personal standards in two regression models to predict anorexia nervosa and bulimia nervosa. With anorexia nervosa as the dependent variable, doubts about actions was a nonsignificant predictor of anorexia nervosa (beta=0.39, p=0.06). Concern over mistakes emerged as the only significant predictor of bulimia nervosa (beta=0.41, p=0.01).
Discussion
Confirming and extending previous clinically based knowledge, we found that elevated scores on a perfectionism scale—especially the aspect of perfectionism captured by the subscale for concern over mistakes—were significantly associated with the presence of anorexia nervosa and bulimia nervosa. This subscale measures negative reactions to mistakes and the tendency to interpret mistakes as failures. Concern over mistakes was not associated with elevations in any of the other psychiatric disorders assessed, although high scores were inversely associated with alcohol abuse or dependence. Multivariable regression models confirmed that, among the aspects of perfectionism that we measured, concern over mistakes and doubts about actions appear to be the most strongly associated with the presence of eating disorders.
High scores on the subscale for doubts about actions were more broadly associated with both eating and anxiety disorders, with high odds ratios for anorexia nervosa, bulimia nervosa, panic disorder, phobia, and generalized anxiety disorder. This subscale measures doubts about the ability to accomplish tasks and obsessional aspects of perfectionism. The fact that high scores for doubts about actions were associated with both eating and anxiety disorders (and not major depression or substance use disorders) provides additional evidence for the relation between these two classes of disorders. Indeed, a high percentage of individuals with eating disorders report comorbid anxiety disorders (23–28), which tend to persist after recovery from eating disorders (3–5). In addition, there is evidence of shared genetic factors between eating and anxiety disorders (29), and a unique genetic effect may contribute to symptoms of early eating and overanxious disorders (unpublished paper by J. Silberg and C. Bulik).
Previous investigations have shown that perfectionism is a salient clinical feature of both anorexia nervosa and bulimia nervosa. Although prospective studies have not assessed whether elevated perfectionism is a prospective risk factor, its persistence after recovery has led some to suggest that it may be a trait risk factor for eating disorders (24; unpublished study by J. Silberg and C. Bulik). Our current results suggest that the observed association between perfectionism and eating disorders is not confined to clinical samples and that the aspect of perfectionism captured by scores on a subscale measuring concern over mistakes may be most strongly associated with eating disorders and not generally predictive of psychopathology.
Limitations of this investigation include that the data collection was not prospective and, therefore, the emergence of perfectionism may be a consequence of an eating disorder. There may be other disorders that we did not assess (e.g., obsessive-compulsive disorder or obsessive-compulsive personality disorder) that are also associated with perfectionism. In addition, our response rate was not optimal, although predictors of response did not differ from previous interview waves and were typical for twin studies (30).
 |
Received June 7, 2002; revision received Aug. 22, 2002; accepted Sept. 17, 2002. From the Virginia Institute for Psychiatric and Behavioral Genetics, Department of Psychiatry, and the Department of Psychology, Virginia Commonwealth University. Address reprint requests to Dr. Bulik, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, PO Box 980126, Richmond, VA 23298-0126; [email protected] (e-mail). Supported by NIMH grants MH-01553, MH-40828, and MH-42953 and by grant AA-09095 from the National Institute on Alcohol Abuse and Alcoholism. The authors thank Kenneth Kendler, M.D., for enabling access to data from the Virginia Twin Registry.
1. Lilenfeld LR, Stein D, Bulik CM, Strober M, Plotnicov K, Pollice C, Rao R, Merikangas KR, Nagy L, Kaye WH: Personality traits among currently eating disordered, recovered and never ill first-degree female relatives of bulimic and control women. Psychol Med 2000; 30:1399-1410Crossref, Medline, Google Scholar
2. Halmi KA, Sunday SR, Strober M, Kaplan A, Woodside DB, Fichter M, Treasure J, Berrettini WH, Kaye WH: Perfectionism in anorexia nervosa: variation by clinical subtype, obsessionality, and pathological eating behavior. Am J Psychiatry 2000; 157:1799-1805Link, Google Scholar
3. Bastiani A, Rao R, Weltzin T, Kaye W: Perfectionism in anorexia nervosa. Int J Eat Disord 1995; 17:147-152Crossref, Medline, Google Scholar
4. Srinivasagam NM, Kaye WH, Plotnicov KH, Greeno C, Weltzin TE, Rao R: Persistent perfectionism, symmetry, and exactness after long-term recovery from anorexia nervosa. Am J Psychiatry 1995; 152:1630-1634Link, Google Scholar
5. Kaye WH, Greeno CG, Moss H, Fernstrom J, Fernstrom M, Lilenfeld LR, Weltzin TE, Mann JJ: Alterations in serotonin activity and psychiatric symptoms after recovery from bulimia nervosa. Arch Gen Psychiatry 1998; 55:927-935Crossref, Medline, Google Scholar
6. Fairburn CG, Cooper Z, Doll HD, Welch SL: Risk factors for anorexia nervosa: three integrated case-control comparisons. Arch Gen Psychiatry 1999; 56:468-476Crossref, Medline, Google Scholar
7. Vohs KD, Bardone AM, Joiner TE Jr, Abramson LY, Heatherton TF: Perfectionism, perceived weight status, and self-esteem interact to predict bulimic symptoms: a model of bulimic symptom development. J Abnorm Psychol 1999; 108:695-700Crossref, Medline, Google Scholar
8. Joiner TE Jr, Heatherton TF, Rudd MD, Schmidt NB: Perfectionism, perceived weight status, and bulimic symptoms: two studies testing a diathesis-stress model. J Abnorm Psychol 1997; 106:145-153Crossref, Medline, Google Scholar
9. Shafran R, Cooper Z, Fairburn C: Clinical perfectionism: a cognitive-behavioural analysis. Behav Res Ther 2002; 40:773-791Crossref, Medline, Google Scholar
10. Kendler K, Prescott C: A population-based twin study of lifetime major depression in men and women. Arch Gen Psychiatry 1999; 56:39-44Crossref, Medline, Google Scholar
11. Kendler KS, Prescott CA: A population-based twin study of lifetime major depression in men and women. Arch Gen Psychiatry 1999; 56:39-44; correction, 2000; 57:94-95Google Scholar
12. Frost RO, Marten P, Lahart C, Rosenblate R: The dimensions of perfectionism. Cognit Ther Res 1990; 14:449-468Crossref, Google Scholar
13. Rheaume J, Freeston M, Dugas M, Letarte H, Ladouceur R: Perfectionism, responsibility and obsessive-compulsive symptoms. Behav Res Ther 1995; 33:785-794Crossref, Medline, Google Scholar
14. Spitzer RL, Williams JBW, Gibbon M, First MB: Structured Clinical Interview for DSM-III-R—Patient Version 1.0 (SCID-P). Washington, DC, American Psychiatric Press, 1990Google Scholar
15. Sullivan PF, Bulik CM, Kendler KS: The epidemiology and classification of bulimia nervosa. Psychol Med 1998; 28:599-610Crossref, Medline, Google Scholar
16. Bulik CM, Sullivan PF, Kendler KS: Heritability of binge-eating and broadly defined bulimia nervosa. Biol Psychiatry 1998; 44:1210-1218Crossref, Medline, Google Scholar
17. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ: Generalized anxiety disorder in women. Arch Gen Psychiatry 1992; 49:267-272Crossref, Medline, Google Scholar
18. Kendler KS, Gardner CO, Prescott CA: Panic syndromes in a population-based sample of male and female twins. Psychol Med 2001; 31:989-1000Crossref, Medline, Google Scholar
19. Kendler KS, MacLean C, Neale MC, Kessler RC, Heath AC, Eaves LJ: The genetic epidemiology of bulimia nervosa. Am J Psychiatry 1991; 148:1627-1637Link, Google Scholar
20. Kendler KS, Heath AC, Neale MC, Kessler RC, Eaves LJ: Alcoholism and major depression in women. Arch Gen Psychiatry 1993; 50:690-698Crossref, Medline, Google Scholar
21. Kendler KS, Myers J, Prescott CA, Neale MC: The genetic epidemiology of irrational fears and phobias in men. Arch Gen Psychiatry 2001; 58:257-265Crossref, Medline, Google Scholar
22. SAS/STAT Software: Version 8. Cary, NC, SAS Institute, 1999Google Scholar
23. Braun DL, Sunday SR, Halmi KA: Psychiatric comorbidity in patients with eating disorders. Psychol Med 1994; 24:859-867Crossref, Medline, Google Scholar
24. Bulik C, Sullivan P, Fear J, Joyce P: Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatr Scand 1997; 96:101-107Crossref, Medline, Google Scholar
25. Deep A, Nagy L, Weltzin T, Rao R, Kaye W: Premorbid onset of psychopathology in long-term recovered anorexia nervosa. Int J Eat Disord 1995; 17:291-298Medline, Google Scholar
26. Halmi K, Eckert E, Marchi P, Sampugnaro V, Apple R, Cohen J: Comorbidity of psychiatric diagnoses in anorexia nervosa. Arch Gen Psychiatry 1991; 48:712-718Crossref, Medline, Google Scholar
27. Brewerton T, Lydiard R, Herzog D, Brotman A, O’Neil P, Ballenger J: Comorbidity of axis I psychiatric disorders in bulimia nervosa. J Clin Psychiatry 1995; 56:77-80Medline, Google Scholar
28. Bulik C, Sullivan P, Carter F, Joyce P: Lifetime anxiety disorders in women with bulimia nervosa. Compr Psychiatry 1996; 37:368-374Crossref, Medline, Google Scholar
29. Kendler KS, Walters EE, Neale MC, Kessler RC, Heath AC, Eaves LJ: The structure of the genetic and environmental risk factors for six major psychiatric disorders in women: phobia, generalized anxiety disorder, panic disorder, bulimia, major depression and alcoholism. Arch Gen Psychiatry 1995; 52:374-383Crossref, Medline, Google Scholar
30. Lykken DT, McGue M, Tellegen A: Recruitment bias in twin research: the rule of two-thirds reconsidered. Behav Genet 1987; 17:343-362Crossref, Medline, Google Scholar



