The Outcome of Anorexia Nervosa in the 20th Century
Abstract
OBJECTIVE: The present review addresses the outcome of anorexia nervosa and whether it changed over the second half of the 20th century. METHOD: A total of 119 study series covering 5,590 patients suffering from anorexia nervosa that were published in the English and German literature were analyzed with regard to mortality, global outcome, and other psychiatric disorders at follow-up. RESULTS: There were large variations in the outcome parameters across studies. Mortality estimated on the basis of both crude and standardized rates was significantly high. Among the surviving patients, less than one-half recovered on average, whereas one-third improved, and 20% remained chronically ill. The normalization of the core symptoms, involving weight, menstruation, and eating behaviors, was slightly better when each symptom was analyzed in isolation. The presence of other psychiatric disorders at follow-up was very common. Longer duration of follow-up and, less strongly, younger age at onset of illness were associated with better outcome. There was no convincing evidence that the outcome of anorexia nervosa improved over the second half of the last century. Several prognostic features were isolated, but there is conflicting evidence. Most clearly, vomiting, bulimia, and purgative abuse, chronicity of illness, and obsessive-compulsive personality symptoms are unfavorable prognostic features. CONCLUSIONS: Anorexia nervosa did not lose its relatively poor prognosis in the 20th century. Advances in etiology and treatment may improve the course of patients with anorexia nervosa in the future.
Anorexia nervosa received its present name only in the late 19th century (1). In the 20th century, critical analyses of epidemiological data showed that a true increase in the incidence and prevalence rates of anorexia nervosa over time was questionable (2, 3). Currently, the etiology of anorexia nervosa is not fully understood, with present models emphasizing its multifactorial origin, coupled with multiple determinants and risk factors and their interactions within a developmental framework (3).
Treatment of anorexia nervosa shifted in the second half of the 20th century from a purely medical approach that included reliance on neuroleptics in the 1950s and 1960s to a strong emphasis on individual psychotherapy (4), taking into account both a developmental and a biological framework (5) and the need for a multifaceted treatment approach (6). Later, both behavioral and cognitive interventions were added to treatment programs (7). In younger patients, the inclusion of family therapy has been advocated since the 1970s (3, 8). At the end of the 20th century, medications played a role in the treatment of some patients with anorexia nervosa, but they have been rarely used as the exclusive mode of intervention (9).
Selection criteria for the inclusion of studies in the present review were the following: 1) the study contained data on at least one of 15 outcome measures, and/or 2) the study contained data on any prognostic factor. Previous reviews of the outcome of anorexia nervosa by my associates and myself covered 45 studies (with 46 series of patients) published between 1953 and 1989 (10–56) and 23 additional follow-up studies (with 24 series of patients) published between 1981 and 1989 (57–80). Furthermore, Fichter and Quadflieg (81) discussed 22 additional series of anorectic patients (82–99; unpublished 1991 paper presented by Halmi). In addition to these three reviews, and based on a systematic search with PUBMED, I identified an additional 27 series of patients in outcome studies published between 1993 and 1999 (100–125). Thus, a total of 119 patient outcome series on anorexia nervosa were suitable for the present analysis. A preliminary and descriptive report on 108 patient outcome series published before 1996 (126) was used as a starting point for the present analysis. In addition to the 119 outcome series, there were five studies (127–131) that contained only data on prognostic factors suitable for the present review.
Study Characteristics
The 119 outcome series were composed of 5,590 patients (group size: mean=47.0, SD=30.8, range=6–151). There were considerable differences among the studies in design, group size, and methods. Few studies were prospectively organized. There was only one study based exclusively on male patients (65). Diagnostic categories changed considerably over the period of the studies, with virtually no official criteria existing at the time of the first study, to the appearance of the first research criteria, by Feighner et al. (132), and ending with more recent criteria offered by DSM-III, DSM-III-R, DSM-IV, and ICD-10.
Because of the global descriptions of age at onset in the studies, precise age parameters could not be computed. For the present review, the following two age groups were formed: 1) patient series containing only younger adolescent patients, i.e., no older than 17 years at illness onset (N=37), and 2) series containing both younger and older patients, i.e., adolescents and adults (N=82).
Duration of follow-up was also quite difficult to compute from the original studies. Besides missing data, this problem was due to variations in the definition of the starting point or to the general practice of providing only ranges instead of precise group parameters. Similarly, data on the follow-up period, which ranged from less than 1 year to a maximum of 29 years, did not allow a more precise calculation of group parameters. Almost all groups were characterized by a marked heterogeneity regarding the duration of follow-up. Thus, the present review classified not the mean but the entire range of follow-up duration for arrangement of the studies into the following groups: 1) 20 series with follow-up after less than 4 years, 2) 45 series with follow-up from 4 to 10 years later, 3) seven series with follow-up after more than 10 years to 20 years, 4) four series with follow-up after more than 20 years, and 5) 42 series with variable follow-up periods that did not fit into the other group). Because of low frequencies, groups 3 and 4 had to be collapsed for data analysis; because of the heterogeneity of data, group 5 was excluded from the analyses on the impact of duration of follow-up. There was one study with no clear description of the length of follow-up.
There were a general lack of control conditions and a scarcity of precise information on treatment in these studies. Different treatment and psychotherapeutic approaches were used. The diversity of interventions precluded any definite evaluation of treatment effects.
Outcome Measures
The majority of outcome studies on anorexia nervosa reported crude mortality rates; a small number of studies presented standard mortality ratios. The crude mortality rates may have been slightly inflated; not all studies reported the cause of death, so causes other than the eating disorder might have led to subject death. In the surviving patients, outcome was most frequently described as one or more of the following three categories: 1) global, 2) normalization of the core symptom characteristics of anorexia nervosa, i.e., involving weight, menstruation, and eating behavior, and 3) psychiatric diagnoses other than eating disorders.
The most common scheme of global outcome classification in anorexia nervosa was the trichotomy between good, fair, and poor outcome. Although the studies varied regarding criteria, there was a general agreement that a good outcome stands for recovery from all essential clinical symptoms of anorexia nervosa, whereas a fair outcome represents improvement with some residual symptoms, and a poor outcome is synonymous with chronicity of the disorder. A substantial number of studies used the criteria of Morgan and Russell (37), whereas other studies used more idiosyncratic definitions or did not report data for all three categories. The sum of the three categories did not necessarily round up to precisely 100%. In the present analysis, all reported data were included in calculations of the basic findings across studies. The original data that included mortality as a fourth outcome criterion in calculations of outcome percentages were adjusted into a three-category outcome, with mortality as a separate criterion. Thus, the potential inflation of crude mortality rates and the nonreported causes of death in some studies did not affect the outcome rates in the surviving patients.
In a substantial number of studies, psychiatric diagnoses in addition to eating disorders were mentioned. However, with the wide span of the dates of publication, a certain variation of criteria in the clinical assessment of psychiatric disorders other than the eating disorders needed to be accepted. The following eight psychiatric diagnoses were extracted from the outcome studies: 1) a broad category of affective disorders, 2) other neurotic disorders, including unspecified anxiety disorders and phobias, 3) obsessive-compulsive disorders, 4) schizophrenia, 5) histrionic personality disorder, 6) unspecified personality disorders, including borderline states, 7) obsessive-compulsive personality disorder, and 8) substance abuse disorders.
Statistical Analyses
A total of 15 outcome variables were calculated in percentages that were rounded to the nearest whole. In order to take into account the large variation of group sizes, weighted percentages were calculated by weighting each reported rate with the size of the study group. With the help of SPSS (SPSS, Chicago), data for all studies were converted into individual data for performance of statistical analyses. The following variables that may have influenced outcome were used in analyses of variance (ANOVAs): 1) dropout rate, 2) duration of follow-up, 3) age at illness onset, and 4) period effects. The ANOVAs were supplemented by post hoc comparisons and calculations of effect sizes by computing the percentage of variance (sum of squares between the groups divided by the total), according to the procedure introduced by Cohen (133). According to Cohen, 1.0%–5.9% variance is small, 6.0%–13.9% is medium, and >14.0% is large.
Results
Effects of Dropout Rates
In a large number of studies, conclusions were jeopardized by a relatively high dropout rate at follow-up. The mean dropout rate for the 105 patient series with some relevant information was 12.3% (SD=14.7, range=0–77). An analysis of dropout effects revealed an inconsistent pattern, with no clear indication that studies with high dropout rates tended to have better results because of nonparticipating patients with poor outcomes (data available on request).
Mortality and Global Outcome
Two important issues were considered. First, the sizes of the patient groups differed significantly for the various outcome measures, because not all variables were assessed in all studies. Second, for each measure, there were rather wide standard deviations with extreme ranges across the studies, so that the means reflected only a central trend.
The mean crude mortality rate was 5.0% (Table 1). In the surviving patients, on average, full recovery was found in only 46.9% of the patients, while 33.5% improved, and 20.8% developed a chronic course of the disorder. Outcome was slightly better for the core symptoms, with normalization of weight occurring in 59.6% of the patients, normalization of menstruation in 57.0%, and normalization of eating behavior in 46.8%. However, these slightly higher rates of normalization of the core symptoms, compared to the global outcome rating, may be largely due to the smaller total group sizes. Nevertheless, this gap remained, even after adaptation for group size (when only the studies that reported both global outcome ratings and normalization of the core symptoms were considered).
Other Psychiatric Disorders
The findings presented in Table 1 show that at follow-up a large proportion of anorectic patients suffered from additional psychiatric disorders. Frequent diagnoses at follow-up were neurotic disorders, including anxiety disorders and phobias, affective disorders, substance use disorders, obsessive-compulsive disorder (OCD), and unspecified personality disorders, including borderline states. A few studies reported a high rate of obsessive-compulsive personality disorder and a less pronounced rate of histrionic personality disorder. Schizophrenia was only rarely observed at follow-up.
Effect Variables
It was possible to control for three major factors that might have affected outcome. Their influence is reported only for mortality and the global outcome of the eating disorder in order to avoid conclusions that might be biased due to incomplete data or a markedly smaller group size for other outcome variables. Furthermore, only 61 studies that reported three global outcome categories (recovery, improvement, and chronicity) were considered for these analyses.
The first factor tested was duration of follow-up. Findings are shown in Table 2. All four outcome parameters were significantly affected by duration of follow-up, and all four effect sizes were large. With increasing duration of follow-up, mortality rates also increased. In the surviving patients, there was a strong tendency toward recovery with increasing duration of follow-up. The rate of recovery increased, while the rates of improvement and chronicity declined. With the exception of the test on improvement rates in groups 1 and 2, all post hoc tests indicated that group differences were significant. Given the significance of the follow-up duration, this variable was controlled in two-way ANOVAs in the additional analyses on the impact of age at onset of illness and the effects of period.
When I compared the group of patients with adolescent onset and the group with a much wider age range at onset of illness, there was a significantly lower mortality rate in the group with the younger patients, as shown in Table 3. The rates of recovery, improvement, and chronicity were more favorable in the group with the younger patients. However, in each instance, in addition to duration of follow-up, the interactions between duration of follow-up and each outcome variable were significant, as shown in Figure 1. The interaction effects showed that the differences between the subgroups with different onsets of illness were wider or narrower or even inverted for the four outcome measures, depending on the duration of follow-up. A comparison of the two effect sizes, as shown in Table 3, indicates that the effect of age at onset was stronger for mortality, whereas the effect of duration of follow-up was stronger for recovery, improvement, and chronicity.
The third effect tested was a potential period effect or time trend. The studies were divided into large groups, as follows: 1) studies from 1950 to 1979, 2) studies from 1980 to 1989, and 3) studies from 1990 to 1999. Mortality showed a complex pattern associated with time trends (Table 4). It was absent both for very short and very extended study courses in the early studies (with only one study each), from 1950 through 1979, whereas it increased linearly in the studies from 1980 to 1989 and from 1990 to 1999, with the highest rate for the most extended studies reported for 1980–1989. There were few differences between the studies for 1980–1989 and the studies for 1990–1999 on the other outcome measures—recovery, improvement, and chronicity—whereas the studies from 1950 to 1979 primarily stood out because of high recovery rates and low rates of improvement and chronicity during short-term courses (<4 years) (Figure 2). For all four outcome measures, the effect sizes for duration of follow-up were markedly stronger than for time period.
Prognostic Factors
Knowledge of the identified prognostic factors for anorexia nervosa is summarized in Table 5. First, the findings were considerably heterogeneous for the majority of the prognostic factors. Most clearly, this interpretation applies to the ambiguous findings regarding age at onset of illness. Furthermore, most studies indicated that a short duration of symptoms before treatment resulted in a favorable outcome. The impact of the duration of inpatient treatment is unclear because of ambiguous findings across the outcome studies. Similarly, no definite conclusions could be drawn as to whether greater weight loss at presentation had long-term effects on outcome.
Although hyperactivity and dieting as weight-reduction measures did not have any prognostic significance, it is quite clear that vomiting, bulimia, and purgative abuse imply an unfavorable prognosis. A few studies also showed that premorbid developmental and clinical abnormalities, including eating disorders during childhood, carry the risk for a poor outcome of anorexia nervosa. In contrast, a good parent-child relationship may protect the patient from a poor outcome.
In addition, the data clearly show that chronicity leads to poor outcome, a finding that implies that there are cases of anorexia nervosa in which treatment is refractory. A substantial number of studies provided evidence that the features of histrionic personality disorder indicate a favorable outcome. In contrast to comorbid OCD, which has no effect on outcome (118), the features of coexisting obsessive-compulsive personality or compulsivity add to chronicity. Finally, no definite conclusions can be drawn from the outcome studies as to the relevance of socioeconomic status.
Discussion
Besides use of a more extended database than in previous reviews, the present review on the outcome of anorexia nervosa is the first to my knowledge that was not confined to descriptive statistics only. For the first time an attempt was made to analyze trends by use of inferential statistics in order to isolate factors that might have influenced the course of anorexia nervosa in the last century. Findings based on this large group of 5,590 patients contained in a large number of studies indicate that despite wide variations of all outcome parameters across studies, anorexia nervosa remains a mental illness with a serious course and outcome in many of the affected individuals. This conclusion is based on various parameters analyzed in the present review.
First, crude mortality rates were high and increased significantly with length of follow-up. Even stronger evidence comes from a series of studies that calculated standard mortality rates. A review of the standard mortality rate in 10 cohort studies (134) found standard mortality rates between 1.36 and 17.80, indicating a slight to an almost 18-fold increase in mortality in patients with anorexia nervosa, with a maximal standard mortality rate of 30 for female patients in the first year after presentation and a statistically significant increase for up to 15 years after presentation. The data suggest that there are more deaths from suicide and other and unknown causes and fewer deaths related to the eating disorder than have been previously reported.
Second, less than a half of the patients, or exactly 46%, fully recovered from anorexia nervosa, whereas a third improved with only partial or residual features of anorexia nervosa, and 20% remained chronically ill over the long term. This relatively poor global outcome is slightly obscured if one looks in isolation at the better outcome of the core symptoms of weight restoration (60%) and normalization of both menstruation (57%) and eating behavior (47%).
A third outcome indicator of the seriousness of the course of anorexia nervosa—namely, other psychiatric disorders—shows that exactly one-quarter of the anorexia nervosa patients had anxiety disorders and one-quarter had affective disorders. Substance use disorders, OCD, and obsessive-compulsive personality disorder were very common diagnoses at outcome. Furthermore, there was evidence that some of these comorbidities—that is, depression, anxiety disorder, phobias, and personality disorders—served as risk factors contributing to a less favorable outcome of anorexia nervosa (78, 94, 105, 106). However, so far, little is known about the comorbidity of these various psychiatric disorders among each other, their true coexistence with anorexia nervosa, and the sequential patterns across time. The two parameters of global outcome and other psychiatric disorders overlap greatly, so that at follow-up, more than 50% of the anorexia nervosa patients showed either a complete or a partial eating disorder in combination with another psychiatric disorder or another psychiatric disorder without an eating disorder. However, an exact figure could not be obtained from the present data set.
There are two main factors mitigating the problematic outcome of anorexia nervosa, namely, duration of follow-up and age at onset of the disorder. In contrast to the strong effect of the increasing crude mortality rate, the global outcome in the surviving patients clearly improves with increasing duration of follow-up. The data indicate with strong effect sizes that with increasing duration of follow-up, the illness course improved linearly if the patient survived. Thus, it is recommended that clinicians follow up with patients for extended periods.
Onset of the disorder during adolescence was associated with a lower mortality rate and a strong effect size that was clearly more important than the duration of follow-up. This finding simply reflects the probabilistic event that more deaths are to be expected with increasing age. Although the other three general outcome measures were affected by age at onset, indicating that younger age at onset was associated with better outcome, the duration of follow-up was a more influential factor. However, two limitations of the analyses have to be taken into consideration. First, the group with variable age at onset was not the most suitable contrast to the group with adolescent onset because of the wide variation in age. A group of patients with adult onset only would be more appropriate for comparison. However, such a contrasting group was not available for study. Second, it must also be kept in mind that onset of anorexia nervosa before puberty has a very poor outcome (135).
Trends over five decades of outcome research are less clear. The early studies, from 1950 to 1979, provided evidence for lower mortality during long-term follow-up (>10 years) and higher recovery rates with short-term follow-up (<4 years). However, these findings must be accepted with caution. First, the mortality figures for long-term follow-up from 1950 to 1979 were based on one study, whereas the reductions in mortality at long-term follow-up for 1980–1989 and 1990–1999 were based on two and five studies, respectively. Second, there was a lack of a common definition for the three global outcome measures in the early studies, whereas those from 1980–1989 and 1990–1999 predominantly refer to the criteria of Morgan and Russell (37), which were introduced in 1975. Accordingly, the reliability of outcome measurement in the early studies may be questionable. With these caveats and the relatively small effect sizes in mind, there was only limited evidence that the outcome of anorexia nervosa has improved significantly across these five decades.
Research on the outcome of anorexia nervosa has also analyzed a large list of prognostic factors and produced both conflicting and clear evidence of their significance. There is clear and almost unanimous evidence from a sizable number of studies that vomiting, bulimia and purgative abuse, chronicity, and features of obsessive-compulsive personality represent unfavorable prognostic factors, whereas hysterical personality features represent the only favorable prognostic factors that have not been documented with conflicting evidence. The favorable functions of many other prognostic factors are obscured by the fact that besides some positive evidence, there are also a sizable number of studies that found these factors to be of no significance. These factors include early age at onset, short duration of symptoms before treatment, short duration of inpatient treatment, good parent-child relationship, and high socioeconomic status. Similarly, there was no clear evidence that major weight loss and premorbid abnormalities serve as unfavorable factors. Both the variability in findings on prognostic factors and the likely nature of the data preclude any delineation of rules as to individual prognosis in a patient suffering from anorexia nervosa.
So far, one of the major questions of developmental psychopathology as to the continuity and discontinuity of psychiatric disorder has received little attention in studies on the course of anorexia nervosa. Most of the studies have concentrated on outcome, leaving aside the process of course. Study of the latter requires prospective designs that have emerged only in the recent past. Some of these more recent studies have analyzed time trends of certain features of anorexia nervosa based on the survival-analysis model (116, 131, 136). Finally, the descriptive nature of data on treatment, the lack of rigorous evaluation of interventions in the majority of outcome studies, and the scarcity of randomized intervention studies with sufficient evaluation of outcome do not allow any definite statement as to the role and function of treatment for long-term course.
 |
 |
 |
 |
 |
Received May 18, 2001; revision received Oct. 30, 2001; accepted Jan. 28, 2002. From the Department of Child and Adolescent Psychiatry, University of Zurich. Address reprint requests to Dr. Steinhausen, Department of Child and Adolescent Psychiatry, University of Zurich, Neumünsterallee 9, Postfach, CH-8032 Zurich, Switzerland; [email protected] (e-mail). The author thanks C. Winkler Metzke for assistance with data analysis.
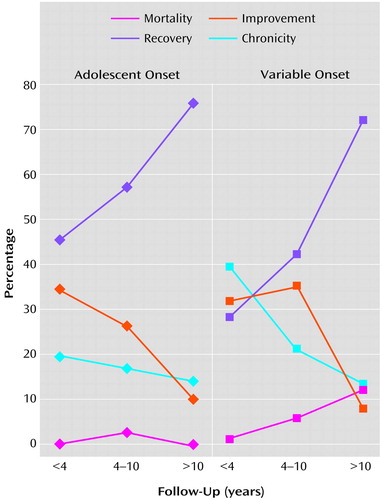
Figure 1. Outcome of Anorexia Nervosa in 119 Patient Series by Duration of Follow-Up and Age at Onseta
aA total of 577 patients had less than 4 years of follow-up, 2,132 had 4–10 years of follow-up, and 438 had more than 10 years of follow-up.
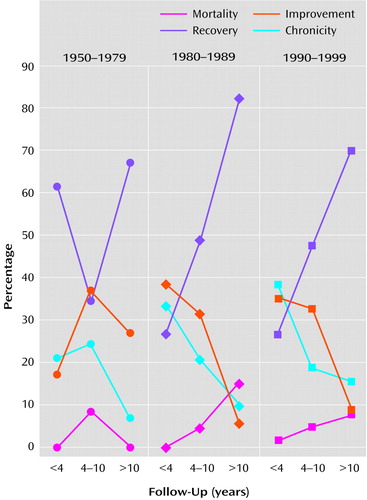
Figure 2. Outcome of Anorexia Nervosa in 119 Patient Series by Duration of Follow-Up and Time Period of Studya
aA total of 577 patients had less than 4 years of follow-up, 2,132 had 4–10 years of follow-up, and 438 had more than 10 years of follow-up.
1. Silverman JA: Anorexia nervosa: historical perspective on treatment, in Handbook of Treatment for Eating Disorders, 2nd ed. Edited by Garner DM, Garfinkel PE. New York, Guilford, 1997, pp 3-10Google Scholar
2. Fombonne E: Anorexia nervosa: no evidence of an increase. Br J Psychiatry 1995; 166:462-471Crossref, Medline, Google Scholar
3. Steinhausen HC: Anorexia and bulimia nervosa, in Child and Adolescent Psychiatry: Modern Approaches, 4th ed. Edited by Rutter M, Taylor E. Oxford, UK, Blackwell Scientific, 2002Google Scholar
4. Bruch H: Eating Disorders: Obesity, Anorexia Nervosa and the Person Within. New York, Basic Books, 1978Google Scholar
5. Crisp AH: Anorexia Nervosa: Let Me Be. London, Academic Press, 1980Google Scholar
6. Russell GFM: Anorexia nervosa: its identity as an illness and its treatment, in Modern Trends in Psychological Medicine, 2nd ed. Edited by Price JH. London, Butterworths, 1970, pp 131-164Google Scholar
7. Bemis KMM: The present status of operant conditioning for the treatment of anorexia nervosa. Behav Modif 1987; 11:432-463Crossref, Medline, Google Scholar
8. Vandereycken W: The place of family therapy in the treatment of eating disorders, in Eating Disorders in Adolescence: Anorexia and Bulimia Nervosa. Edited by Steinhausen HC. New York, Walter de Gruyter, 1995, pp 287-300Google Scholar
9. Garfinkel PE, Walsh BT: Drug therapies, in Handbook of Treatment for Eating Disorders, 2nd ed. Edited by Garner DM, Garfinkel PE. New York, Guilford Press, 1997, pp 372-382Google Scholar
10. Steinhausen HC, Glanville K: Follow-up studies of anorexia nervosa—a review of research findings (editorial). Psychol Med 1983; 3:239-249Crossref, Google Scholar
11. Kay DW: Anorexia nervosa: a study in prognosis. Proc R Soc Med 1953; 46:669-674Medline, Google Scholar
12. Beck JC, Brøchner-Mortensen K: Observations on the prognosis in anorexia nervosa. Acta Med Scand 1954; 149:409-430Crossref, Medline, Google Scholar
13. Williams E: Anorexia nervosa: a somatic disorder. Br Med J 1958; 2:190-195Crossref, Medline, Google Scholar
14. Lesser LI, Ashenden BJ, Debushey M, Eisenberg L: Anorexia nervosa in children. Am J Orthopsychiatry 1960; 30:572-580Crossref, Medline, Google Scholar
15. Thomä H: Anorexia Nervosa. Bern, Switzerland, Huber, 1961Google Scholar
16. Blitzer JR, Rollins N, Blackwell A: Children who starve themselves: anorexia nervosa. Psychosom Med 1961; 23:369-383Crossref, Medline, Google Scholar
17. Meyer JE: Das Syndrom der Anorexia nervosa: Katamnestische Untersuchungen. Arch Psychiatr Nervenkr 1961; 202:31-59Crossref, Google Scholar
18. Tolstrup K: Die Charakteristika der jüngeren Fälle von Anorexia nervosa, in Anorexia Nervosa. Edited by Meyer JE, Feldmann H. Stuttgart, Germany, Thieme, 1965, pp 51-59Google Scholar
19. Frahm H: Ergebnisse einer systematisch durchgeführten somatisch orientierten Behandlungsform bei Kranken mit Anorexia nervosa. Ibid, pp 64-70Google Scholar
20. Frazier SH: Anorexia nervosa. Dis Nerv Syst 1965; 26:155-159Medline, Google Scholar
21. Kay DW, Shapira K: The prognosis in anorexia nervosa, in Anorexia Nervosa. Edited by Meyer JE, Feldman H. Stuttgart, Germany, Thieme, 1965, pp 113-127Google Scholar
22. Crisp AH: Some aspects of the evolution, presentation and follow-up of anorexia nervosa. Proc R Soc Med 1965; 58:814-820Medline, Google Scholar
23. Farquharson RF, Hyland HH: Anorexia nervosa: the course of 15 patients treated from 20 to 30 years previously. Can Med Assoc J 1966; 96:411-419Google Scholar
24. Dally PJ, Sargant W: Treatment and outcome of anorexia nervosa. Br Med J 1966; 2:793-795Crossref, Medline, Google Scholar
25. Warren W: A study of anorexia nervosa in young girls. J Child Psychol Psychiatry 1968; 9:27-40Crossref, Medline, Google Scholar
26. Seidensticker J, Tzagournis M: Anorexia nervosa—clinical features and long-term follow-up. J Chronic Dis 1980; 21:366-367Google Scholar
27. Browning CH, Miller SI: Anorexia nervosa: a study in prognosis and management. Am J Psychiatry 1968; 124:1128-1132Link, Google Scholar
28. Ziegler R, Sours J: A naturalistic study of patients with anorexia nervosa admitted to a university medical center. Compr Psychiatry 1968; 9:644-651Crossref, Medline, Google Scholar
29. Dally PJ: Anorexia Nervosa. London, Heinemann Medical Books, 1969Google Scholar
30. Theander S: Anorexia nervosa: a psychiatric investigation of 94 female patients. Acta Psychiatr Scand Suppl 1970; 214:1-194Medline, Google Scholar
31. Valanne EH, Taipale V, Larkio-Miettinen AK, Morén R, Aukee M: Anorexia nervosa: a follow-up study. Psychiatria Fennica 1972, pp 265-269Google Scholar
32. Halmi KA, Brodland G, Loney J: Prognosis in anorexia nervosa. Ann Intern Med 1973; 78:907-909Crossref, Medline, Google Scholar
33. Bruch H: Outcome and outlook, in Eating Disorders. Edited by Bruch H. New York, Basic Books, 1973, pp 377-387Google Scholar
34. Bhanji S, Thompson J: Operant conditioning in the treatment of anorexia nervosa. Br J Psychiatry 1974; 124:166-172Crossref, Medline, Google Scholar
35. Niskanen P, Jääskeläinen J, Achté K: Anorexia nervosa: treatment results and prognosis. Psychiatria Fennica 1974, pp 257-263Google Scholar
36. Silverman JA: Anorexia nervosa: clinical observations in a successful treatment plan. J Pediatr 1974; 84:68-73Crossref, Medline, Google Scholar
37. Morgan HG, Russell GFM: Value of family background and clinical features as predictors of long-term outcome in anorexia nervosa: four-year follow-up study of 41 patients. Psychol Med 1975; 5:355-371Crossref, Medline, Google Scholar
38. Brady JP, Rieger W: Behavioral treatment of anorexia nervosa, in Applications of Behavior Modification. Edited by Thompson T, Dockens WS III. New York, Academic Press, 1961, pp 45-63Google Scholar
39. Pierloot RA, Wellens W, Houben ME: Elements of resistance to a combined medical and psychotherapeutic program in anorexia nervosa. Psychother Psychosom 1975; 26:101-117Crossref, Medline, Google Scholar
40. Niederhoff H, Wiesler B, Kuenzer W: Somatisch orientierte Behandlung der Anorexia nervosa. Monatsschr Kinderheilkd 1975; 123:343-344Medline, Google Scholar
41. Beumont PJV, George GCW, Smart DE: “Dieters” and “vomiters and purgers” in anorexia nervosa. Psychol Med 1976; 6:617-622Crossref, Medline, Google Scholar
42. Halmi KA, Brodland G, Rigas C: A follow-up study of seventy-nine patients with anorexia nervosa: an evaluation of prognostic factors and diagnostic criteria, in Life History Research in Psychopathology, vol 4. Edited by Winokur G, Roff M, Wirt RD. Minneapolis, University of Minnesota Press, 1976, pp 290-300Google Scholar
43. Willi J, Hagemann R: Langzeitverläufe von Anorexia nervosa. Schweizerische Med Wochenschrift 1976; 106:1459-1465Medline, Google Scholar
44. Rosman BL, Minuchin S, Liebman R, Baker L: Input and outcome of family therapy in anorexia nervosa, in Successful Psychotherapy. Edited by Claghorn JL. New York, Brunner/Mazel, 1976, pp 128-139Google Scholar
45. Goetz PL, Succop RA, Reinhart JB, Miller A: Anorexia nervosa in children: a follow-up study. Am J Orthopsychiatry 1977; 47:597-603Crossref, Medline, Google Scholar
46. Sturzenberger S, Cantwell PD, Burroughs J, Salkin B, Green JK: A follow-up study of adolescent psychiatric inpatients with anorexia nervosa. J Am Acad Child Psychiatry 1977; 16:703-715Crossref, Medline, Google Scholar
47. Cantwell DP, Sturzenberger S, Burroughs J, Salkin B, Green J: Anorexia nervosa—an affective disorder? Arch Gen Psychiatry 1977; 34:1087-1093Crossref, Medline, Google Scholar
48. Stonehill E, Crisp AH: Psychoneurotic characteristics of patients with anorexia nervosa before and after treatment and at follow-up 4-7 years later. J Psychosom Res 1977; 16:703-715Google Scholar
49. Garfinkel PE, Moldofsky H, Garner DM: The outcome of anorexia nervosa: significance of clinical features, body image and behavior modification, in Anorexia Nervosa. Edited by Vigersky RA. New York, Raven Press, 1977, pp 315-329Google Scholar
50. Pertschuk MJ: Behavior therapy: extended follow-up. Ibid, pp 305-314Google Scholar
51. Cremerius J: Zur Prognose der Anorexia nervosa. Z Psychosom Med Psychoanal 1978; 24:56-69Medline, Google Scholar
52. Ziolko HU: Zur Katamnese der Pubertätsmagersucht. Arch Psychiatr Nervenkr 1978; 225:117-125Crossref, Medline, Google Scholar
53. Petzold E: Familienkonfrontationstherapie bei Anorexia nervosa. Göttingen, Germany, Verlag für medizinische Psychologie Dr CJ Hogrefe, 1979Google Scholar
54. Hsu LKG, Crisp AH, Harding B: Outcome of anorexia nervosa. Lancet 1979; 1:61-65Crossref, Medline, Google Scholar
55. Schütze G: Anorexia Nervosa. Bern, Switzerland, Huber, 1980Google Scholar
56. Rollins N, Piazza E: Anorexia nervosa: a qualitative approach to follow-up. J Am Acad Child Psychiatry 1981; 20:167-183Crossref, Medline, Google Scholar
57. Steinhausen HC, Rauss-Mason C, Seidel R: Follow-up studies of anorexia nervosa: a review of four decades of outcome research. Psychol Med 1991; 21:447-454Crossref, Medline, Google Scholar
58. Becker H, Körner P, Stöffler A: Psychodynamics and therapeutic aspects of anorexia nervosa: a study of family dynamics and prognosis. Psychother Psychosom 1981; 36:8-16Crossref, Medline, Google Scholar
59. Bassøe HH, Eskeland I: A prospective study of 133 patients with anorexia nervosa—treatment and outcome. Acta Psychiatr Scand 1982; 65:127-133Crossref, Medline, Google Scholar
60. Kohle K, Mall H: Follow-up study of 36 anorexia nervosa patients treated on an integrated internistic-psychosomatic ward. Int J Eat Disord 1983; 2:215-219Crossref, Google Scholar
61. Colligan RC, Ferdinande RJ, Lucas AR, Duncan JW: A one-year follow-up study of adolescent patients hospitalized with anorexia nervosa. J Dev Behav Pediatr 1983; 4:278-279Crossref, Medline, Google Scholar
62. Morgan HG, Purgold J, Welbourne J: Management and outcome in anorexia nervosa—a standardized prognostic study. Br J Psychiatry 1983; 143:282-287Crossref, Medline, Google Scholar
63. Steinhausen HC, Glanville K: Retrospective and prospective follow-up of adolescent anorexia nervosa. Acta Psychiatr Scand 1983; 68:1-10Crossref, Medline, Google Scholar
64. Hall A, Slim E, Hawker F, Salmond C: Anorexia nervosa—long-term outcome in 50 female patients. Br J Psychiatry 1984; 145:407-413Crossref, Medline, Google Scholar
65. Burns T, Crisp AH: Outcome of anorexia nervosa in males. Br J Psychiatry 1984; 145:319-325Crossref, Medline, Google Scholar
66. Touyz SW, Beumont PJV: Anorexia nervosa: a follow-up investigation. Med J Aust 1984; 141:219-222Crossref, Medline, Google Scholar
67. Nussbaum M, Shenker IR, Baird D, Saravay S: Follow-up investigation in patients with anorexia nervosa. J Pediatr 1985; 106:835-840Crossref, Medline, Google Scholar
68. Tolstrup K, Brinch M, Isager T, Nielsen S, Nystrup J, Severin B, Olesen NS: Long-term outcome of 151 cases of anorexia nervosa. Acta Psychiatr Scand 1985; 71:380-387Crossref, Medline, Google Scholar
69. Martin FE: The treatment and outcome of anorexia nervosa in adolescents: a prospective study and five-year follow-up. J Psychiatr Res 1985; 19:509-514Crossref, Medline, Google Scholar
70. Theander S: Outcome and prognosis in anorexia nervosa and bulimia: some results of previous investigations, compared with those of a Swedish long-term study. J Psychiatr Res 1985; 19:493-508Crossref, Medline, Google Scholar
71. Suematsu H, Kuboki T, Itoh T: Statistical studies on the prognosis of anorexia nervosa. Psychother Psychosom 1985; 43:104-112Crossref, Medline, Google Scholar
72. Hawley RM: The outcome of anorexia nervosa in younger subjects. Br J Psychiatry 1985; 146:657-660Crossref, Medline, Google Scholar
73. Toner BB, Garfield PE, Garner DM: Long-term follow-up of anorexia nervosa. Psychosom Med 1986; 48:520-529Crossref, Medline, Google Scholar
74. Santonastaso P, Favaretto G, Canton G: Anorexia nervosa in Italy: clinical features and outcome in a long-term follow-up study. Psychopathology 1987; 20:8-17Crossref, Medline, Google Scholar
75. Engel K: Prognostic factors in anorexia nervosa. Psychother Psychosom 1988; 49:137-144Crossref, Medline, Google Scholar
76. Engel K, Wilfarth B: Therapy results and follow-up of an integrated treatment for severe cases of anorexia nervosa. Psychother Psychosom 1988; 50:5-14Crossref, Medline, Google Scholar
77. Remschmidt H, Wienand F, Wewetzer C: Der Langzeitverlauf der Anorexia nervosa. Monatsschr Kinderheilkd 1988; 136:726-731Medline, Google Scholar
78. Bryant-Waugh R, Knibbs J, Fosson A, Kaminski Z, Lask B: Long-term follow-up of patients with early onset anorexia nervosa. Arch Dis Child 1988; 63:5-9Crossref, Medline, Google Scholar
79. Deter HC, Petzold E, Hehl FJ: Differenzierung der Langzeitwirkungen einer stationären psychosomatischen Therapie von Anorexia-nervosa-Patienten. Z Psychosom Med 1989; 35:68-91Google Scholar
80. Willi J, Limacher B, Nussbaum P: Zehnjahres-Katamnese der 1973-75 im Kanton Zürich erstmals hospitalisierten Anorexien. Schweizerische Med Wochenschrift 1989; 119:147-159Google Scholar
81. Fichter MM, Quadflieg N: Comparative studies on the course of eating disorders in adolescents and adults: is age at onset a predictor of outcome? in Eating Disorders in Adolescence: Anorexia and Bulimia Nervosa. Edited by Steinhausen HC. New York, Walter De Gruyter, 1995, pp 301-337Google Scholar
82. Arroyo D, Tonkin R: Adolescents with bulimic and nonbulimic eating disorders. J Adolesc Health Care 1985; 6:21-24Crossref, Medline, Google Scholar
83. Calvo Sagardoy R, Fernandez Ashton A, Ayuso Mateos JL, Bayon Perez C, Santo-Domingo Carrasco J: Between 5 and 9 years follow-up in the treatment of anorexia nervosa. Psychother Psychosom 1989; 52:133-139Crossref, Medline, Google Scholar
84. Crisp AH, Callender JS, Halek C, Hsu LKG: Long-term mortality in anorexia nervosa: a 20-year follow-up of the St George’s and Aberdeen cohorts. Br J Psychiatry 1992; 161:104-107Crossref, Medline, Google Scholar
85. Deter HC, Herzog W, Petzold E: The Heidelberg-Mannheim study: long-term follow-up of anorexia nervosa patients at the University Medical Center—background and preliminary results, in The Course of Eating Disorders: Long-Term Follow-Up Studies of Anorexia and Bulimia Nervosa. Edited by Herzog W, Deter HC, Vandereycken W. Berlin, Springer, 1992, pp 71-84Google Scholar
86. Greenfeld DG, Anyan WR, Hobart M, Quinlan DM, Plantes M: Insight into illness and outcome in anorexia nervosa. Int J Eat Disord 1991; 10:101-109Crossref, Google Scholar
87. Higgs JF, Goodyer IM, Birch J: Anorexia nervosa and food avoidance emotional disorder. Arch Dis Child 1989; 64:346-351Crossref, Medline, Google Scholar
88. Jenkins ME: An outcome study of anorexia nervosa in an adolescent unit. J Adolesc 1987; 10:71-81Crossref, Medline, Google Scholar
89. Kreipe RE, Churchill BH, Strauss J: Long-term outcome of adolescents with anorexia nervosa. Am J Dis Child 1989; 143:1322-1327Medline, Google Scholar
90. Ratnasuriya RH, Eisler I, Szmukler GI, Russell GFM: Anorexia nervosa: outcome and prognostic factors after 20 years. Br J Psychiatry 1991; 158:465-502Crossref, Google Scholar
91. Rosenvinge JH, Mouland SO: Outcome and prognosis of anorexia nervosa: a retrospective study of 41 subjects. Br J Psychiatry 1990; 156:92-97Crossref, Medline, Google Scholar
92. Santonastaso P, Pantano M, Panarotto L, Silvestri A: A follow-up study on anorexia nervosa: clinical features and diagnostic outcome. Eur Psychiatry 1991; 6:177-185Google Scholar
93. Steiner H, Mazer C, Litt IF: Compliance and outcome in anorexia nervosa. West J Med 1990; 157:133-139Google Scholar
94. Steinhausen HC, Seidel R: Outcome in adolescent eating disorders. Int J Eat Disord 1993; 14:487-496Crossref, Medline, Google Scholar
95. Walford G, McCune N: Long-term outcome in early-onset anorexia nervosa. Br J Psychiatry 1991; 159:383-389Crossref, Medline, Google Scholar
96. Fichter MM, Quadflieg N, Rief W: The German Longitudinal Bulimia Nervosa Study I, in The Course of Eating Disorders: Long-Term Follow-Up Studies of Anorexia and Bulimia Nervosa. Edited by Herzog W, Deter HC, Vandereycken W. Berlin, Springer, 1992, pp 133-149Google Scholar
97. Herzog DB, Sacks NR, Keller MB, Lavori PW, Ranson KB, Gray HM: Patterns and predictors of recovery in anorexia nervosa and bulimia nervosa. J Am Acad Child Adolesc Psychiatry 1993; 32:835-842Crossref, Medline, Google Scholar
98. Vandereycken W, Pieters G: A large-scale longitudinal follow-up study of patients with eating disorders: methodological issues and preliminary results, in The Course of Eating Disorders: Long-Term Follow-Up Studies of Anorexia and Bulimia Nervosa. Edited by Herzog W, Deter HC, Vandereycken W. Berlin, Springer, 1992, pp 182-197Google Scholar
99. Norring CEA, Sohlberg SS: Outcome, recovery, relapse and mortality across six years in patients with clinical eating disorders. Acta Psychiatr Scand 1993; 87:437-444Crossref, Medline, Google Scholar
100. Smith C, Feldman SS, Nasserbakht A, Steiner H: Psychological characteristics and DSM-III-R diagnoses at 6-year follow-up of adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry 1993; 32:1237-1245Crossref, Medline, Google Scholar
101. Deter HC, Herzog W: Anorexia nervosa in a long-term perspective: results of the Heidelberg-Mannheim Study. Psychosom Med 1994; 56:20-27Crossref, Medline, Google Scholar
102. van der Ham T, van Strien DC, van Engeland H: A four-year prospective follow-study of 49 eating-disordered adolescents: differences in course of illness. Acta Psychiatr Scand 1994; 90:229-235Crossref, Medline, Google Scholar
103. Wonderlich SA, Fullerton D, Swift WJ, Klein MH: 5-year outcome from eating disorders—relevance of personality disorders. Int J Eat Disord 1994; 15:233-244Crossref, Medline, Google Scholar
104. Gillberg C, Råstam M, Gillberg IC: Anorexia nervosa 6 years after onset, 1: personality disorders. Compr Psychiatry 1995; 36:61-69Crossref, Medline, Google Scholar
105. Eckert ED, Halmi KA, Marchi P, Grove W, Crosby R: Ten-year follow-up of anorexia nervosa: clinical course and outcome. Psychol Med 1995; 25:143-156Crossref, Medline, Google Scholar
106. Herpertz-Dahlmann BM, Wewetzer C, Schulz E, Remschmidt H: Course and outcome in adolescent anorexia nervosa. Int J Eat Disord 1996; 19:335-345Crossref, Medline, Google Scholar
107. Theander S: Anorexia nervosa with an early onset: selection, gender, outcome, and results of a long-term follow-up study. J Youth Adolesc 1996; 25:419-429Crossref, Google Scholar
108. Bryant-Waugh R, Hankins M, Shafran R, Lask B, Fosson A: A prospective follow-up of children with anorexia nervosa. J Youth Adolesc 1996; 25:431-437Crossref, Google Scholar
109. Steinhausen HC, Boyadjieva S: The outcome of adolescent anorexia nervosa: findings from Berlin and Sofia. J Youth Adolesc 1996; 25:473-481Crossref, Google Scholar
110. Kreipe RE, Piver Dukam C: Outcome of anorexia nervosa related to treatment utilizing an adolescent medicine approach. J Youth Adolesc 1996; 25:483-497Crossref, Google Scholar
111. Casper RC, Jabine LN: An eight-year follow-up: outcome from adolescent compared to adult-onset anorexia nervosa. J Youth Adolesc 1996; 25:499-517Crossref, Google Scholar
112. Sunday SR, Reeman IM, Eckert E, Halmi KA: Ten-year outcome in adolescent onset anorexia nervosa. J Youth Adolesc 1996; 25:533-544Crossref, Google Scholar
113. Fichter MM, Quadflieg N: Course and two-year outcome in anorexic and bulimic adolescents. J Youth Adolesc 1996; 25:545-562Crossref, Google Scholar
114. North C, Growers S, Byram V: Family functioning and life events in the outcome of adolescent anorexia nervosa. Br J Psychiatry 1997; 171:545-549Crossref, Medline, Google Scholar
115. Schulze U, Neudörfli A, Krill A, Warnke A, Remschmidt H, Herpertz-Dahlmann B: Verlauf und Heilungserfolg der frühen Anorexia nervosa. Z Kinder Jugendpsychiatr 1997; 25:5-16Google Scholar
116. Strober M, Freeman R, Morrell W: The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10-15 years in a prospective study. Int J Eat Disord 1997; 22:339-360Crossref, Medline, Google Scholar
117. Finzer P, Haffner J, Müller-Küppers M: Zu Verlauf und Prognose der Anorexia nervosa: Katamnese von 41 Patienten. Prax Kinderpsychol Kinderpsychiatr 1998; 47:302-313Medline, Google Scholar
118. Thiel A, Züger M, Jacoby GE, Schüssler G: Thirty-month outcome in patients with anorexia or bulimia nervosa and concomitant obsessive-compulsive disorder. Am J Psychiatry 1998; 155:244-249Abstract, Google Scholar
119. Sullivan PF, Bulik CM, Fear JL, Pickering A: Outcome of anorexia nervosa: a case-control study. Am J Psychiatry 1998; 155:939-946Link, Google Scholar
120. Saccomani L, Savoini M, Cirrincione M, Ravera G: Long-term outcome of children and adolescents with anorexia nervosa: study of comorbidity. J Psychosom Res 1998; 44:565-571Crossref, Medline, Google Scholar
121. Deter HC, Köpp W, Zipfel S, Herzog W: Männliche Anorexia-nervosa-Patienten im Langzeitverlauf. Nervenarzt 1998; 69:419-426Crossref, Medline, Google Scholar
122. Jarman FC, Rickards WS, Hudson L: Late adolescent outcome of early-onset anorexia nervosa. J Paediatr Child Health 1991; 27:221-227Crossref, Medline, Google Scholar
123. Fichter MM, Quadlieg N: Six-year course and outcome of anorexia nervosa. Int J Eat Disord 1999; 26:359-385Crossref, Medline, Google Scholar
124. Pla C, Toro J: Anorexia nervosa in a Spanish adolescent sample: an 8-year longitudinal study. Acta Psychiatr Scand 1999; 100:441-446Crossref, Medline, Google Scholar
125. Wentz Nilsson E, Gillberg C, Gillberg IC, Råstam M: Ten-year follow-up of adolescent-onset anorexia nervosa: personality disorders. J Am Acad Child Adolesc Psychiatry 1999; 38:1389-1395Crossref, Medline, Google Scholar
126. Steinhausen HC: Eating disorders, in Risks and Outcomes in Developmental Psychopathology. Edited by Steinhausen HC, Verhulst F. Oxford, UK, Oxford University Press, 1999, pp 210-330Google Scholar
127. Sohlberg S, Norring C, Holmaren S, Rosmark B: Impulsivity and long-term prognosis of psychiatric patients with anorexia nervosa/bulimia nervosa. J Nerv Ment Dis 1989; 177:249-258Crossref, Medline, Google Scholar
128. Crisp AH, Harding G, McGuiness B: Anorexia nervosa: psychoneurotic characteristics of parents: relationship to prognosis. J Psychosom Res 1974; 18:167-173Crossref, Medline, Google Scholar
129. Kalucy RS, Crisp AH, Harding B: A study of 56 families with anorexia nervosa. Br J Med Psychol 1977; 50:381-395Crossref, Medline, Google Scholar
130. Rollins N, Blackwell A: The treatment of anorexia nervosa in children and adolescents: stage 1. J Child Psychol Psychiatry 1968; 9:81-91Crossref, Medline, Google Scholar
131. Herzog DB, Dorer DJ, Keel PK, Selwyn SE, Ekeblad ER, Flores A, Greenwood DN, Burwell RA, Keller MB: Recovery and relapse in anorexia and bulimia nervosa: a 7.5-year follow-up study. J Am Acad Child Adolesc Psychiatry 1999; 38:829-837Crossref, Medline, Google Scholar
132. Feighner JP, Robins E, Guze SB, Woodruff RA Jr, Winokur G, Muñoz R: Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry 1972; 26:57-63Crossref, Medline, Google Scholar
133. Cohen J: Statistical Power Analysis for the Behavioral Sciences, revised ed. New York, Academic Press, 1977Google Scholar
134. Nielsen S, Møller-Madsen S, Isager T, Jørgensen J, Pagsberg K, Theander S: Standardized mortality in eating disorders—a quantitative summary of previously published and new evidence. J Psychosom Res 1998; 44:413-434Crossref, Medline, Google Scholar
135. Russell GFM: Anorexia nervosa of early onset and its impact on puberty, in Feeding Problems and Eating Disorders in Children and Adolescents. Edited by Cooper PJ, Stein A. Chur, Switzerland, Harwood Academic, 1992, pp 85-112Google Scholar
136. Steinhausen HC, Seidel R, Winkler Metzke C: Evaluation of treatment and intermediate and long-term outcome of adolescent eating disorder. Psychol Med 2000; 30:1089-1098Crossref, Medline, Google Scholar



