Suicide Attempts in Patients With Bipolar I Disorder During Acute and Maintenance Phases of Intensive Treatment With Pharmacotherapy and Adjunctive Psychotherapy
Abstract
OBJECTIVE: Lifetime rates of suicide attempts among patients with bipolar I disorder were compared to rates during a 2-year period of intensive treatment with pharmacotherapy and with one of two adjunctive psychosocial interventions. METHOD: Subjects entered the study during an acute mood episode. Subjects were treated with primarily lithium pharmacotherapy and with either psychotherapy specific to bipolar disorder, which included help in regularizing daily routines, or nonspecific, intensive clinical management involving regular visits with empathic clinicians. Data on prior suicide attempts were obtained retrospectively from interviews with the NIMH-Life-Chart method. Data on suicide attempts during the clinical trial were collected systematically throughout the protocol. RESULTS: The rate of suicide attempts was 1.05 per 100 person-months before patients entered the trial. Patients experienced a threefold reduction in the rate of suicide attempts during the acute treatment phase (until the patient achieved stabilization, defined by completion of 4 weeks during which the patient had a mean score of ≤7 on the 17-item Hamilton Depression Rating Scale and ≤7 on the Bech-Rafaelsen Mania Scale) and a 17.5-fold reduction during maintenance treatment. Poisson loglinear regression analysis modeling the relationship between the observed rates and the three protocol stages (pretreatment, acute, and maintenance) showed that the reductions were significant in the acute and maintenance phases, compared with the pretreatment phase. No patient with one or more suicide attempts before entering the trial attempted suicide during the protocol. CONCLUSIONS: A treatment program in a maximally supportive clinical environment can significantly reduce suicidal behavior in high-risk patients with bipolar I disorder.
No patient population is at greater risk of suicide-related morbidity and mortality than individuals suffering from bipolar disorder (1). An estimated 25% to 50% of all individuals with bipolar disorder will make a suicide attempt (2). The progressive, episodic, and chronic nature of bipolar depression poses a unique problem and dictates the need for a continuing clinical focus on suicidality not only during acute depressive episodes but also during preventive and maintenance clinical care.
Converging evidence from naturalistic studies has suggested the effectiveness of lithium prophylaxis in preventing suicide (3), and recent reports and reviews have confirmed this association (4–7). Upon discontinuation of lithium prophylaxis, the risk of suicide for an individual has been reported to increase 16-fold (8). However, one study found a significant reduction of suicide risk only when lithium was administered in concert with supportive care: without an adjunct educational and/or psychological treatment program, lithium evidenced no protection against suicide (9). Oquendo and Mann (10) have written recently about the importance of psychosocial factors in identifying and managing suicide risk in patients with bipolar disorder. However, to our knowledge, there are no data concerning the effects on suicidality of either more general psychosocial treatments or those that specifically target suicidality in bipolar disorder.
For much of the second half of the 20th century, psychosocial treatments were generally viewed as superfluous in the treatment of patients with bipolar I disorder. It is only within the last decade that serious efforts to develop and study manual-based psychosocial treatments for patients with bipolar I disorder have been undertaken (11–13). Yet, researchers have analyzed the efficacy of these interventions only for decreasing rates of syndromal recurrence and for improving psychosocial functioning. However, these psychosocial interventions may indirectly reduce suicide risk. The pertinacity of suicidality warrants further exploration.
We report on the effects of psychosocial treatment on rates of suicide attempts among 175 patients with bipolar I disorder who were followed for an average of 1.4 years. Most subjects described in this report were treated with lithium (N=166 of 175) during the study period. In addition, all subjects received one of two levels of psychosocial intervention described in the Method section.
Method
Subjects
The study group consisted of 175 patients with bipolar I disorder who entered the Maintenance Therapies in Bipolar Disorder program between August 15, 1991, and November 28, 2000 (14). Subjects were between age 18 and 65, met Research Diagnostic Criteria for bipolar I disorder or schizoaffective manic disorder, were experiencing an acute affective episode, and had a 17-item Hamilton Depression Rating Scale score ≥15 or a Bech-Rafaelsen Mania Scale (15) score ≥15. Exclusion criteria included rapid cycling bipolar disorder (four or more affective episodes per year), a lifetime diagnosis of schizophrenia or antisocial personality disorder, current drug or alcohol abuse (unless confined to affective episodes), and pregnancy.
Procedure
Subjects were treated acutely with a combination of pharmacotherapy and one of two levels of psychosocial intervention. Pharmacotherapy was guided by an algorithm, the ultimate goal of which was to enter the maximum possible number of patients into the maintenance treatment phase while they were receiving lithium alone. Subjects who could not tolerate lithium or who had medical conditions incompatible with its use (e.g., significant renal or cardiovascular disease) received divalproex or carbamazepine. Subjects were seen weekly in the acute treatment phase, biweekly for the first 3 months of the maintenance treatment phase, and then monthly for the remaining 21 months. Plasma lithium, divalproex, or carbamazepine concentrations were assessed at each visit.
In addition to receiving pharmacotherapy, subjects were randomly assigned to treatment with either interpersonal and social rhythm therapy or intensive clinical management, according to the protocol design (14). Interpersonal and social rhythm therapy is a psychotherapy specific to bipolar disorder that adds a component targeting regularity in social rhythm to interpersonal psychotherapy for unipolar depression. Patients address interpersonal problems as they relate to mood symptoms, learn to regularize their daily social routines (i.e., sleep-wake cycle, exercise habits, mealtimes), modify potential triggers of affective episodes, and address current interpersonal problems. Intensive clinical management, by contrast, is a nonspecific but active psychosocial intervention. It involves regular visits with an empathic clinician who provides psychoeducation, discusses symptoms, and helps the subject to manage medication side effects.
The overall clinic environment was structured to be attractive and attentive to patients’ needs and to encourage adherence to all aspects of the treatment protocol. Subjects were followed by therapist-physician teams consisting of experienced therapists and faculty psychiatrists. There was very little turnover in these treatment teams over the course of any individual subject’s study participation. The clinic maintained a 24-hour answering service that, at a minimum, put subjects in touch with a clinician associated with the protocol and, in most cases, with one or the other member of the subject’s own treatment team any time the patient called the clinic service. Every attempt was made to reschedule missed visits, and extra crisis sessions could be scheduled within the context of the protocol when clinicians were concerned about a patient’s clinical state.
Subjects were treated in the acute phase until stabilized (defined by completion of 4 weeks during which symptom scores averaged ≤7 on the 17-item Hamilton depression scale and ≤7 on the Bech-Rafaelsen Mania Scale) and then reassigned on a random basis to preventive maintenance treatment with either interpersonal and social rhythm therapy or intensive clinical management. In the preventive phase each subject continued the pharmacotherapy regimen that had led to stabilization during the acute phase. Barring a recurrence, pharmacotherapy remained unchanged throughout the 2-year maintenance phase of the study.
Data on prior suicide attempts were taken from NIMH-Life-Chart protocols (16) that were created by trained raters. In preparation for the Life-Chart interview, the rater summarized all material available from any prior medical charts, which were obtained at the time of the subject’s study entry. To improve subjects’ recall during the Life-Chart interview, individual time lines, marked by events likely to enhance recall—including birthdays, anniversaries, changes of residence or employment, etc., as well as events gleaned from review of patents’ earlier charts—were created from the onset of the subject’s bipolar illness to the date of the interview. Once the patient had responded to treatment of the index episode, the Life-Chart interview was scheduled. Subjects were queried in detail about the onset and offset of episodes, treatments received, hospitalizations, and life events (including suicide attempts) over the period of interest. Because of the importance of suicidal behavior in this population, querying on this topic was particularly careful. A suicide attempt was defined according to the model of Mann et al. (17) as a self-destructive act that was sufficiently serious to require medical evaluation and that was carried out with the intent to end one’s life. The length of the Life-Chart interviews varied depending on the length of the subject’s illness and the number of events reported, but typically lasted 3–6 hours. Longer interviews were divided into two and, sometimes, three sessions.
The University of Pittsburgh’s biomedical institutional review board approved all recruitment, assessment, and treatment procedures. All subjects who met inclusion and exclusion criteria provided written informed consent after receiving a complete description of the study and having an opportunity to ask questions.
Statistical Analyses
Weighted Poisson loglinear regression analysis (18) was used to model the relationship between the observed number of suicide attempts and the protocol stage (pretreatment, acute, maintenance). Analyses were conducted by using the GENLOG procedure of SPSS 10.0 (SPSS, Inc., Chicago) and the GENMOD procedure of SAS 8.0 (SAS Institute, Inc., Cary, N.C.).
Results
Ninety-eight women and 77 men participated in the study. The mean age was 35.1 years (SD=10.5) and the mean educational level 14.8 years (SD=1.9). Ninety percent (N=158) were European American, and 42.3% (N=74) were single, 36.0% (N=63) were married, 20.6% (N=36) were divorced or separated, and 1.1% (N=2) were widowed.
During the acute treatment phase, 92 patients (52.6%) were predominantly treated for depression, 40 (22.9%) for mania, and 43 (24.6%) for mixed or cycling episodes.
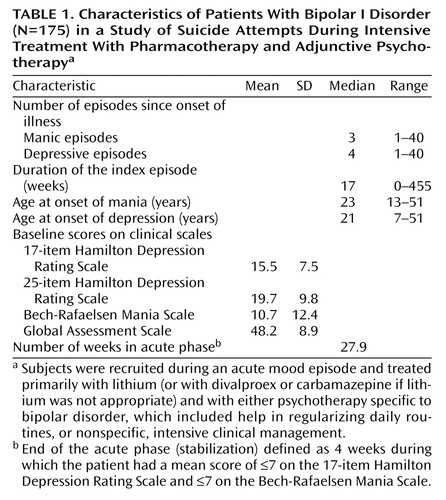
The clinical characteristics of the study subjects are reported in Table 1. Of the 175 patients, 166 (94.9%) were treated with lithium during the majority of the protocol. The mean plasma lithium level in these subjects was 0.83 meq/liter (SD=0.22, range=0.32–1.21).
We computed rates of prior suicide attempts beginning from the estimated date of onset of illness to the entry into acute treatment phase. The period considered for the calculation of the months at risk under treatment was between August 15, 1991 and December 5, 2000.
Seventy-two attempts were identified to have occurred before the patients entered the protocol. These 72 attempts occurred in 50 subjects, none of whom attempted suicide during the protocol. Eleven subjects reported making multiple attempts: six subjects reported two attempts, two reported three attempts, and three reported five attempts. Of these 72 attempts, five occurred in individuals who were taking lithium, seven in individuals taking antidepressants, one in an individual taking other psychotropic medications, and 44 in individuals who were not taking any medications for their mood disorder at the time of the attempt. Three attempts occurred in individuals who were receiving psychosocial treatment alone. For the remaining 12 attempts, Life-Chart data on the subject’s treatment were missing. Overall, four attempts occurred in subjects who were receiving both psychosocial treatment and medication.
Five suicide attempts occurred during the protocol, four during the acute treatment phase and one during the maintenance phase. At the time of the attempts, three of the patients were taking lithium, one had stopped taking lithium 2 days before the attempt, and one was taking divalproex. In the week before the attempt, three subjects were mildly to moderately depressed (Hamilton depression scale score between 14 and 27), one had low depression and mania ratings (Hamilton depression scale score=6, Bech-Rafaelsen Mania Scale score=0), and one patient had mixed symptoms, evidenced by relatively severe depression and mania ratings (on the day before the suicide attempt: Hamilton depression scale score=22, Bech-Rafaelsen Mania Scale score=21). At the time of the suicide attempt, four patients were receiving intensive clinical management in the acute phase and one was receiving interpersonal and social rhythm therapy in the maintenance phase.
Forty-seven subjects failed to complete the acute phase, and 20 failed to complete the maintenance phase. The reasons for study termination were termination against medical advice (N=35), failure to stabilize and/or intolerable side effects (N=16), termination with medical advice (N=4), and other reasons (e.g., moved out of town) (N=12).
In the entire subject group, a base rate of 1.05 attempts per 100 patient-months was computed for the period before study entry. During the acute phase, the rate of suicide attempts per 100 patient-months was 0.31, a threefold reduction in this short period relative to the period before entering the study. During the maintenance phase, the rate of attempts per 100 patient-months was 0.06 (a 17.5-fold reduction) (Figure 1). Using Poisson loglinear regression to model the relationship between the number of suicide attempts and the protocol stage (pretreatment, acute, maintenance), we found that these reductions were significant both in the acute (χ2=5.70, df=1, p<0.02) and in the maintenance phase (χ2=8.28, df=1, p=0.004), compared to the pretreatment phase. When we compared the rate of suicide attempts during the maintenance phase with the rate during the acute phase, the difference was not significant at the p<0.05 level. The mode-specific rates were 0.26 for patients receiving intensive clinical management and 0.07 for patients receiving interpersonal and social rhythm therapy, again with no significant difference. Overall, the rate was 0.17 during the protocol, corresponding to a six-fold reduction.
Discussion
The present attempt to examine the impact of psychosocial treatment and a maximally supportive clinic environment on the rate of suicide attempts in individuals with bipolar disorder is limited in several ways. We acknowledge that the study inclusion and exclusion criteria may have led to a selection bias favoring patients with less complicated forms of bipolar disorder. However, this limitation is somewhat mitigated by the fact that we examined each patient as his or her own comparison subject. A second limitation, while a very satisfying outcome from the standpoint of clinical care, is the low rate of suicide attempts during the protocol itself, which leads to low power for statistical analysis. This limitation is common to many studies, leading to a virtual absence of data on nonfatal suicidal behaviors, as claimed in a recent Cochrane review (19) on lithium effect for maintenance treatment of mood disorder. This lack of data made the authors conclude that “it is impossible to draw meaningful conclusions about the place of lithium therapy in suicide prevention” (19). Finally, it is possible that the Life-Chart method, which depended partially on subjects’ recall, could have underestimated the actual number of suicide attempts before study entry, failed to represent the lethality of attempts accurately, or in other ways biased these analyses. In point of fact, the majority of the attempts included in our analyses were well documented in medical charts, thus somewhat reducing the likelihood that they were improperly characterized.
We found a consistent reduction in suicide attempt risk associated with a combination of pharmacotherapy (mostly lithium) and either a highly structured psychosocial treatment designed specifically for individuals with bipolar I disorder or a more general supportive intervention offered in the context of a research clinic environment geared toward optimal care of patients with this condition. This reduction is more pronounced during the maintenance phase than during the acute phase. In their review of the results of 33 studies, yielding 13-fold lower rates of suicide and reported attempts during long-term lithium treatment than without it or after its discontinuation, Baldessarini et al. (4) suggested that the protection against suicide offered by lithium is substantial but incomplete and that the evaluation of alternative treatments is required. Our results provide preliminary evidence that intensive clinical management or psychotherapy add to the effect of lithium or other appropriate pharmacotherapy. Our study setting is unique in that patients were seen at least monthly, monitored for treatment adherence, traced if they miss appointments, received medications at no cost, and had access to a 24-hour on-call service operated by the clinic staff. Thus, the study allowed examination of the benefit of treatments in optimal conditions. Although the overall suicide risk during the protocol was low, it is noteworthy that four of the five suicide attempts observed occurred among subjects who were being followed with clinical management as opposed to interpersonal and social rhythm therapy, suggesting that disorder-specific psychotherapy may have effects on suicidal behavior over and above the protective effect of a highly supportive clinical milieu. It is important to underscore the potential role for suicide prevention when clinical trials are conducted in a structured clinical setting. Such clinical settings often provide a 24-hour emergency on-call system for patients and an ongoing “safety net” through attention of multiple staff members to each patient’s clinical state. Patients educated about early warning signs of an impending relapse can best take advantage of this clinical milieu. In short, we believe that study settings such as the one in which this clinical trial was carried out provide the first line of defense and that disorder-specific psychotherapy coupled with adequate pharmacological interventions provide the second line of defense. The ongoing NIMH-supported Systematic Treatment Enhancement Program in Bipolar Disorder (G. Sachs, personal communication, 2001) should provide additional information on this point in a study with adequate power to test this important question.
Even these preliminary data provide some evidence that it is possible to decrease the high risk of suicidal behavior associated with bipolar disorder through vigorous treatment. Should similar results occur in the Systematic Treatment Enhancement Program in Bipolar Disorder, the combined findings will provide a powerful argument for increased intensity of care for patients with bipolar I disorder.
 |
Received Aug. 8, 2001; revision received Feb. 2, 2002; accepted March 5, 2002. From the Department of Psychiatry, Western Psychiatric Institute and Clinic, University of Pittsburgh. Address reprint requests to Dr. Frank, Western Psychiatric Institute and Clinic, 3811 O’Hara St., Pittsburgh, PA 15213; [email protected] (e-mail). Supported by NIMH grants MH-29618 (Dr. Frank) and MH-30915 (Dr. Kupfer) and an unrestricted grant from Merck Laboratories (Dr. Frank). The authors thank Patty Houck for advice on SAS procedures for weighted Poisson regression.
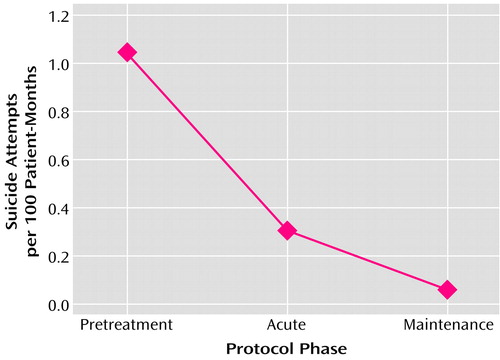
Figure 1. Rate of Suicide Attempts of Patients With Bipolar I Disorder (N=175) Before and During the Acute and Maintenance Phases of Intensive Treatment With Pharmacotherapy and Adjunctive Psychotherapya
aSubjects were recruited during an acute mood episode and treated primarily with lithium (or with divalproex or carbamazepine if lithium was not appropriate) and with either psychotherapy specific to bipolar disorder, which included help in regularizing daily routines, or nonspecific, intensive clinical management. The pretreatment phase extended from the onset of illness to the patient’s response to treatment of the index episode. The acute phase extended from after initial treatment response until the patient was stabilized (defined as 4 weeks of symptom scores averaging ≤7 on the 17-item Hamilton Depression Rating Scale and ≤7 on the Bech-Rafaelsen Mania Scale). During the maintenance phase, patients were randomly assigned to one of the two types of adjunctive psychotherapy, and the pharmacotherapy regimen that led to stabilization was continued.
1. Goodwin FK, Jamison KR: Suicide in Manic-Depressive Illness. New York, NY, Oxford University Press, 1990Google Scholar
2. Jamison KR: Suicide and bipolar disorder. J Clin Psychiatry 2000; 61(suppl 9):47-51Google Scholar
3. Schou M: Suicidal behavior and prophylactic lithium treatment of major mood disorders: a review of reviews. Suicide Life Threat Behav 2000; 30:289-293Medline, Google Scholar
4. Baldessarini RJ, Tondo L, Hennen J: Treating the suicidal patient with bipolar disorder: reducing suicide risk with lithium. Ann NY Acad Sci 2001; 932:24-38Crossref, Medline, Google Scholar
5. Tondo L, Hennen J, Baldessarini RJ: Lower suicide risk with long-term lithium treatment in major effective illness: a meta-analysis. Acta Psychiatr Scand 2001; 104:163-172Crossref, Medline, Google Scholar
6. Bowden CL: The ability of lithium and other mood stabilizers to decrease suicide risk and prevent relapse. Curr Psychiatry Rep 2000; 2:490-494Crossref, Medline, Google Scholar
7. Gelenberg AJ: Can lithium prevent suicide? Acta Psychiatr Scand 2001; 104:161-163Crossref, Medline, Google Scholar
8. Gallicchio V, Birch B (eds): Lithium: Biochemical and Clinical Advance. Cheshire, Conn, Weidner, 1996Google Scholar
9. Coppen A, Peet M, Bailey J, Noguera R, Burns BH, Swani MS, Maggs R, Gardner R: Double-blind and open prospective studies on lithium prophylaxis in affective disorders. Psychiatr Neurol Neurochir 1973; 76:501-510Medline, Google Scholar
10. Oquendo M, Mann JJ: Identifying and managing suicide risk in bipolar patients. J Clin Psychiatry 2001; 62 (suppl 25):31-34Google Scholar
11. Craighead WE, Miklowitz DJ, Vajk FC, Frank E: Psychosocial treatment in bipolar disorder, in A Guide to Treatments That Work. Edited by Nathan PE, Gorman JM. New York, Oxford University Press, 1998, pp 240-248Google Scholar
12. Frank E, Swartz HA, Kupfer DJ: Interpersonal and social rhythm therapy: managing the chaos of bipolar disorder. Biol Psychiatry 2000; 6:593-604Crossref, Google Scholar
13. Miklowitz DJ, Frank E: New psychotherapies for bipolar disorder, in Bipolar Disorder: Clinical Course and Outcome. Edited by Goldberg JF, Harrow M. Washington, DC, American Psychiatric Press, 1999, pp 57-84Google Scholar
14. Frank E, Hlastala S, Ritenour A, Houck P, Tu XM, Monk TM, Mallinger AG, Kupfer DJ: Inducing lifestyle regularity in recovering bipolar disorder patients: results from the maintenance therapies in bipolar disorder protocol. Biol Psychiatry 2000; 41:1165-1173Crossref, Google Scholar
15. Bech P, Bolwig TG, Kramp P, Rafaelsen OJ: The Bech-Rafaelsen Mania Scale and the Hamilton Depression Scale. Acta Psychiatr Scand 1979; 59:420-430Crossref, Medline, Google Scholar
16. Denicoff KD, Leverich GS, Nolen WA, Rush AJ, McElroy SL, Keck PE, Suppes T, Altshuler LL, Kupka R, Frye MA, Hatef J, Brotman MA, Post RM: Validation of the prospective NIMH-Life-Chart Method (NIMH-LCM-p) for longitudinal assessment of bipolar illness. Psychol Med 2000; 30:1391-1397Crossref, Medline, Google Scholar
17. Mann JJ, Waternaux C, Haas GL, Malone KM: Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 1999; 156:181-189Abstract, Google Scholar
18. Agresti A: Categorical Data Analysis. New York, John Wiley & Sons, 1990Google Scholar
19. Burgess S, Geddes J, Hawton K, Townsend E, Jamison K, Goodwin G: Lithium for maintenance treatment of mood disorders (Cochrane Review). Cochrane Database Syst Rev 2001; 3:CD003013Google Scholar



